Chapter 28 Noninvasive Respiratory Support
In this chapter, supplemental oxygen therapy, humidification systems, adjunctive respiratory therapy, and noninvasive ventilation (NIV) are discussed. NIV encompasses various methods of positive pressure ventilation, including continuous positive airway pressure (CPAP), delivered without an endotracheal tube.1
OXYGEN THERAPY
Oxygen delivery to the tissues depends on arterial oxygen content, cardiac output, and individual organ perfusion. Arterial oxygen content depends on the hemoglobin concentration and arterial oxygen saturation (Sao2; see Equation 1-13). The latter is, in turn, dependent on the oxyhemoglobin dissociation curve (see Fig. 1-14) and the arterial partial pressure of oxygen (Pao2) (see Chapter 1). Supplemental oxygen therapy is indicated to maintain the Pao2 above 8 κPa (60 mmHg) or the Sao2 above 90%. Only low concentrations of supplemental oxygen are required to treat hypoxemia due to hypoventilation. In contrast, high concentrations of oxygen may be required to treat hypoxemia due to ventilation/perfusion mismatch. Oxygen is ineffective if hypoxemia is due to pure shunt. High-concentration oxygen therapy in the setting of hypoventilation may mask the development of severe hypercarbia and respiratory acidosis (see Chapter 1).
Impaired gas exchange is almost universally present following cardiac and thoracic surgery, so oxygen is indicated for the duration of a patient’s stay in the intensive care unit (ICU). It should also be continued following discharge from the ICU if a patient is receiving opioid analgesia because that predisposes the patient to nocturnal desaturation.2 Supplemental oxygen therapy during the perioperative period has also been shown to reduce the incidence of surgical wound infections.3
Excessive oxygen therapy is not without risk. High-concentration oxygen promotes absorption atelectasis and, in patients with severe chronic obstructive pulmonary disease (COPD), it may exacerbate hypercarbia (see Chapter 27). Administration of high oxygen concentrations (FIo2 >0.6) for longer than several days may potentially cause direct pulmonary toxicity and should be avoided if possible.4 However, supplemental oxygen should not be withheld in the presence of clinically significant hypoxemia (Sao2 <85% to 90%).
Oxygen Delivery Systems
Variable-Performance Systems
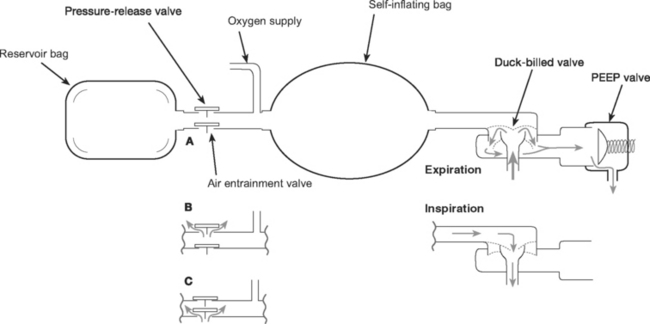
Manual Resuscitators.
The components of manual resuscitators (such as the Laerdal and the Ambu) are illustrated in Figure 28-1. As with other variableperformance systems, FIo2 depends on the oxygen flow, tidal volume, and respiratory rate, but it can be increased by attaching an oxygen reservoir bag to the air entrainment inlet. The resuscitation bag is designed for short-term emergency use when augmentation of a patient’s respiratory effort by manual ventilation is required. Care should be taken with a patient who has respiratory distress but good respiratory drive because spontaneous breathing through a manual resuscitator increases the work of breathing, potentially worsening the respiratory distress.
HUMIDIFICATION
Humidification Devices
Heat and Moisture Exchangers
Microbiologic filters have been developed that conserve the heat and moisture of the gas expired by a patient; they use them to heat and humidify the inspired gas delivered during the next breath. Modern heat and moisture exchangers are light in weight, low in resistance, and low in volume. They provide variable degrees of humidification (approximately 20 to 30 g/m3), that decrease with duration of use and high minute ventilation. Some may be effective for several days of continuous use. Heat and moisture exchangers should not be used with noninvasive ventilation because their resistance, although low, imposes increased work of breathing.
ADJUNCTIVE RESPIRATORY THERAPIES
Physical Therapy
Lung-expansion techniques duplicate the normal sigh breath (periodic voluntary hyperinflation), increasing end-inspiratory lung volume and reversing atelectasis. The most commonly used technique is incentive spirometry. This requires proper patient instruction and encouragement and should be done several times per hour, with a target tidal volume greater than 14 ml/kg.