A. Normal pattern
B. Stage 1 diastolic dysfunction (impaired relaxation)
C. Stage 2 diastolic dysfunction (pseudonormalization)
D. Stage 3 diastolic dysfunction (restrictive physiology)
E. Stage 4 diastolic dysfunction (extremely severe uncompensated irreversible restrictive physiology)
4. A patient has coarctation of the aorta. PW Doppler reveals a peak velocity of 2.0 m/s proximal to the coarctation. A continuous wave (CW) Doppler across the coarctation reveals a peak Doppler velocity of 4.0 m/s. What is the pressure gradient across the coarctation?
A. 8 mm Hg
B. 9 mm Hg
C. 36 mm Hg
D. 48 mm Hg
E. 64 mm Hg
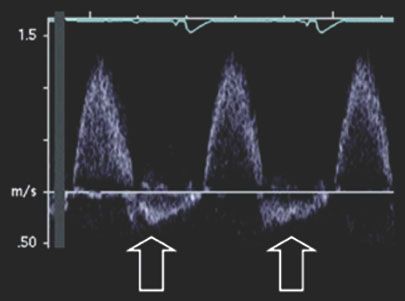
5. The Doppler tracing of the descending aorta in Figure 5.2. was obtained in a patient with suspected aortic regurgitation. What is the degree of regurgitation?
A. Unable to determine degree of regurgitation
B. Trivial
C. Mild (1+)
D. Moderate (2+)
E. Severe (4+)
6. Which of the following statements is correct concerning contrast echocardiography?
A. Contrast agents utilize microbubbles that are 50 to 100 microns in size
B. In the normal heart, contrast agents should opacify the right heart but not the left heart
C. Contrast agents can pass through the pulmonary circulation to opacify the left atrium and left ventricle
D. Acoustic impedance of contrast agents is higher than that of the blood pool
E. Contrast effect persists for 10 s to 15 s in the normal heart
7. Which of the following is correct concerning echocardiographic use of agitated saline injections?
A. Microbubbles are 1 to 10 microns in size and easily traverse the pulmonary bed to the left heart
B. In the presence of an intrapulmonary shunt, the majority of these bubbles appear in the left atrium within 1 to 2 cardiac cycles.
C. A negative bubble study (i.e., no bubbles imaged within the left heart) with agitated saline rules out a right-to-left shunt
D. Indications for agitated saline studies include unexplained cyanosis and stroke
E. Bubbles cannot be present in the left heart in the normal circulation without the presence of a left-to-right shunt
8. Which of the following is MOST helpful to diagnose the severity of aortic insufficiency?
A. Degree of LV dilatation
B. Length of the color Doppler regurgitant jet into the LV
C. Amount of diastolic Doppler flow reversal in the ascending aorta
D. Vena contracta width of the regurgitant jet
E. Comparison of the forward flow Doppler TVI to reverse flow TVI in the abdominal aorta
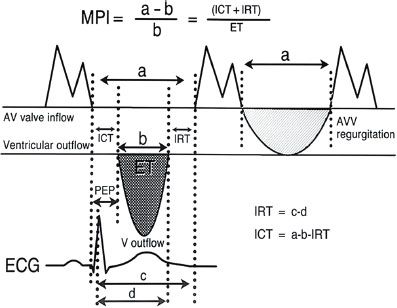
9. Which of the following formulas is correct for the myocardial performance index (i.e., TEI index):
A. [ICT + IRT] / ET
B. PEP / ET
C. E / Ea
D. [Pulmonary venous atrial reversal duration] – [mitral inflow atrial duration]
E. [LVEDD – LVESD] / LV ET
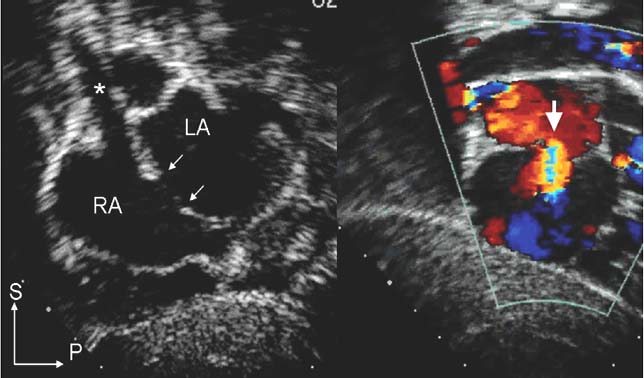
10. Which echocardiographic scan plane is most optimal to define a secundum atrial septal defect?
A. Suprasternal long-axis view
B. Parasternal long-axis view
C. Parasternal short-axis view
D. Subcostal four-chamber view
E. Apical four-chamber view
11. Which of the following is the most common associated cardiac defect found with a sinus venosus atrial septal defect?
A. Anomalous right pulmonary venous connection
B. Inlet ventricular septal defect
C. Bicuspid aortic valve
D. Persistent left superior vena cava
E. Coarctation of the aorta
12. Which of the following findings on echocardiography is consistent with constriction?
A. E/A ratio of mitral Doppler inflow <1.0
B. Decreased Ea velocity on tissue Doppler of the lateral mitral annulus
C. Increased respiratory variation in mitral inflow E-wave velocity >30%
D. Increased hepatic venous atrial systolic Doppler flow reversals during inspiration
E. Increased E-wave deceleration time on mitral inflow Doppler
13. Which of the following parameters is consistent with restrictive physiology?
A. Mitral inflow E/A Doppler ratio <1
B. Increased lateral mitral annular Ea velocity
C. Mitral inflow deceleration time <80 ms
D. Increased systolic / diastolic ratio of pulmonary venous Doppler
E. Lateral mitral annular E/Ea ratio <10
14. Which of the following associated congenital heart lesions is most common in a patient with Down syndrome and an atrioventricular septal defect (AVSD)?
A. Coarctation of the aorta
B. Total anomalous pulmonary venous connection
C. Aortic valve stenosis
D. Tetralogy of Fallot
E. Left ventricular hypoplasia
15. Which of the following is the most common anatomic finding in a complete AVSD?
A. Cleft in posterior leaflet of mitral component of AV valve
B. Medial rotation of left ventricular papillary muscles
C. Ratio of left ventricular inlet to outlet distance >1.0
D. Left ventricular outflow tract (LVOT) is “sprung” anteriorly
E. Left and right atrioventricular valve attachments are present at different levels
16. Which of the following statements is TRUE regarding M-mode?
A. Has a low PRF
B. Has excellent temporal resolution
C. X-axis represents distance from transducer
D. Y-axis represents time
E. Utilizes two imaging crystals to transmit and receive impulses
17. Which of the following statements regarding resolution in echocardiography is CORRECT?
A. Resolution is defined as the smallest distance between two points distinguishable as separate points
B. Axial resolution is the ability to differentiate points perpendicular to the ultrasound beam path
C. Lateral resolution is the ability to differentiate between points along the path of the ultrasound beam
D. Lateral resolution is better than axial resolution
E. Image resolution is best where the ultrasound beam is widest
18. Which of the following is the most likely source of error in calculation of Doppler flow velocity?
A. Angle of incidence of the ultrasound beam
B. Depth of the vascular structure
C. Frequency of the transducer
D. Presence and degree of imaging artifact
E. Variation in heart rate
19. Which of the following is true regarding CW Doppler?
A. Utilizes a single ultrasound crystal that continuously transmits and receives
B. No limit to maximal velocity measured
C. Excellent range resolution
D. Less dependent on angle of incidence compared to PW Doppler
E. Lower Nyquist limit compared to PW Doppler
20. Which of the following statements regarding PW Doppler is CORRECT?
A. Utilizes two ultrasound crystals that continuously transmit and receive
B. No limit to maximal velocity measured
C. Excellent range resolution
D. Lower PRF than color Doppler
E. PRF is fixed
21. Which of the following is a CORRECT statement regarding the Nyquist limit?
A. Represents the highest frequency shift that can be unambiguously detected and displayed
B. Is equal to the PRF
C. Is higher with PW Doppler versus CW Doppler
D. Remains the same with all transducer frequencies
E. Is lower at more shallow depths of interrogation
22. Which of the following is a TRUE statement regarding color Doppler?
A. Color Doppler represents the mean velocity of blood flow
B. Intensity of color represents peak Doppler flow velocity
C. 2D image content is unchanged with color Doppler imaging
D. Nyquist limit is increased with color Doppler imaging
E. Utilizes a single ultrasound beam with multiple sampling sites along that beam
23. Which of the following is the optimal echocardiographic view to delineate a subpulmonary ventricular septal defect?
A. Parasternal long-axis view
B. Apical four-chamber view
C. Suprasternal long-axis view
D. Parasternal short-axis view
E. Apical five-chamber view
24. Which of the following is the most characteristic acquired cardiac lesion resulting from a subpulmonary ventricular septal defect?
