4 OBJECTIVES
Noncardiac Chest Pain
 List the various organ systems that are responsible for causing chest pain, describe the diseases of the respiratory, musculoskeletal, and gastrointestinal systems that cause chest pain, and elucidate how to differentiate them.
List the various organ systems that are responsible for causing chest pain, describe the diseases of the respiratory, musculoskeletal, and gastrointestinal systems that cause chest pain, and elucidate how to differentiate them.
 Explain the pathophysiology and pathogenesis of common causes of chest pain other than coronary artery disease and describe the evaluation of patients with these diseases.
Explain the pathophysiology and pathogenesis of common causes of chest pain other than coronary artery disease and describe the evaluation of patients with these diseases.
 Evaluate and critique neuropsychiatric causes of chest pain.
Evaluate and critique neuropsychiatric causes of chest pain.
GENERAL CONSIDERATIONS
Chest pain is a very common symptom that can result from a number of causes and may denote serious or life-threatening diseases such as acute coronary syndrome (ACS), pulmonary embolism, and tension pneumothorax. Conversely, it may result from a disorder that may not be life threatening but may be disabling because of the patient’s anxiety about the discomfort. Because of the potential seriousness of the complaint of chest pain, it should prompt immediate evaluation. Identification of the correct cause requires a thorough understanding both of the patient’s symptoms and of the differential diagnosis of disorders that can cause chest pain.
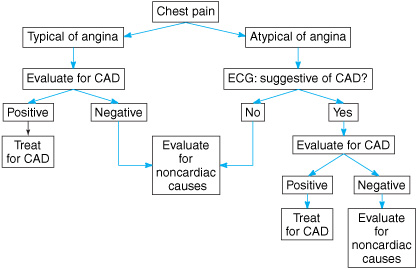
Coronary artery disease (CAD) remains the leading cause of death in the United States. For this reason, the immediate priority in evaluating a patient with chest pain is to assess for CAD as the cause of the pain (Figure 4–1). The process begins with a history and physical examination, but the physician must appreciate the limitations of history and physical examination in distinguishing the cause of chest pain. Evaluation for ACS, or chest pain caused by myocardial ischemia, often includes a number of laboratory tests such as cardiac enzyme levels, exercise testing, echocardiography, computed tomography (CT) angiography, and thallium scintigraphy. One third of patients initially evaluated for ACS in the emergency department are discharged or released after 36 hours of observation without the diagnosis of acute ischemia. When the cause remains unclear after these tests, the patient is often assessed with coronary arteriography. A number of risk factors predict the chances of an abnormal angiogram. However, of patients who undergo coronary arteriography, 20%–30% have normal or near-normal coronary arteries, and the cause of their chest pain remains unclear. About 80% of this group continues to have chest pain for 10 years or more and 50% remain disabled because of chest pain.
Figure 4–1. The evaluation of chest pain begins with a history and is initially directed at eliminating coronary artery disease (CAD) as the cause of chest pain. If the results of the evaluation are negative for CAD, the evaluation should proceed to search for other causes. “Noncardiac causes” include all causes of chest pain other than CAD and may include some causes referable to the heart (see text). See Figure 4–2 for the evaluation of noncardiac causes of chest pain. ECG, electrocardiogram.
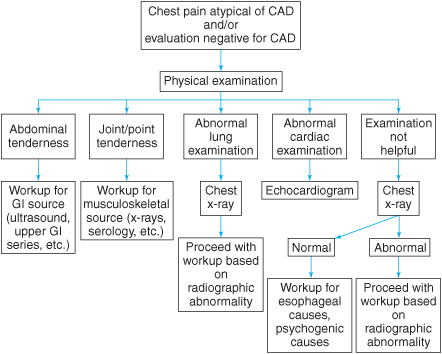
Determining the cause of chest pain not due to CAD is often difficult (Figure 4–2). Various studies have demonstrated that common causes include gastrointestinal (GI), musculoskeletal, pulmonary, and psychological disorders, as well as cardiac causes other than CAD. This chapter reviews these disorders and discusses approaches to the diagnosis.
