Fig. 2.1
ECG of patients during chest pain
Echocardiography: moderate concentric hypertrophy (LV mass/BSA 135 g/m2, relative wall thickness 0.45) with preserved LV global function (estimated ejection fraction of 56 %) and hypokinesia of the middle and apical anterior wall; normal dimension and function of the right ventricle (TAPSE 20 mm, FAC area 40 %); impaired relaxation of the left ventricle (E/A < 0.75, E/E’ < 10); mild mitral and tricuspid regurgitation; systolic pulmonary artery pressure of 35 mmHg
Chest x-ray showed the absence of pulmonary congestion, lobe consolidation, or bronchograms.
Clinical Course and Therapeutic Management
Clinical, instrumental, and laboratory data allowed us to make diagnosis of SCA-NSTEMI: ECG changes (ST depression >0.05 in more than two contiguous leads), rise in cardiac biomarker levels, and normal left ventricle global function with regional hypokinesia – no signs of myopericarditis.
According to guidelines, the patient was assessed with established risk scores for prognosis and bleeding (GRACE 120, intermediate risk; CRUSADE 30, low risk of bleeding). Antiplatelet therapy with aspirin and ticagrelor (P2Y12 inhibitor) with a loading dose of 300 mg and 180 mg, respectively, and anticoagulant therapy with fondaparinux 2.5 mg/die were started. Intravenous nitrate treatment and beta-blocker therapy (metoprolol 2.5 mg ev.) were administered due to persistent angina and tachycardia. ACE inhibitor (ramipril 5 mg) was continued, and high-dose statin therapy (atorvastatin 80 mg) was initiated.
The patient remained asymptomatic in the subsequent hours despite an increase in cardiac biomarkers (troponin I 15 ng/ml) at the laboratory analysis (6 h after patient admission). Given a GRACE score of 120, an ECG suggesting a left main or multivessel coronary artery disease (ST depression in many leads with ST elevation in avR) and the presence of high-risk criteria (significant rise in troponin) an early invasive strategy was performed. Thus, the patient underwent a coronary angiography (<24 h) that showed triple-vessel disease with a SYNTAX score >22 (Fig. 2.2).
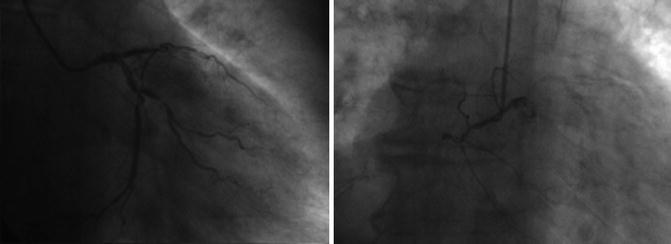
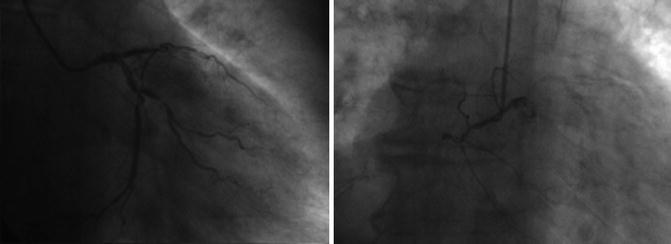
Fig. 2.2
Coronarography showing multivessel disease
Considering the clinical status (asymptomatic patient, progressive lowering in cardiac biomarkers: Tn I 10 ng/ml 12 h after patient admission) and the unfavorable coronary anatomy (SYNTAX score >22), the patient was sent for coronary artery bypass grafting (CABG, class I A). Ticagrelor was then discontinued, and CABG was performed 5 days later without procedural or bleeding complications. The patient was then transferred on day 12 to a postsurgery rehabilitation center with a progressive improvement in functional capacity and subsequently dismissed after 7 days. The therapy at discharge was dual-antiplatelet therapy (aspirin 100 mg and ticagrelor 90 bid), ramipril 5 mg, atorvastatin 80 mg, metoprolol 50 mg bid, pantoprazole 20 mg, and insulin therapy.