A. Aortic regurgitation
B. LVOT obstruction
C. Right ventricular outflow tract obstruction
D. Pulmonary valve stenosis
E. Aortic valve stenosis
25. Which of the following is the most characteristic physiologic effect of a large ventricular septal defect?
A. Right ventricular volume overload
B. Low pulmonary arterial pressure
C. Equal right ventricular and left ventricular systolic pressure
D. Increased systemic blood flow
E. Decreased pulmonary blood flow
26. Which of the following is the BEST morphologic marker of the right atrium?
A. Broad based triangular appendage
B. Receives superior vena cava
C. Chamber is connected to morphologic RV
D. Presence of septum primum
E. Connected to tricuspid valve
27. The atrial septum is BEST imaged in which scan plane?
A. Suprasternal
B. Subcostal
C. Parasternal long axis
D. Parasternal short axis
E. Apical four-chamber
28. Which of the following is a typical echocardiographic feature of the morphologic right ventricle?
A. Ellipsoid shape
B. More apical insertion point of atrioventricular valve
C. Smooth superior septal surface
D. Finely trabeculated apical portion
E. Lack of atrioventricular valve septal attachments
29. Which of the following is a typical echocardiographic feature of the morphologic left ventricle?
A. Heavily trabeculated inflow portion
B. Triangular shape
C. Trabeculated septal surface
D. Lack of atrioventricular valve septal chordal attachments
E. More apical insertion of atrioventricular valve
30. A neonate with pulmonary valve stenosis has a peak Doppler velocity by CW Doppler of 4.0 m/s. Which of the following is the estimated peak instantaneous Doppler gradient?
A. 64 mm Hg
B. 77 mm Hg
C. 72 mm Hg
D. 50 mm Hg
E. Cannot be calculated
31. Which of the following is the most common anatomic type of subaortic stenosis?
A. Tunnel type
B. Discrete membrane
C. Asymmetric septal hypertrophy
D. Systolic anterior motion of mitral valve
E. Anomalous mitral chordal insertion within the LVOT
32. The most common associated cardiac abnormality in the patient with coarctation of the aorta is?
A. Bicuspid aortic valve
B. Ventricular septal defect
C. Atrial septal defect
D. Pulmonary valve stenosis
E. Coronary artery anomaly
33. In patients with coarctation of the aorta, systemic arterial pressure begins to be significantly affected when the overall aortic lumen is narrowed by?
A. 20%
B. 30%
C. 50%
D. 75%
E. 90%
34. Which of the following is the most diagnostic echo finding in pericardial effusion with cardiac tamponade?
A. Diastolic right atrial wall collapse
B. 10% variation in mitral inflow Doppler velocities with respiration
C. Diastolic right ventricular wall collapse
D. Effusion >25 mm circumferentially
E. 15% variation in tricuspid inflow Doppler velocities with respiration
35. Which of the following methods of assessing LV systolic function is most independent of loading conditions?
A. Ejection fraction
B. Shortening fraction
C. Myocardial performance index
D. Rate corrected velocity of circumferential fiber shortening
E. Stress–velocity index
36. Normal left ventricular shortening fraction is maximal at which age?
A. 2-week old
B. 18-year old
C. 2-year old
D. 10-year old
E. No significant change in shortening fraction occurs with age
37. Holodiastolic Doppler flow reversal in the abdominal aorta can be attributed to which of the following?
A. Bidirectional cavopulmonary anastamosis
B. Large patent ductus arteriosus
C. Moderate aortic insufficiency
D. Sano shunt
E. High output state
38. Which of the following is the most common type of ventricular septal defect that is associated with coarctation of the aorta?
A. Apical muscular
B. Anterior malalignment
C. Perimembranous
D. Inlet
E. Subpumonary
39. The Doppler finding often seen in patients with supravalvar aortic stenosis has been demonstrated to be a high-velocity post-stenotic jet that hugs the aortic wall and preferentially transfers kinetic energy into the right innominate artery. Which of the following best describes this Doppler finding?
A. Coanda effect
B. Ohm’s law
C. Continuity equation
D. Poiseuille’s law
E. Bernoulli’s equation
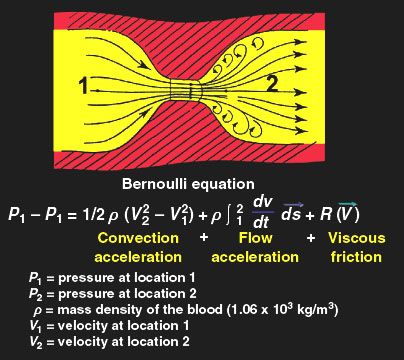
40. In the simplified Bernoulli equation, which component of the complete equation is not ignored?
A. Flow acceleration
B. Convective acceleration
C. Viscous friction
D. Proximal Doppler velocity
E. None are ignored
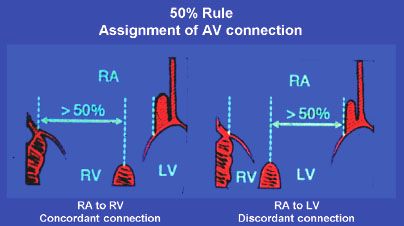
41. Which of the following is true about an overriding atrioventricular valve?
A. Has chordal attachments into both ventricles
B. Must have chordal attachments to the ventricular septal crest
C. Empties into two ventricles
D. Cannot coexist with straddling
E. Is never associated with malalignment type of VSD
42. Which of the following is true about a straddling cardiac valve?
A. Cannot coexist with overriding
B. Is always associated with malalignment type of VSD
C. Frequently involves the aortic valve
D. Is a common component of tetralogy of Fallot
E. Involves anomalous insertion of chordae tendinae
43. Which statement is correct regarding polysplenia syndrome?
A. The situs of abdominal viscera is always ambiguous
B. The spleen are multiple and located on both left and right sides
C. IVC fails to join the heart directly with azygos continuation
D. Multiple gallbladders common
E. Biliary atresia never occurs
44. Which statement is correct regarding the orientation of the great arteries?
A. A right-anterior aorta is most frequently associated with congenitally-corrected transposition of the great arteries (l-TGA)
B. A left-anterior aorta is most frequently associated with complete d-TGA
C. A right-posterior aorta is frequently found in double inlet left ventricle
D. A left-posterior aorta is commonly found in either type (l- or d-) of TGA
E. Normal hearts are characterized by a right-posterior aorta
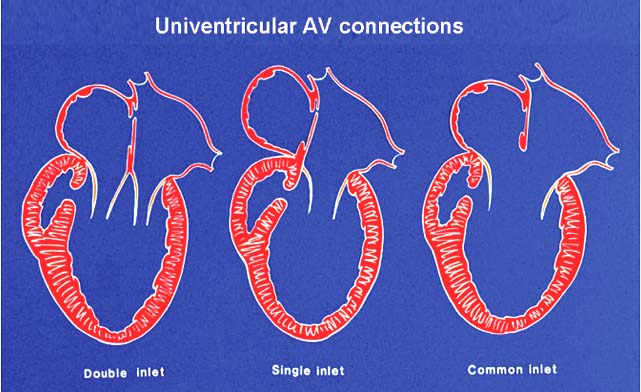
45. Tricuspid atresia is an example of which of the following?
A. Common inlet
B. Double inlet
C. Single inlet
D. Absent inlet
E. Ambiguous AV connection
46. Where does a type A interruption of the aortic arch occur?
A. Between the right innominate and left common carotid arteries
B. Proximal to the right innominate artery
C. Between the left common carotid and left subclavian arteries
D. Distal to the left subclavian artery
E. Just distal to the sinotubular junction in the ascending aorta
47. Which of the following statements is correct concerning venous return to the normal heart?
A. When the IVC is interrupted, venous return to the SVC is from the thebesian veins
B. When a persistent left SVC drains to a severely dilated coronary sinus, the brachiocephalic vein is typically small or absent
C. The connection of the right SVC to the right atrium confidently identifies the morphologic right atrium
D. It is more common for the right pulmonary veins than the left pulmonary veins to merge into a single vein that enters the left atrium
E. Interruption of the IVC is more common in asplenia versus polysplenia syndrome
48. Which of the following is the most reliable feature of the normal atrioventricular valve that distinguishes the mitral valve from the tricuspid valve?