PATHOPHYSIOLOGY OF CHEST PAIN
The pathophysiology of chest pain is variable. The lung, for example, can have pain arising from stimulation of the mucosa of the trachea and main bronchi, whereas the lung parenchyma along with the visceral pleura is insensitive to painful stimuli as it is not innervated by nociceptive receptors. The tracheobronchial tree and lungs are innervated by autonomic afferent and efferent pathways. These include afferent pathways for the cough, stretch and irritant receptors in the central airways, but seldom include afferent pathways for pain. Pain originating from the tracheobronchial tree is presumably mediated by type C fibers or through the vagal pathway. Pain receptors in the parietal and diaphragmatic pleural surfaces are derived from the intercostal nerves; irritation of these areas results in pain in the adjacent chest wall. The central portion of the diaphragm is supplied by the phrenic nerve, and pain in this area is often perceived in the ipsilateral shoulder. It is the inflammation in the adjacent parietal pleura that causes chest pain. Distension of pulmonary vascular structures with stimulation of mechanical receptors from pressure overload states such as those seen in pulmonary hypertension and valvular stenosis may initiate pain in these conditions.
Figure 4–2. The evaluation of chest pain not caused by CAD is guided by history and physical examination. Additional tests may be ordered to aid with the diagnosis. See the text for a description of abnormal cardiac and pulmonary examination findings in patients with chest pain. GI, gastrointestinal.
Disorders of the chest wall secondary to trauma, inflammation, or fibrositis of the muscle bone articulations occurs and can produce superficial or deep somatic pain. The pain perception is initiated by nociceptors that can detect thermal, mechanical, or chemical changes above a certain threshold. The pain fibers travel via the spinal cord to the brain, specifically the somatosensory cortex and the limbic system. Radiculitis along the cutaneous distribution of the involved intercostal nerves can cause pain with associated hyperalgesia or anesthesia of the surrounding skin. Vascular compression and obstructive lesions affecting the sympathetic chain and stellate ganglion can lead to pain when the thoracic outlet area is affected either by tumor or other infiltrative disorders. The neurobiology of pain associated with cardiac and pericardiac structures is not clear and the chemical transmitters and sensory pathways that travel through the cardiac nerves, sympathetic ganglia, and the dorsal thoracic roots are not well understood. Pain attributed to mitral valve prolapse syndrome cannot be explained on the basis of mitral regurgitation, and autonomic and neuroendocrine dysfunction may be a possible cause. The pericardium contains few afferent pain fibers except in the diaphragmatic portion through the phrenic nerves. This results in pain referred to the area of the trapezius muscle and associated pleural pain is not uncommon. Vascular rupture with hematoma formation causes pain in aortic dissection.
Mechanical and thermoreceptors activated by stretch, chemical irritants, and stimulated through the vagal and sympathetic chain result in pain originating in the esophagus. Sensation from both the esophagus and the heart is transmitted to the central nervous system through the sympathetic and parasympathetic systems. The sympathetic or spinal afferents are primarily responsible for the sensation of esophageal pain. Centrally, the nociceptive primary afferents terminate on neurons in specific layers of the dorsal horn of the spinal cord. Convergence of multiple visceral afferents from both the heart and esophagus onto the same dorsal horn probably explains the difficulty in distinguishing between esophageal and cardiac pain.
PULMONARY CAUSES OF CHEST PAIN
Pleurisy & Pleural Effusion
Inflammation of the pleura (pleurisy or pleuritis) may be caused by a number of disorders (see Table 4–1). Pleurisy is typically characterized by fever, cough, dyspnea, and pleuritic chest pain (pain that varies with the respiratory cycle). Physical examination may reveal a pleural friction rub on the involved side, and a pleural effusion, which is usually an exudate, may be evident on chest x-ray. Pleurisy is more a syndrome than a true disease and is often associated with infections, neoplasms, or various connective tissue diseases, the most common of which is systemic lupus erythematosus. In some cases, pleurisy is the initial manifestation of lupus. When this occurs, the diagnosis of lupus is not usually immediately apparent. Lupus pleuritis is usually associated with fever, cough, dyspnea, and a pleural friction rub, and it tends to be recurrent. It is seen in both idiopathic and drug-induced lupus. The diagnosis of lupus pleuritis is made by pleural fluid analysis and serologic testing.