2.2 Non-ST-Segment Elevation Myocardial Infarction (NSTEMI)
Definition and Epidemiology
Coronary artery disease (CAD) is one of the major causes of deaths and morbidity in developed countries with a prevalence that increases with age [1]. Nearly 17.3 million deaths in 2013 worldwide were related to cardiovascular disease [2]. Acute coronary syndrome (ACS) represents one of the most frequent and life-threatening clinical presentations of CAD and is related to plaque rupture or an ischemic imbalance between myocardial oxygen supply and demand. The extensive use of high-sensitive troponin assay may have led to more diagnosis of myocardial infarction (MI) hiding a possible reduction in the incidence of MI [3]. According to the most recent guidelines [4], the term myocardial infarction should be used in the presence of symptoms of ischemia and/or rise in cardiac biomarkers (troponin I or T values above the 99th percentile upper reference limit) with the following criteria: ST-segment or T-wave changes, imaging evidence of loss of viable myocardium or regional motion abnormalities, and intracoronary thrombus by angiography or autopsy. Two different clinical presentations may be encountered based on electrocardiogram (ECG) findings and pathophysiology:
Myocardial infarction with persistent (>20 min) ST elevation (see Chap. 1).
Myocardial infarction without persistent ST elevation includes ST-segment depression >0.05 mV in two contiguous leads, T-wave inversion >0.1 mV in two contiguous leads, pseudo-normalization of T wave, or no ECG changes [4]. Two types of non-ST-elevation ACS are recognized: NSTEMI or unstable angina (UA) based on the evaluation of cardiac biomarkers.
In the last years, it has been observed an increase in the rate of non-ST-elevation myocardial infarction (NSTEMI) in relation to ST-elevation myocardial infarction (STEMI) with an annual incidence of ~3 per 1,000 inhabitants [5]. Hospital mortality is higher between STEMI patients, while in the long term death rates are consistently larger in NSTEMI [6]. NSTEMI patients are often older with significant comorbidities. These data suggest the need of significant efforts both in the acute phase and in long-term management to ensure better outcomes.
Pathophysiology
Atherosclerosis is a multifocal disease caused by lipid accumulation that affects large-sized and medium-sized arteries [7]. CAD is a dynamic process that leads to a progressive reduction in the vessel size due to plaque formation. NSTEMI is due to complete or partial occlusion of a coronary artery or a mismatch between oxygen supply and demand. ACS is generally precipitated by a plaque rupture or erosion with acute thrombosis or vasoconstriction leading to a sudden and critical reduction in blood flow. Inflammation plays a determinant role in plaque erosion and subsequent thrombus formation. Rarely ACS may be caused by other mechanisms such as arteritis, trauma, dissection, congenital abnormalities, or drug abuse [8].
Diagnosis
The diagnosis of NSTE is complex and more difficult than STEMI due to less obvious signs and a wider differential diagnosis. Risk stratification should be evaluated during the diagnostic phase guiding the revascularization and treatment strategy.
Clinical Presentation
The more frequent symptom of ACS is retrosternal chest pain irradiating to the left arm or to the neck sometimes described as retrosternal pressure or heaviness. Dyspnea, diaphoresis, or nausea is often associated. Atypical presentation is common in older patients, women, and patients with diabetes and may lead to a missed diagnosis [9]. Exacerbation of symptoms during physical exertion and reduction at rest is common. Relief of pain after administration of nitrates is also quite specific. UA is characterized by the presence of new-onset angina, post-MI angina, or crescendo angina. The presence of risk factors should be carefully evaluated as it significantly increases the probability of CAD diagnosis. The most common risk factors are male sex, family history of CAD, older age, peripheral artery disease, diabetes mellitus, renal failure, previous cardiovascular disease, and dyslipidemia.
Physical Examination
Physical examination shall evaluate the presence of NSTEMI complication such as heart failure with pulmonary or systemic congestion and establish the presence of precipitating factors (i.e., anemia). Extracardiac (pneumonia, pneumothorax, costochondritis) and nonischemic (valvular disease, pericarditis) causes of chest pain may also be excluded.
Electrocardiogram
A 12-lead resting ECG must be obtained in 10 min after the first medical contact. Additional ECG must be obtained if the patient presents symptoms at (3 h) 6-9-24 h and immediately during symptoms [8]. Comparison with previous ECG recordings is recommended especially in patients with known ST alterations (i.e., left ventricular hypertrophy). A completely normal ECG does not exclude the presence of ACS. Typical ECG findings are ST-segment depression or T-wave inversion in at least two contiguous leads.
Cardiac Enzymes
Cardiac troponins are the reference markers of MI because they are more specific and sensitive than other markers [10]. The initial rise in troponins occurs in approximately 4 h and may remain elevated up to 2 weeks. The diagnostic cutoff is a value exceeding the 99th percentile of normal reference population with an assay with an imprecision of <10 % [4]. High-sensitivity assays have been introduced with higher sensitivity and specificity. A single normal test is not sufficient to exclude ACS in the presence of suggestive symptoms and may be repeated. Relevant changes in troponin levels are also important because they allow to make differential diagnosis between a relevant number of possible non-ACS-related troponin elevations (Table 2.1).
Table 2.1
Possible causes of troponin rise
Chronic or acute renal failure |
Congestive heart failure |
Hypertensive crisis |
Arrhythmias |
Pulmonary embolism |
Myocarditis |
Stroke or subarachnoidal hemorrhage |
Aortic dissection |
Cardiac contusion, ablation, cardioversion |
Takotsubo cardiomyopathy |
Infiltrative disease (i.e., amyloidosis) |
Drug toxicity |
Sepsis or respiratory failure |
Rhabdomyolysis |
Imaging
Noninvasive Imaging
Echocardiography is the tool of choice due to its availability and feasibility. Left and right ventricular systolic function may be assessed and represents a relevant prognostic factor. New-onset regional wall hypokinesia or akinesia is also a typical finding that suggests myocardial ischemia. Echocardiography may also exclude other causes of chest pain such as aortic dissection, pulmonary embolism, aortic stenosis, pericarditis, or hypertrophic cardiomyopathy.
Stress echocardiography and nuclear myocardial perfusion are II° level tests that may lead to myocardial ischemia diagnosis especially in low-risk patients. Multidetector computed tomography (CT) permits visualization of coronary arteries and may be useful in excluding other causes of chest pain such as aortic dissection or pulmonary embolism. Different studies reported high negative predictive value of this technique in intermediate-risk patients [11].
Invasive Imaging
Coronary angiography remains the gold standard as it provides relevant diagnostic informations. Timing of angiography should be evaluated on the basis of risk assessment. It is recommended to prefer radial approach when feasible because it has lower risk of hematomas and bleeding [12]. Angiograms should be obtained after and before the use of nitrates to exclude the vasoconstriction due to ACS. In ambiguous lesions, intravascular ultrasound (IVUS) of fractional flow reserve (FFR) may help in the correct evaluation of stenosis and treatment strategy.
Risk Stratification and Treatment Strategy
To date two alternative approaches have been validated for the treatment of acute coronary syndromes (ACS) without ST-segment elevation (NSTE-ACS), such as unstable angina (UA) and acute myocardial infarction without ST elevation (NSTEMI). The two strategies differ in the timing for cardiac catheterization.
The first option is the early invasive strategy, meaning that the patient is quickly sent to the cath lab for coronary angiography, followed by the eventual PCI or surgical revascularization based on the angiographic results.
The second option, called conservative strategy, consists in medical therapy alone for the initial treatment, reserving cardiac catheterization only to those who have recurrent ischemia or other high-risk features.
Conservative Strategy Versus Invasive Strategy
Currently, the results of these alternative strategies have been analyzed in several randomized trials. A meta-analysis in which seven studies were included showed a significant benefit offered by the early invasive strategy in terms of reduction of 2-year mortality from all causes and myocardial infarction (MI), with no increase in adverse periprocedural events. Patients who have most benefited from an early invasive strategy were those with abnormal troponin values and high-risk features.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