A. Shape of the orifice
B. Atrioventricular valve—semilunar valve continuity
C. Presence of septal chordal attachments
D. Level of attachment of atrioventricular valve at cardiac crux
E. Number of leaflets
49. How many organ systems are characterized by situs or sidedness (i.e., these organ systems do NOT exhibit bilateral mirror image symmetry)?
A. 2
B. 3
C. 4
D. 5
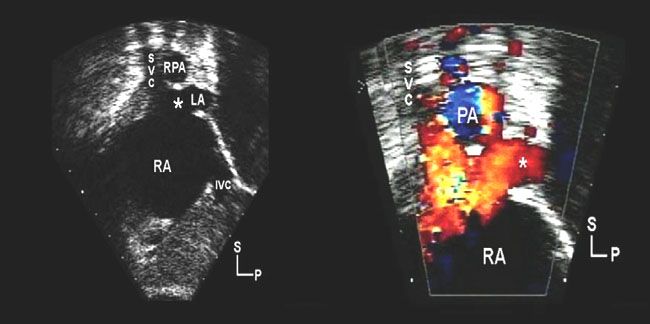
50. A 9-year-old patient presents with decreased exercise tolerance and cardiomegaly on chest x-ray. An echocardiogram was subsequently performed. What is the defect designated by the asterisk in Figure 5.3.?
A. Secundum atrial septal defect
B. Coronary sinus atrial septal defect
C. Sinus venosus atrial septal defect
D. Persistent left superior vena cava to unroofed coronary sinus
E. Primum atrial septal defect
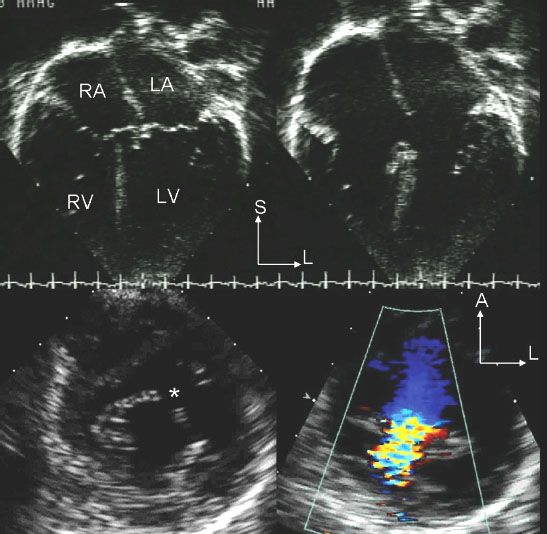
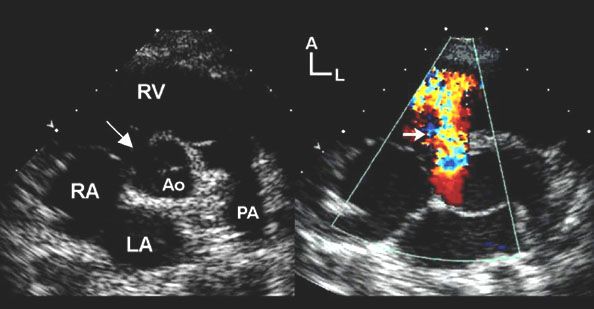
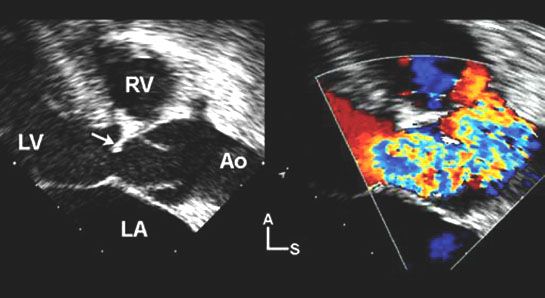
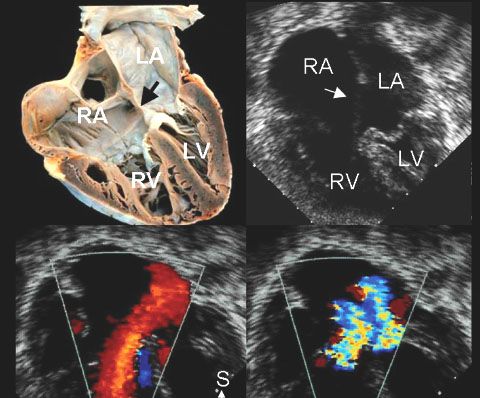
51. Which of the following congenital heart defects is demonstrated in Figure 5.4.?
A. Partial AVSD
B. Unroofed coronary sinus
C. Complete AVSD
D. Total anomalous pulmonary venous connection
E. Large inlet ventricular septal defect
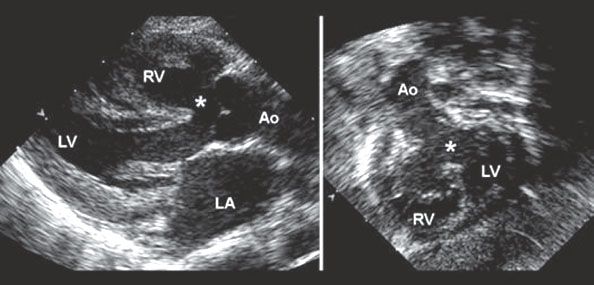
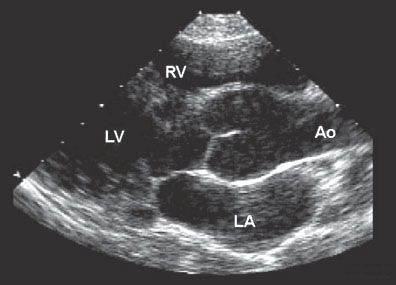
52. Which of the following congenital heart lesions is NOT consistent with the images in Figure 5.5.?
A. Tetralogy of Fallot
B. Pulmonary atresia with ventricular septal defect
C. Truncus arteriosus
D. Large malalignment ventricular septal defect
E. d-TGA
53. A 6-month-old child presents with failure to thrive and the echocardiographic image (Figure 5.6.) is obtained. What is the congenital heart defect demonstrated?
A. Muscular VSD
B. Membranous VSD
C. Infundibular VSD
D. Inlet VSD
E. Doubly committed VSD
54. Which of the following diagnoses is most consistent with the echocardiographic image in Figure 5.7.?
A. Down syndrome
B. DiGeorge syndrome
C. Marfan syndrome
D. Noonan syndrome
E. Williams syndrome
55. What is the most likely etiology of the echocardiographic image in Figure 5.8.?

A. Thrombus
B. Myxoma
C. Fibroma
D. Rhabdomyoma
E. Secondary metastasis
56. An 8-year-old patient has a resuscitated sudden cardiac death event while playing soccer. An echocardiogram performed in the emergency room displays the image in Figure 5.9. What is the most likely diagnosis?

A. Rhabdomyoma
B. Myxoma
C. Fibroma
D. Fibroelastoma
E. Sarcoma
57. Doppler flow studies in the human fetus have confirmed that the ratio of right-to-left ventricular combined output is about which of the following?
A. 10% / 90%
B. 25% / 75%
C. 55% / 45%
D. 25% / 75%
E. 90% / 10%
58. Fetal echocardiogram demonstrates fetal tachycardia. You and all your colleagues agree that the fetus has sustained VT and evidence of hydrops fetalis. The mother desires that “everything be done” for the fetus. The fetus is at 22 weeks gestation. What is your recommendation?