The differential diagnosis of pleural effusions is broad, and as discussed in greater detail in Chapter 11, the cause of pleural effusions must always be investigated, most often with thoracentesis. Patients with pleural effusions often present with dyspnea and with chest pain that may be sharp or dull in character. On physical examination, breath sounds are diminished and the chest is dull to percussion over the effusion. Above the effusion, the lung is atelectatic, and bronchial breath sounds are heard. Chest x-ray confirms the presence of an effusion. The most common causes for pleural effusions causing pain are infectious and neoplastic but the differential is extensive. Residual pleural scarring and persistently abnormal chest x-ray findings are common after resolution of the pleural effusion.
Table 4–1. Pulmonary causes of chest pain
Pleurisy and pleural effusion |
Malignant mesothelioma |
Pneumothorax |
Pneumomediastinum |
Diffuse parenchymal lung disease |
Pulmonary embolism |
Pulmonary hypertension |
Malignant Mesothelioma
Malignant mesothelioma has a classic presentation with pleural effusion with chest pain that may be referred to the ipsilateral shoulder or upper abdomen and that is typically constant rather than pleuritic in nature. The majority of patients with mesothelioma have a remote history of asbestos exposure; the latent period between asbestos exposure and the development of mesothelioma is 20–40 years. Smoking does not increase the risk of malignant mesothelioma as it does for most pulmonary neoplasms.
Physical examination may only reveal findings consistent with a pleural effusion. A pleural effusion, which may be massive, and pleural thickening are almost always evident on chest x-ray. The diagnosis is made with pleural biopsy. Malignant mesothelioma is difficult to distinguish histologically from adenocarcinoma, and for this reason many experts suggest that an open pleural biopsy is required for diagnosis. A percutaneous needle biopsy yields very small fragments of tissue and is often inadequate to allow differentiation of mesothelioma from adenocarcinoma. Pathologic distinction may be confirmed by electron microscopy and immunocytochemistry.
Pneumothorax
Chest pain is seen in up to 90% of patients with pneumothorax. The pain of pneumothorax is often anterior or radiating to the ipsilateral shoulder and is almost invariably associated with dyspnea. The diagnosis of spontaneous pneumothorax may be suspected based on the history of a sudden onset of unilateral chest pain, often pleuritic in nature, associated with sudden (and often worsening) dyspnea. Pneumothoraces are often described as primary or secondary. Primary pneumothoraces are classically seen in tall, thin young males without previous history of lung disease. The presumed etiology is the rupture of apical blebs and there is a high rate of recurrence. Secondary pneumothoraces occur in patients with known structural lung diseases (COPD, LAM, etc) or trauma including iatrogenic trauma such as complications from central venous access insertion. In patients on mechanical ventilators, worsening hypoxemia and increasing airway pressures suggest the possibility of pneumothorax.
Physical examination often reveals diminished or absent breath sounds and hyperresonance to percussion on the affected side of the chest. If the pneumothorax is large enough or is under tension, the trachea may be deviated away from the side of the pneumothorax. With a tension pneumothorax, the patient may become hypotensive because of decreased venous return to the heart resulting from increased intrathoracic pressure and will require emergency treatment.
The diagnosis of pneumothorax is confirmed with chest x-ray (see Chapter 11). However, a tension pneumothorax is usually easy to diagnose by history and physical examination alone, and delaying treatment until a chest x-ray can be obtained may result in a fatal outcome.
Pneumomediastinum
Pneumomediastinum is air within the mediastinum. The most common cause of pneumomediastinum is alveolar rupture with dissection of air along the bronchovascular bundle toward the hilum and into the mediastinum. Common causes include severe asthma attacks and with repeated Valsalva maneuvers during childbirth. Pneumomediastinum can also be the presenting sign of an esophageal rupture. The presenting symptom of pneumomediastinum is often substernal chest pain with radiation to the neck. The hallmark physical sign is Hamman’s sign, which is a grating sound heard over the precordium due to bubbles of air in the mediastinum. Hamman’s sign is usually synchronized with the heartbeat and is best heard with the patient in the left lateral decubitus position. Subcutaneous emphysema in the neck, face, and upper chest may also be present. Radiographic imaging is the confirmatory tests.