A. Give betamethasone immediately
B. Order anti-SSA/Ro and anti-SSA/La antibody panels and treat with prednisolone if positive
C. Start sotalol 80 mg PO BID
D. Load with digoxin 10 mcg IV
E. Observe only
59. Fetal four chamber view is inadequate to exclude which of the following congenital heart lesions?
A. AVSD
B. Hypoplastic left heart syndrome
C. Tricuspid atresia
D. d-TGA
E. Ebstein’s anomaly
60. What is the normal range for fetal cardio-thoracic area ratio?
A. <20%
B. 25% to 35%
C. 40% to 50%
D. 55% to 70%
E. >70%
61. What is the most common fetal arrhythmia?
A. Premature atrial contractions (PAC)
B. Premature ventricular contractions (PVC)
C. Supraventricular tachycardia (SVT)
D. Atrial flutter
E. Complete heart block
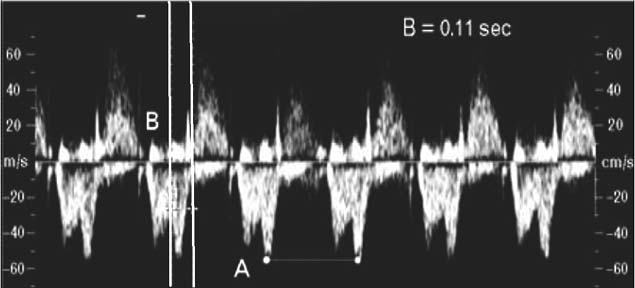
62. From the fetal Doppler interrogation in Figure 5.10., what interval is being measured between the parallel lines?
A. PP interval
B. RR interval
C. QT interval
D. PR interval
E. VA interval
63. While performing a fetal echocardiogram, you notice flow reversal across the ductus arteriosus. Which of the following defects is most likely to explain this finding?
A. TGA
B. AVSD
C. Critical aortic stenosis
D. Total anomalous pulmonary venous connection
E. Pulmonary atresia with intact ventricular septum
64. While performing a fetal echocardiogram, you notice retrograde flow into the aortic arch. Which of the following defects is most likely to explain this finding?
A. TGA
B. AVSD
C. Critical aortic valve stenosis
D. Total anomalous pulmonary venous connections
E. Pulmonary atresia with intact ventricular septum
65. The normal fetal heart rate ranges from which of the following?
A. 80 to 120 BPM
B. 60 to 100 BPM
C. 120 to 180 BPM
D. 140 to 220 BPM
E. 100 to 140 BPM
66. The normal fetal cardiac axis is between which of the following?
A. 30 and 60 degrees
B. 60 and 90 degrees
C. 90 and150 degrees
D. 60 and180 degrees
E. 0 and 90 degrees
67. What percentage of fetal cardiac output at term perfuses the lungs?
A. 10%
B. 30%
C. 50%
D. 75%
E. 100%
68. Match the fetal teratogen and its most commonly associated fetal congenital heart lesion:
A. Lithium 1. Ductal constriction
B. Fetal alcohol syndrome 2. VSD
C. Indomethocin 3. Coarctation of the aorta
D. Fetal hydantoin syndrome 4. Ebstein’s anomaly
E. Isotretinoin 5. d-TGA
69. Match the chromosomal anomaly with its most common congenital heart lesion:
A. Turner syndrome (XO) 1. Truncus arteriosus
B. DiGeorge syndrome (22q11-) 2. VSD
C. Trisomy 21 3. Coarctation of aorta
D. Trisomy 13 4. AVSD
E. William’s syndrome 5. Supravalvar aortic stenosis
70. Which of the following is least commonly associated with fetal bradycardia?
A. Maternal systemic lupus
B. Umbilical cord compression
C. Fetal heterotaxy syndrome
D. Fetal congenitally corrected TGA
E. Fetal tetralogy of Fallot
71. Which congenital heart lesion should be excluded in the fetus with SVT?
A. Ebstein’s anomaly
B. Ventricular septal defect
C. Coarctation of aorta
D. d-TGA
E. AVSD
72. Which of the following is the calculation for the pulsatility index (s = peak systolic Doppler velocity, d = minimum diastolic Doppler velocity) in the umbilical artery?
A.(s–d)/s
B.s/d
C.(s–d)/mean velocity
D.(s+d)/s
E.(s+d)/mean velocity
73. Which of the following is not a common echocardiographic sign of congestive heart failure in the fetus?
A. Abnormal umbilical venous Doppler
B. Mitral valve regurgitation
C. Increased pulsatility index in umbilical artery
D. Increased pulsatility index in middle cerebral artery
E. Tricuspid valve regurgitation
74. Which of the following fetal lesions would not be expected to have significant ventricular hypertrophy demonstrated in utero?
A. Recipient twin in twin-twin transfusion
B. Fetus of diabetic mother
C. Fetal hypertrophic cardiomyopathy (HCM)
D. Fetal tetralogy of Fallot
E. Fetal Noonan syndrome
75. A maternal etiology for congenital heart disease is insulin-dependent maternal diabetes. Which of the following statements regarding this referral for fetal echocardiography is false?
A. The incidence of congenital heart disease is lower than referrals with a family history of congenital heart disease
B. The most common cardiac lesions include d-TGA
C. A hemoglobin A1C above 8% predicts a high risk of congenital heart disease
D. The incidence of congenital heart disease is 3% to 7%
E. The cardiomyopathy is usually reversible
76. The presence of which of the following devices is a relative contraindication to performing a cardiac magnetic resonance imaging study?
A. Stainless steel vascular occluding coil
B. Hemostatic vascular clip
C. Temporary pacemaker lead without a generator
D. Amplatzer septal occluder
E. AICD
77. Which of the following devices would generate the most prominent imaging artifact with cardiac magnetic resonance imaging?
A. Amplatzer ASD device
B. Permanent pacemaker lead
C. Stainless steel PDA coil
D. Nonferromagnetic stent
E. PDA clip
78. Blood appears black on which cardiac magnetic resonance imaging technique?
A. Spin echo
B. Gradient echo cine MRI
C. Isotropic 3D steady-state free precession MRI
D. Cardiac-triggered, navigator-gated free-breathing 3D MRA
E. Contrast-enhanced 3-D MRA
79. For which of the following indications would cardiac magnetic resonance imaging most likely offer additional noninvasive diagnostic information compared to transthoracic echocardiography?
A. To quantitate left ventricular myocardial deformation
B. To quantitate atrioventricular valve regurgitation
C. To quantitate left ventricular diastolic dysfunction
D. To evaluate the size of the left-to-right shunt with a VSD
E. To evaluate pulmonary venous anatomy
80. Which of the following would be the optimal technique to calculate Qp:Qs by cardiac magnetic resonance imaging in a patient with a large secundum atrial septal defect?
A. Spatial modulation of magnetization (SPAMM)
B. Phase-velocity cine MR
C. Velocity-encoded cine (VEC) MR
D. Myocardial perfusion study
E. Spin echo cine MR
81. Which of the following is correct regarding the spin echo cardiac magnetic resonance imaging technique?
A. Produces bright blood images
B. Low tissue contrast
C. Images acquired during a single cardiac cycle
D. Facilitates optimal imaging of myocardial walls and cardiac tumors
E. Increased imaging artifact with metallic implants compared to other CMR techniques
82. Which of the following is characteristic of the “gradient echo” cardiac magnetic resonance imaging technique?
A. Produces bright blood images
B. Images take longer to acquire than “spin echo” technique
C. High tissue contrast
D. Relatively slow imaging speed compared to spin echo technique
E. Less imaging artifact with metallic implants compared to other CMR techniques
83. Which of the following is the best cardiac magnetic resonance technique to assess myocardial viability?
A. Myocardial delayed enhancement (MDE)
B. First-pass myocardial perfusion
C. Dobutamine stress CMR
D. ECG-gated VEC MRI sequence
E. SPAMM
Answers
1. ANSWER: C. PW Doppler utilizes one crystal that both emits and receives the sound pulses. The maximal frequency shift that can be determined by PW Doppler is equal to one-half the PRF and is termed the Nyquist limit. This Nyquist limit can be extended by using lower frequency transducers. High PRF lacks range gating resulting in range ambiguity.
2. ANSWER: A. The simplified Bernoulli equation ignores the components of flow acceleration and viscous friction. Doppler velocities across a patent ductus arteriosus or Blalock–Taussig shunt will likely be underestimated due to viscous friction in these tortuous connections and difficulties with proper ultrasound beam alignment. Multiple obstructions in series, such as multiple sites of LVOT obstruction (subvalvar, valvar, coarctation), will need to account for flow acceleration proximal to the distal site(s) of obstruction. Isolated valvar stenoses would be an appropriate use of the simplified Bernoulli equation.
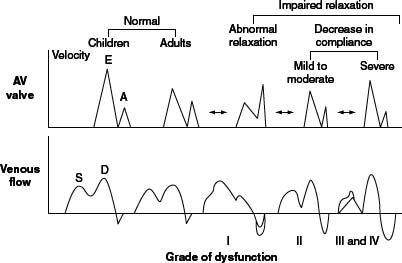
3. ANSWER: B. These Doppler patterns are consistent with impaired relaxation. Mitral inflow Doppler demonstrates an E:A ratio <1 while mitral annular tissue Doppler imaging also demonstrates a decreased early annular velocity and abnormal E’/A’ ratio <1. Pulmonary venous Doppler shows a systolic dominance and a prominent atrial reversal wave, consistent with grade I diastolic dysfunction (Fig. 5.11).
4. ANSWER: D. The pressure gradient can be predicted by using the “expanded” Bernoulli equation, P1 – P2 = 4 (V22 – V12), utilizing the Doppler velocities proximal and distal to the coarctation: 4 ([4.0]2 – [2.0]2) = 48 mm Hg.
5. ANSWER: E. The presence of holodiastolic flow reversal in the abdominal aorta is consistent with severe aortic regurgitation.
6. ANSWER: C. Contrast agents are designed to pass through the pulmonary capillary bed to opacify the left heart structures. The typical size of these microspheres is 1 to 10 microns. The acoustic impedance of contrast agents is much lower than that of the blood pool. The contrast effect persists for 3 min to 5 min with most contrast agents.
7. ANSWER: D. Microbubbles created with agitated saline range in size from 10 to 100 microns and do not pass through the pulmonary capillary bed. These microbubbles opacify the right atrium and right ventricle but not left heart structures in the absence of an intracardiac or intrapulmonary shunt. They can be helpful to identify an intracardiac right-to-left shunt that may be an etiology in stroke or unexplained cyanosis. In the presence of an intrapulmonary shunt the microbubbles typically appear in the left heart in 3 to 5 cardiac cycles compared to 1 to 2 cardiac cycles for an intracardiac shunt. A negative bubble study does not definitively exclude the presence of an intermittent right-to-left shunt.
8. ANSWER: D. The width of the regurgitant jet (vena contracta) and the ratio of the vena contracta dimension to the aortic annulus dimension are quantitative measures to grade aortic regurgitation. The degree of left ventricular dilatation is a semiquantitative measure and is most consistent with the duration of aortic regurgitation in addition to its severity. The length of the regurgitant jet into the left ventricle is influenced by many factors in addition to regurgitant severity including LV end diastolic pressure and eccentricity of the jet. The degree of Doppler flow reversal in the abdominal aorta is an excellent predictor of regurgitation degree as is the forward to reverse flow TVI in the transverse aortic arch.
9. ANSWER: A. The myocardial performance index (MPI) is a ratio of the total time spent in isovolumic activity (isovolumic contraction and isovolumic relaxation times) divided by the time spent in ventricular ejection (Fig. 5.12).
10. ANSWER: D. The subcostal imaging window is optimal to demonstrate the atrial septum and any associated atrial septal defects that may be present. To visualize the atrial septum without potential drop-out, the imaging plane of sound should be perpendicular to the cardiac structure of interest. With respect to the atrial septum, the imaging plane that is optimally perpendicular is the subcostal four-chamber and sagittal views. Atrial septal defects can be demonstrated in other imaging windows including the parasternal short axis, apical four-chamber, and high right parasternal views but care must be taken not to diagnose an atrial septal defect when the plane of sound is more parallel to the atrial septum creating the potential for false drop-out in the 2D image. The addition of color Doppler and spectral Doppler interrogation in these views will also facilitate the diagnosis of an atrial septal defect (Fig. 5.13).
11. ANSWER: A. Sinus venosus atrial septal defects are most commonly associated with anomalous connection of the right pulmonary veins. Either a single right upper pulmonary vein or the right upper and middle pulmonary veins insert anomalously to the superior vena cava or the SVC-right atrial junction. Sinus venosus defects are found most commonly in the superior portion of the atrial septum creating a “biatrial” insertion of the superior vena cava. These defects can also be located inferiorly near the entrance of the inferior vena cava into the right atrium.
12. ANSWER: C. Constrictive pericarditis is characterized by increased respiratory variation in mitral inflow Doppler velocities by >25%. Transmitral Doppler often demonstrates an increased E:A ratio and a shortened E-wave deceleration time. Lateral mitral tissue Doppler velocities are usually normal. Hepatic venous Doppler will demonstrate increased atrial systolic flow reversals during expiration.
13. ANSWER: C. Echocardiographic hallmarks of restrictive physiology in adults include a increased mitral inflow Doppler E:A ratio >2.0, shortened mitral E-wave deceleration time <160 ms, decreased lateral mitral Ea velocity, and an increased E/Ea ratio >15. Pulmonary venous Doppler demonstrates decreased systolic to diastolic pulmonary venous filling wave ratio with significantly increased atrial reversal wave velocity and duration.
14. ANSWER: D. Patients with Down syndrome (trisomy 21) have an almost 50% incidence of congenital heart disease, with AVSD being the most common cardiac anomaly in this cohort. AVSD in association with tetralogy of Fallot is a common constellation of cardiac anomalies in patients with Down syndrome. Obstruction of the LVOT and coarctation of the aorta are also common cardiac abnormalities in patients with AVSD but are not as common in Down syndrome patients. Left ventricular hypoplasia can also occur in the setting of AVSD (“unbalanced AVSD with right ventricular dominance”) but is less commonly seen in this cohort. Aortic valve stenosis and anomalous pulmonary venous connections are uncommon.
15. ANSWER: D. Anatomic hallmarks of AVSD include a cleft in the anterior leaflet of the left atrioventricular valve, lateral rotation of the left ventricular papillary muscles, and attachments of the left and right atrioventricular valves at the same level at the cardiac crux. In addition, due to the absence of the atrioventricular septum in these defects, the left ventricular inflow is shortened and the left ventricular outflow is elongated (“goose-neck deformity”) creating a ratio of LV inlet to LV outlet ratio <1. Owing to the presence of a common atrioventricular valve, the aortic valve is no longer “wedged” between the tricuspid and the mitral valves and is pushed anteriorly (“sprung”).
16. ANSWER: B. M-mode has excellent temporal resolution and a high fixed PRF. The x-axis represents time while the y-axis represents distance from the transducer. M-mode utilizes a single imaging crystal.
17. ANSWER: A. Resolution is defined as the smallest distance between 2 points that are distinguishable from one another. Axial resolution is the ability to differentiate points along the ultrasound beam and is equal to its wavelength. Lateral resolution is the ability to resolve points perpendicular to the ultrasound beam and is dependent on beam width, with the best resolution found where the beam is the narrowest. Axial resolution is better than lateral resolution.
18. ANSWER: A. Doppler velocity is calculated as follows: V = [c(fd)]/[2fo cos θ]. The speed of sound (c) and the transmitted ultrasound frequency (fo) are constant while the frequency shift (fd) can be measured very accurately. Therefore, the main source of error in velocity calculation is the angle of incidence (θ) between the ultrasound beam and the moving structure or blood. When the angle of incidence is <20 degrees, the Doppler velocity is not significantly underestimated (Fig. 5.14).
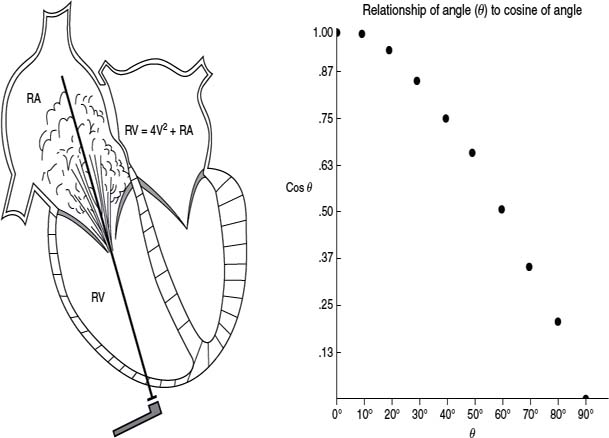
19. ANSWER: B. CW Doppler utilizes two crystals, one that is continuously transmitting and one that is continuously receiving, making the sampling rate infinite so that there is no limit to the detection of the maximal frequency shift. A disadvantage is that there is no range-gating resulting in lack of range resolution (the maximal Doppler velocity can be anywhere along the ultrasound beam path). Both CW and PW Doppler are equally dependent on the angle of incidence for accurate velocity determination (Fig. 5.15).
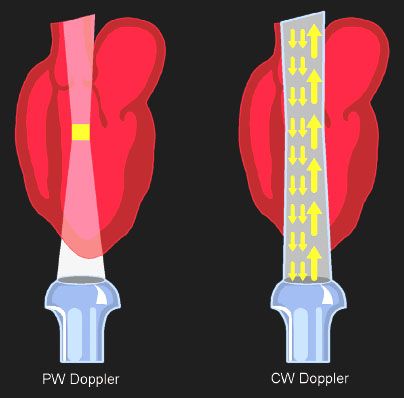
20. ANSWER: C. PW Doppler utilizes one crystal that intermittently transmits and receives. The time between transmission and reception allows determination of the depth of the signal providing excellent range resolution. However, the maximal detectable frequency shift is limited resulting in a lower Nyquist limit than CW Doppler. Spectral Doppler has a higher PRF than color Doppler. PRF varies with the depth of the sample volume with PW Doppler, with a higher PRF with more shallow sample volumes.
21. ANSWER: A. The Nyquist limit is the maximal frequency shift detectable by PW Doppler and is equal to one-half of the PRF. The Nyquist limit is lower with PW Doppler and is increased with lower frequency transducers and at shallower depths of interrogation.
22. ANSWER: A. Color Doppler utilizes multiple sampling sites along multiple ultrasound beams to generate frequency shifts that are converted into a digital format and autocorrelated into a color scheme. Color Doppler is a mean velocity of blood flow with the intensity of color representing mean Doppler flow velocities. The Nyquist limit is lower with color Doppler compared to spectral Doppler. Color Doppler is superimposed on 2D images resulting in less resolution.
23. ANSWER: D. Subpulmonary ventricular septal defects are located adjacent to the pulmonary valve and aortic valve. These VSDs have been termed subpulmonary, supracristal, or doubly committed defects. These defects can be best demonstrated in the parasternal short-axis scan plane but can also be demonstrated from the subcostal and apical windows with appropriate angulation into the right ventricular outflow tract.
24. ANSWER: A. Aortic regurgitation is the most common associated abnormality because of prolapse of the aortic cusp into a subpulmonary ventricular septal defect. While this associated prolapse of aortic tissue limits the size of the VSD and can lessen the left-to-right shunt, the progression of aortic insufficiency due to distortion of the aortic valve is well recognized. If this regurgitation is significant and progresses, then surgical closure of the ventricular septal defect is indicated (and is not dependent on the size of the left-to-right shunt).
25. ANSWER: C. Large ventricular septal defects result in equalization of right and left ventricular pressures as well as elevated pulmonary arterial pressure. Left-to-right shunting at ventricular level results in a substantial increase in pulmonary blood flow with left atrial and left ventricular volume overload. Overall systemic blood flow is not significantly increased in this setting.
26. ANSWER: A. The best morphologic hallmarks of the right atrium are the broad based right atrial appendage and the connections of the inferior vena cava and coronary sinus. Superior vena caval connection(s) have significant anatomic variability. Atrioventricular relationships can also vary and are not hallmarks of right atrial morphology. The valve of the fossa ovalis is a right atrial structure while septum primum is a left atrial structure. The atrioventricular valve is a hallmark of ventricular morphology, with the morphologic tricuspid valve being the anatomic hallmark of the right ventricle.
27. ANSWER: B. The best imaging plane to define the entire atrial septum is the subcostal imaging plane because it is perpendicular to this anatomic structure. False dropout can occur in imaging planes that are more parallel to the atrial septum.
28. ANSWER: B. The best anatomic hallmark of the morphologic right ventricle is the connection of the tricuspid valve with a more apical insertion at the cardiac crux compared to the morphologic mitral valve. The tricuspid valve is “septophilic” with attachments to the ventricular septum. The right ventricle is more crescent in shape with prominent trabeculations.
29. ANSWER: D. A higher insertion of the morphologic mitral valve at the cardiac crux and lack of atrioventricular valve chordal attachments to the ventricular septum (“septophobic”) are excellent anatomic hallmarks of the morphologic left ventricle. The LV is elliptical in shape with fine trabeculations, mainly toward the cardiac apex.
30. ANSWER: A. Utilizing the modified Bernoulli equation to obtain the peak instantaneous gradient across the pulmonary valve, 4 × (velocity)2 then 4 × (4.0)2 = 64 mm Hg.
31. ANSWER: B. The most common type of subaortic stenosis is related to a discrete membrane proximal to the aortic valve within the LVOT (Fig. 5.16). This membrane is most often circumferential and can be adherent to both the aortic valve and the anterior leaflet of the mitral valve. LVOT obstruction in the setting of hypertrophic cardiomyopathy (HCM) is often related to asymmetric septal hypertrophy in combination with systolic anterior motion of the mitral valve chordal and leaflet tissue. Anomalous mitral chordal insertions within the LVOT can be isolated or found in association with congenital heart disease and may result in obstruction but are not as common as discrete membranes (Fig. 5.16).
32. ANSWER: A. Bicuspid aortic valve is the most commonly associated cardiac finding in patients with simple coarctation with some studies showing as high as an 80% occurrence in patients with coarctation. Atrial and ventricular septal defects are also common in patients with coarctation. Pulmonary valve stenosis and coronary arterial anomalies are much less frequent in this cohort.
33. ANSWER: C. The aortic lumen must be narrowed by at least 50% to significantly affect systemic arterial pressure.
34. ANSWER: C. Cardiac tamponade occurs when increasing fluid in the pericardial space causes a rise in intrapericardial pressure (typically greater than intracardiac pressure) compromising systemic venous return to the right atrium. Diastolic right atrial and right ventricular wall collapse occurs when intrapericardial pressure exceeds intracardiac pressure, with collapse of the right ventricle more sensitive to identify tamponade physiology. Doppler features are more sensitive to identify cardiac tamponade with respiratory changes in Doppler flow across the tricuspid valve (>30%) and mitral valve (>25%) most characteristic due to ventricular interdependence. While the overall size of the pericardial effusion is important, how quickly the fluid accumulates has more of an effect on intrapericardial pressure due to the relative compliance of the pericardium in the acute and chronic settings.
35. ANSWER: E. The relationship between velocity of circumferential fiber shortening and end-systolic wall stress is independent of heart rate and preload and incorporates afterload making it a quantitative measure of ventricular contractility. Ejection fraction, shortening fraction, and the myocardial performance index are all significantly impacted by both preload and afterload.
36. ANSWER: A. SF = (LV EDD – LV ESD) / LV EDD. Left ventricular shortening fraction is maximal during the first month of life (range 35% to 45%). Mean LV shortening fraction in children is 36% and ranges from 28% to 40%.
37. ANSWER: B. The presence of holodiastolic Doppler flow reversal is consistent with a significant run-off from the descending aorta including a large patent ductus arteriosus, severe aortic valve regurgitation, systemic-to-pulmonary artery shunts, and large arteriovenous fistula.
38. ANSWER: C. The most common ventricular septal defect associated with coarctation is a perimembranous defect. While less common, a posterior malalignment VSD often results in severe coarctation or interruption of the aortic arch. Muscular VSD as well as inlet VSD can also occur in the setting of coarctation, in particular with an unbalanced RV-dominant AVSD.
39. ANSWER: A. The systolic jet in patients with supravalvar aortic stenosis propagates further than the jet originating with aortic valvar stenosis and has a tendency to be entrained along the aortic wall thereby transferring its kinetic energy into the right innominate artery. This physical principle, termed the Coanda effect, often is expressed clinically in these patients by marked discrepancy in upper arm blood pressures, with the right arm pressure higher than the left arm blood pressure.
40. ANSWER: B. In the simplified Bernoulli equation, convective acceleration is calculated while flow acceleration and viscous friction are ignored. To accurately utilize the simplified equation, the proximal Doppler velocity must be negligible (Fig. 5.17).
41. ANSWER: C. An overriding atrioventricular valve empties into two ventricles. It is committed to the ventricle that >50% of its orifice is directed (Fig. 5.18). This connection is always associated with a malalignment VSD. Valves that override can also straddle by having chordal attachments to the contralateral ventricle (Fig. 5.18).
42. ANSWER: E. A straddling atrioventricular valve has anomalous chordal insertions or papillary muscles in the contralateral ventricle. Straddling and override often coexist. Straddling is associated with the presence of a ventricular septal defect but does not require a malalignment type of defect. Semilunar valves do not have chordae or papillary muscles so therefore do not straddle. Straddling is not a common feature of tetralogy of Fallot.
43. ANSWER: C. Interruption of the intrahepatic portion of the inferior vena cava with azygous vein continuation to the superior vena cava is a common feature of polysplenia syndrome (left atrial isomerism). The abdominal situs is variable and can be ambiguous, inversus, or solitus. While spleen are usually multiple, they are characteristically located on the same side. A single gall bladder is most typical but biliary atresia can and does occur.
44. ANSWER: E. In the normal heart the aorta is located in a rightward and posterior location relative to the pulmonary artery. In D-transposition, the aorta is typically anterior and rightward. In L-transposition (congenitally corrected TGA), the aorta is most commonly anterior and leftward. The aorta is also most commonly leftward and anterior in double inlet left ventricle.
45. ANSWER: C. Tricuspid atresia is an example of a single inlet atrioventricular valve connection (Fig. 5.19).
46. ANSWER: D. Type A interruption of the aortic arch occurs distal to the origin of the left subclavian artery. Type B interruption occurs between the left common carotid and left subclavian arteries. Type C interruption occurs between the right innominate and the left common carotid arteries.
47. ANSWER: B. When a persistent left superior vena cava drains to the coronary sinus, the size of the coronary sinus is inversely proportional to the size of the bridging innominate vein. When the coronary sinus is severely dilated, the innominate vein is most commonly very small or absent. When the inferior vena cava is interrupted, venous return is directed from the azygous vein to the superior vena cava. Interruption of the IVC is more common in polysplenia syndrome versus asplenia syndrome. Superior vena caval connections are variable and are not an anatomic hallmark of the morphologic right atrium. The left pulmonary veins more commonly merge than the right veins as they connect to the left atrium.
48. ANSWER: D. While all these are features that distinguish the morphologic tricuspid valve from the mitral valve, the most reliable anatomic hallmark is the level of attachment of the atrioventricular valve at the cardiac crux. The atrioventricular valves are invariably associated with their appropriate morphologic ventricle (tricuspid valve with the right ventricle and mitral valve with the left ventricle) and are the best marker for atrioventricular connection and ventricular morphology.
49. ANSWER: B. Organ systems with sidedness include the cardiac, pulmonary, and gastrointestinal systems. Cardiac sidedness is determined by the position of the right atrium. Pulmonary situs is defined by the positions of the morphologic right and left lungs. Abdominal situs is characterized by the location of the liver and stomach.
50. ANSWER: C. This subcostal coronal image demonstrates a sinus venosus atrial septal defect with partial anomalous pulmonary venous connection to the superior vena cava. The defect is located in the superior/posterior portion of the atrial septum adjacent to the superior vena cava. The right upper and middle pulmonary veins are often anomalous and most commonly connect to the superior vena cava.
51. ANSWER: A. These images demonstrate the classic features of a partial AVSD (Fig. 5.20). There is a large primum atrial septal defect with a large left-to-right atrial level shunt. Owing to lack of the atrioventricular septum, both atrioventricular valves are inserted at the same level at the cardiac crux. The inlet ventricular septum is intact. Color Doppler also demonstrates significant mitral regurgitation, most likely related to a cleft in the anterior leaflet.
52. ANSWER: E. Both the parasternal and the subcostal images demonstrate a large anterior malalignment ventricular septal defect with ~50% aortic override of the VSD. This anatomy can be consistent with tetralogy of Fallot, pulmonary atresia with VSD, or truncus arteriosus with additional imaging of the right ventricular outflow tract, the pulmonary arteries, and aortic arch helping to differentiate these diagnoses.
53. ANSWER: B. This parasternal short-axis scan demonstrates a large membranous VSD with a large left-to-right shunt.
54. ANSWER: C. This parasternal long-axis scan demonstrates significant aortic root dilatation consistent with Marfan syndrome. Classic echocardiographic features of Marfan syndrome include aortic root dilatation and mitral valve prolapse. Hallmark cardiac findings in Down syndrome include AVSD and VSDs. Most common cardiac lesions in DiGeorge syndrome include aortic arch anomalies and conotruncal defects. Noonan syndrome typically has right ventricular outflow and pulmonary artery anomalies as well as atrial septal defects and HCM. Williams syndrome classically presents with supravalvar aortic stenosis and supravalvar/branch pulmonary arterial stenoses.
55. ANSWER: B. Cardiac myxomas are the most common adult cardiac tumor and the second most common childhood cardiac tumor. The majority (75%) are located in the left atrium and are typically attached to the fossa ovalis. When large, they can obstruct atrioventricular valve inflow leading to symptoms including positional dyspnea, syncope, and even death. Constitutional symptoms include weight loss, malaise, arthralgias, and myalgias. Carney syndrome is a familial form of myxoma and is associated with lentigines and endocrine abnormalities.
56. ANSWER: C. This parasternal long-axis scan shows a large homogeneous echogenic mass in the posterior wall of the left ventricle consistent with a cardiac fibroma. Fibromas are firm, white, nonencapsulated tumors. They are typically located in the left ventricle within the posterior wall or septum and commonly at the cardiac apex. They are often large and can result in cavitary obstruction or impair atrioventricular valve function. These tumors also have a significant risk of sudden death due to ventricular arrhythmias.
57. ANSWER: C. The right ventricle ejects ~55% to 60% of combined fetal cardiac output while the left ventricle ejects 40% to 45%. Cardiac output increases significantly during gestation, but the relative amounts of output from these two parallel circulations remain relatively the same.
58. ANSWER: C. This fetus has significant hemodynamic compromise by the underlying fetal tachycardia. Starting sotalol is the most effective therapy to treat this hydropic fetus. Digoxin has poor maternal fetal transfer in the hydropic fetus and is not the first-line drug therapy in this clinical scenario. Maternal lupus is associated with fetal heart block and bradycardia; hence, evaluation of ant-SSA/Ro and anti-SSA/La antibodies is not indicated. At 22 weeks, delivery of a live fetus is not an optimal strategy either so pretreatment of the mother with betamethasone is not indicated.
59. ANSWER: D. Evaluation of the outflow tracts is necessary to exclude d-TGA because the four-chamber view is often normal in these fetuses. The remainder of the listed congenital heart lesions is readily diagnosed in the fetal four-chamber view.
60. ANSWER: B. The normal fetal heart comprises about one-third of the fetal thorax, ranging from ~25% to 35%.
61. ANSWER: A. Fetal arrhythmias occur in ~1% to 3% of all pregnancies. PAC comprise the largest percentage of these rhythm abnormalities followed by PVC. Fetal SVT, atrial flutter, and complete heart block account for <10% of all reported fetal arrhythmias.
62. ANSWER: D. This is the mechanical PR interval, measured from the beginning of atrial inflow (mitral A-wave) to the beginning of ventricular ejection.
63. ANSWER: E. With lack of antegrade flow across the atretic pulmonary valve, fetuses with pulmonary atresia with intact ventricular septum often have reversal of flow across the ductus arteriosus into the hypoplastic main pulmonary artery and branch pulmonary arteries. The other listed congenital heart lesions all typically have a normally functioning pulmonary valve with antegrade flow into the main pulmonary artery and ductus arteriosus.
64. ANSWER: C. Because of limited antegrade blood flow across the critically stenotic aortic valve, flow within the aortic arch is supplied retrograde from the ductus arteriosus. The other listed congenital heart lesions all typically have a normally functioning aortic valve with antegrade flow into the ascending aorta and transverse aortic arch and antegrade flow from the ductus arteriosus to the descending aorta.
65. ANSWER: C. The normal fetal heart rate ranges from 100 to 180 BPM throughout gestation. Fetal bradycardia is defined as a sustained heart rate less than 100 BPM while fetal tachycardia as a sustained rate greater than 180 BPM.
66. ANSWER: A. The normal leftward axis of the fetal heart (relative to the midline) ranges from 30 to 60 degrees.
67. ANSWER: A. At term, ~10% of fetal cardiac output perfuses the lungs. The remainder of this deoxygenated blood is directed through the ductus arteriosus to the descending aorta and placenta for oxygenation.
68. ANSWER: A-4, B-2, C-1, D-3, E-5. Lithium has been shown in studies to be associated with fetal Ebstein’s anomaly as well as atrial septal defects and atrioventricular valve atresia. Fetal alcohol syndrome has been commonly associated with septal defects including atrial and ventricular septal defects and is less commonly associated with coarctation and conotruncal defects. Indomethocin is a potent ductal constrictor. Coarctation of the aorta and LVOT obstruction has been described in fetal hydantoin syndrome. Exposure to isotretinoin during gestation has been associated with fetal d-TGA as well as septal defects and conotruncal anomalies.
69. ANSWER: A-3, B-1, C-4, D-2, E-5. Turner syndrome is most commonly associated with coarctation of the aorta and aortic stenosis with bicuspid aortic valve. Other less common defects in Turner syndrome include atrial and ventricular septal defects. DiGeorge syndrome is characterized by interrupted aortic arch and conotruncal defects, including truncus arteriosus. The hallmark lesion associated with trisomy 21 is an AVSD; other lesions include secundum atrial septal defect, ventricular septal defect, tetralogy of Fallot, and aortic arch obstruction. Trisomy 13 has a very high incidence of congenital heart disease, namely ventricular septal defects. Also associated is hypoplastic left heart syndrome, tetralogy of Fallot, and AVSD. William’s syndrome is most commonly associated with supravalvar aortic stenosis and branch pulmonary artery stenosis but also with septal defects and aortic arch anomalies.
70. ANSWER: E. Maternal systemic lupus is associated with complete heart block in the fetus. Umbilical cord compression can result in transient fetal bradycardia or even brief asystole. Both heterotaxy syndrome and congenitally corrected L-TGA are also associated with complete heart block and fetal bradycardia. Tetralogy of Fallot is not a frequent association with fetal conduction abnormalities.
71. ANSWER: A. Ebstein’s anomaly is associated with a 15% to 20% incidence of rhythm abnormalities, most notably Wolff–Parkinson–White syndrome and SVT.
72. ANSWER: C. Doppler velocities within the umbilical artery reflect downstream resistance within the placenta. The pulsatility index is defined as the peak systolic velocity minus the end diastolic velocity divided by the mean velocity.
73. ANSWER: D. In fetuses with congestive heart failure, the cerebral resistance typically falls (“brain-sparing effect”) resulting in a decreased pulsatility index in the middle cerebral artery. A concomitant increase in the umbilical artery pulsatility index is a common finding. Pulsations within the umbilical vein or flow reversal in the ductus venosus are ominous signs in the fetus with heart failure and compromised cardiac output. Atrioventricular valve regurgitation is common in fetal heart failure.
74. ANSWER: D. While right ventricular hypertrophy is one of the salient features of tetralogy of Fallot, it is usually secondary to RV outflow obstruction and develops postnatally. Prominent hypertrophy during fetal life is present in the recipient twin in twin-twin transfusion syndrome as well as poorly controlled maternal diabetes in late gestation fetuses. Both fetal HCM and Noonan syndrome have variable expression of ventricular hypertrophy (from absent to massive hypertrophy).
75. ANSWER: A. The incidence of congenital heart disease in maternal diabetes (4% to 10%) is higher than those with a previous family history of congenital heart disease (2% to 4%). The most common cardiac lesions in fetuses of diabetic mothers include D-TGA, truncus arteriosus, and tetralogy of Fallot. Risk of congenital heart disease in the fetus has been directly associated with the maternal hemoglobin A1C level during early gestation. HCM associated with poor maternal glucose control is most often reversible within weeks or months post delivery.
76. ANSWER: E. Most implanted metallic objects, including coils, clips, pacemaker leads, and occluder devices, are weakly ferromagnetic and are relatively immobile after implantation. Pacemakers and AICDs are a relative contraindication to a cardiac MR exam, but recent reports suggest that even these devices may be safe for the MR examination.
77. ANSWER: C. Stainless steel objects, such as PDA coils, cause the most imaging artifact with MR imaging. Occluder devices including the Amplatzer ASD device also cause significant imaging artifact. Pacemaker leads, PDA vascular clips, and nonferromagnetic stents cause less artifact with MR imaging.
78. ANSWER: A. With spin echo, there is a relatively long time period between spin excitation and data sampling resulting in blood flow leaving the imaging plane when the signal is sampled. This produces an image where blood appears black and surrounding cardiac tissue is encoded in shades of gray or white.
79. ANSWER: E. Cardiac magnetic resonance imaging offers unique advantages in the evaluation of extracardiac structures including pulmonary venous anatomy. Both echocardiography and cardiac magnetic resonance imaging can evaluate myocardial deformation and AV valve regurgitation and calculate the degree of left-to-right shunting in patients with a VSD. Echocardiography is the current noninvasive methodology of choice to evaluate LV diastolic function.
80. ANSWER: C. VCE MRI is a gradient echo sequence that can measure blood flow velocity and quantify blood flow rate. This VEC MR technique is capable of acquiring both anatomic and velocity information and has been shown to correlate closely with invasive measures of flow.
81. ANSWER: D. Spin echo cardiac magnetic resonance imaging is a black blood technique where the blood pool is black and the surrounding cardiac tissue is encoded in shades of gray or white. Signal acquisition is performed over several cardiac cycles. This technique produces high tissue contrast and has less imaging artifact with metallic implants compared to other cardiac MR techniques. Spin echo applications include imaging myocardial and blood vessel walls, cardiac masses and tumors, and the pericardium.
82. ANSWER: A. Gradient echo sequences have less time between spin excitation and signal detection resulting in a faster acquisition than spin echo sequences. Therefore, the gradient echo technique results in high imaging speed with multiple images acquired during each cardiac cycle. The signal from slower moving tissue is gray and has less contrast compared to spin echo images and is more susceptible to imaging artifacts. Faster moving blood has a stronger signal resulting in bright blood images.
83. ANSWER: A. MDE has become the primary cardiac MR technique to assess myocardial viability. Washout of gadolinium contrast agents is delayed in necrotic myocardium as well as areas of fibrotic tissue. Nonviable myocardium therefore appears bright when compared to viable myocardium. MDE has been shown to be very effective in determining the presence, size, and transmurality of myocardial infarctions as well as in the identification of the presence and extent of myocardial fibrosis in patients with HCM.
ACKNOWLEDGMENT
Figures 5.3, 5.4, 5.5, 5.8, 5.9, 5.11, 5.12, 5.14, 5.15, 5.17, 5.18, 5.19 and 5.20 are from Eidem BW, Cetta F, O’Leary PW. Echocardiography in Pediatric and Adult Congenital Heart Disease. Philadelphia: Lippincott Williams & Wilkins, 2010. © Mayo Foundation for Medical Education and Research. All rights Reserved.
SUGGESTED READINGS
Allen HD, Driscoll DJ, Shaddy RE, et al. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
Didier D, Ratib O, Beghetti M, et al. Morphologic and functional evaluation of congenital heart disease by magnetic resonance imaging. J Magn Reson Imaging. 1999;10:639–655.
Drose JA. Fetal Echocardiography. 2nd ed. St Louis, MO: Saunders Elsevier; 2010.
Eidem BW, Cetta F, O’Leary PW. Echocardiography in Pediatric and Adult Congenital Heart Disease. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.
Hance-Miller W, Fyfe DA, Stevenson JG, et al. Indications and Guidelines for performance of transesophageal echocardiography in the patient with pediatric acquired or congenital heart disease. A report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J Am Soc Echocardiogr. 2005;18:91–98.
Kilner PJ, Geva T, Kaemmerer H, et al. Recommendations for cardiovascular magnetic resonance in adults with congenital heart disease from the respective working groups of the European Society of Cardiology. Eur Heart J. 2010;31:794–805.
Lai WW, Geva T, Shirali GS, et al.; Task Force of the Pediatric Council of the American Society of Echocardiography. Pediatric Council of the American Society of Echocardiography. Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J Am Soc Echocardiogr. 2006;19:1413–1430.
Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463.
Lopez L, Colan SD, Frommelt PC, et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr. 2010;23:465–495.
Oh JK, Seward JB, Tajik AJ. The Echo Manual. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
Prakash A, Powell AJ, Krishnamurthy R, et al. Magnetic resonance imaging evaluation of myocardial perfusion and viability in congenital and acquired pediatric heart disease. Am J Cardiol. 2004;93:657–661.
Prakash A, Powell AJ, Geva T. Multimodality noninvasive imaging for assessment of congenital heart disease. Circ Cardiovasc Imaging. 2010;3:112–125.
Rychik J, Ayres N, Cunco B, et al. American Society of Echocardiography guidelines and standards for performance of the fetal echocardiogram. J Am Soc Echocardiogr. 2004;17:803–810.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