Diffuse Parenchymal Lung Disease
Diffuse parenchymal lung disease (DPLD) is an unusual cause of chest pain because of the lack of nociceptive receptors in the lung parenchyma. Pain caused by DPLD is usually due to inflammation of the pleura; thus, the pain is typical of pleurisy or of the major airways. The history is extremely important in developing the differential of DPLD with emphasis on exposures to drugs, occupations and hobbies, and symptoms of connective tissue diseases. The physical examination may be helpful with findings such as crackles and clubbing. The diagnosis is often made by radiographic imaging (CXR and high-resolution CT scanning) but the ultimate diagnosis is made by biopsy and histology. Chest pain caused by inflammation of the trachea and main stem bronchi is felt in the midline of the anterior chest or in the neck, and may be perceived as a dull, aching pain or as a burning pain. There are no specific physical findings associated with pain caused by this mechanism, but the history may suggest the diagnosis of inhalation of an irritant substance or acute tracheobronchitis.
Pulmonary Embolism
Chest pain is reported to occur in 60%–80% of patients with pulmonary embolism although dyspnea is the more common symptom. The cause of the pain is felt to be secondary to stretch on the proximal arteries, right ventricular strain or from pleurisy secondary to pulmonary infarction. The diagnosis of pulmonary embolism is difficult to make on clinical grounds alone, and clinical suspicion is correct no more than one third of the time. Nonetheless, pulmonary embolism is suspected in any patient who has the sudden onset of dyspnea, chest pain, hypoxemia, and a feeling of impending doom. Predisposing conditions include the components of Virchow’s triad which include venous stasis, intimal injury, and hypercoagulable states.
Physical examination is rarely helpful in the diagnosis of pulmonary embolism, although in some patients with massive pulmonary emboli, a right ventricular third heart sound (S3) may be heard, and jugular venous distention may be present. Most pulmonary emboli arise from deep veins in the lower extremities, and physical examination may reveal edema, erythema, and tenderness in a lower extremity, although these findings are unreliable.
Subtle signs of pulmonary embolism on the chest x-ray, including a pulmonary infiltrate, pleural effusion, and elevation of the hemidiaphragm, are sometimes present. However, confirmation of the diagnosis requires further testing including ventilation-perfusion scans, CT angiography, and pulmonary angiograms.
Pulmonary Hypertension
Pulmonary hypertension is sometimes associated with chest pain. The chest pain of pulmonary hypertension usually does not cause chest pain until it is advanced enough to cause right ventricular ischemia. The ischemia is caused by right ventricular pressure overload from increasing pulmonary vascular resistance. The classic description of pulmonary hypertension was primary versus secondary but the most accepted description is that of the World Health Organization (WHO) which divides it into five groups. Physical examination of a patient with severe pulmonary hypertension typically reveals a right ventricular lift and a loud pulmonic component of the second heart sound (P2). In the presence of right ventricular failure, jugular venous distention and peripheral edema are usually present. Enlarged pulmonary arteries are apparent on plain chest x-rays or chest CT scans in advanced pulmonary hypertension. There may be evidence of right ventricular enlargement on an electrocardiogram (ECG). Echocardiography or right heart catheterization and direct measurement of pulmonary artery pressure are required to make a definitive diagnosis of pulmonary hypertension.
GI CAUSES OF CHEST PAIN
General
 After CAD has been ruled out, the differential diagnosis of chest pain should include GI disorders. GI causes of chest pain can be divided into esophageal and nonesophageal categories (Table 4–2
After CAD has been ruled out, the differential diagnosis of chest pain should include GI disorders. GI causes of chest pain can be divided into esophageal and nonesophageal categories (Table 4–2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree