Non-ST Elevation ACS in the Emergency Department
Richard J. Ryan
Christopher P. Cannon
W. Brian Gibler
Why do we need a pathway for patients presenting to the emergency department (ED) with chest pain? Emergency physicians (EPs) encounter this chief complaint on a daily or hourly basis and thus the workup, diagnosis, and treatment should be “routine.” But it is not. For EPs and cardiologists alike, these patients represent an enormous challenge to accurately diagnose and appropriately treat. In particular, the ability to risk stratify non-ST-segment elevation myocardial infarction (NSTEMI) patients and initiate appropriate therapy is particularly difficult.
In the United States each year, approximately 5.3 million patients present to EDs with chest discomfort and related symptoms. Ultimately, nearly 1.4 million individuals are hospitalized for unstable angina (UA) and NSTEMI (1,2).
The 2002 American College of Cardiology/American Heart Association (ACC/AHA) UA/NSTEMI guidelines represent an evidence-based approach to the care of patients with ACS (3,4). From these guidelines a clinical pathway can be developed for the ED setting. A clinical pathway for NSTEMI initiated in the ED will allow EPs to standardize the diagnosis and treatment of patients with NSTEMI across the United States. Several summaries of the guidelines emphasizing emergency care have been published (5,6). Despite the 2002 guidelines and the recent 2005 AHA scientific statement on NSTEMI (7,8) adoption of these guidelines into routine emergency practice remains variable (9). The purpose of a clinical pathway for NSTEMI is to provide the EP and cardiologist at any hospital with a practical approach to treating patients with this condition. Basing medical therapy on a well-established clinical pathway will also allow for clinical quality improvement and real-time feedback to the entire hospital health care team.
The EP treating patients that arrive with chest pain must be able to succinctly incorporate the diagnostic elements such as electrocardiography and cardiac biomarker testing, as well as treatment regimens including nitrates, morphine, beta-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors (ACEIs), antiplatelet agents, and antithrombin drugs for acute coronary syndrome (ACS) for the care of the individual patient. After this, the EP must risk stratify these patients. Those patients with the highest risk can then be identified for guideline-directed pharmacological therapy and early invasive therapy for revascularization. A clinical pathway for NSTEMI patients will help EPs and cardiologists integrate care in an evidence-based, consistent approach for their patients. This will ultimately improve multidisciplinary communication, standardize care, and improve patient outcomes.
A clinical pathway for NSTEMI must be based on guidelines that provide extensive evidence for diagnostic and treatment regimens that provide substantial benefit in the early period after the patient with ACS presents to the ED. The 2002 ACC/AHA UA/NSTEMI guidelines use recommendation classes that rapidly allow one to make choices regarding diagnostic and treatment strategies. A Class I recommendation is generally considered to be useful and effective. Aspirin serves as an excellent example of a Class I treatment. Designation of a regimen as Class IIa identifies a treatment as generally considered effective, but some controversy may be present about the usefulness of a treatment. A Class IIb recommendation suggests that a treatment is controversial but leans toward efficacy. A therapy or diagnostic strategy that is Class III is not useful and may actually be harmful in some cases. Weighting of evidence for these Class I, II, and III recommendations is straightforward. If data from multiple large, randomized trials support a recommendation, then the weight of evidence is A. An evidence grade of B for a therapy is provided if fewer, smaller randomized trials, analyses of nonrandomized studies, or observational registries support a recommendation. Expert consensus provides an evidence grade of C (Table 5-1) (3).
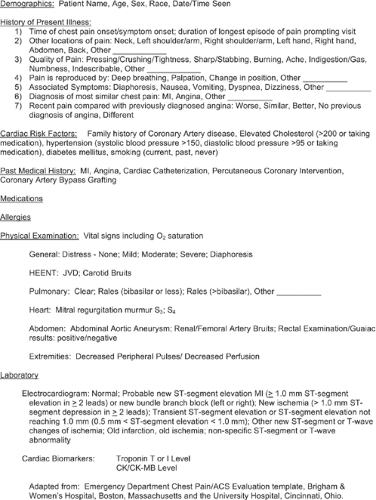
Once an EP identifies a patient with potential ACS, it is critical to quickly risk stratify this patient and promptly deliver guideline-directed therapy. Risk stratification is based on the patient’s history, physical examination, 12-lead electrocardiogram (ECG), and cardiac biomarkers such as troponin and creatinine kinase-MB (CK-MB). The risk stratification process includes (a) determining if the symptoms the patient is having are the result of ACS, and (b) among patients with probable/definite ACS, identifying patients who are at higher or lower risk of death and myocardial infarction (MI) as a complication of their ACS event.
In patients with ACS the history usually includes chest discomfort as a central feature. Less-typical symptoms may occur in older adults, patients with diabetes, patients with chronic renal failure, and women. Despite the absence of classic symptoms, these patients are at significant risk for complications with ACS. The characterization of this discomfort, location, severity, frequency, and possible radiation of pain help to identify the patient with ACS. The patient’s age, sex, family history of coronary artery disease (CAD), smoking, dyslipidemia, hypertension, diabetes, previous CAD, and cocaine use also tend to increase the pretest likelihood of ACS in the individual presenting to the ED. The differential diagnosis for patients with potential ACS should include pulmonary embolism, aortic dissection, parenchymal lung disease, esophageal reflux, biliary disease, psychiatric illnesses including depression and panic disorder, musculoskeletal pain, and trauma. Part of the patient’s history should assess for underlying illnesses such as intracranial tumor, gastrointestinal or other major bleeding, aortic dissection, and hemorrhagic stroke or a major surgery in the previous 2 weeks that can make antithrombotic or antiplatelet therapy potentially dangerous.
The physical examination for patients suspected of having ACS must focus on features associated with high risk for nonfatal myocardial infarction or death. Evidence of cardiogenic failure increases the likelihood that ACS is the cause of the patient’s
symptoms. These symptoms may include jugular venous distension, rales, cardiac murmurs, S3 or S4 gallops, peripheral edema, a new mitral regurgitation murmur, hypotension (systolic blood pressure <100 mm Hg), tachycardia (pulse >100 bpm), and bradycardia (pulse <60 bpm). An important aspect of the physical examination that must not be minimized is the thorough evaluation for evidence of gross gastrointestinal bleeding or other reasons for contraindications to administering antithrombotic or antiplatelet therapy (Fig. 5-1).
symptoms. These symptoms may include jugular venous distension, rales, cardiac murmurs, S3 or S4 gallops, peripheral edema, a new mitral regurgitation murmur, hypotension (systolic blood pressure <100 mm Hg), tachycardia (pulse >100 bpm), and bradycardia (pulse <60 bpm). An important aspect of the physical examination that must not be minimized is the thorough evaluation for evidence of gross gastrointestinal bleeding or other reasons for contraindications to administering antithrombotic or antiplatelet therapy (Fig. 5-1).
Table 5-1. ACC/AHA Classification of Recommendations and Levels of Evidence | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
In the assessment of the potential ACS patient, the 12-lead ECG is one of the most important pieces of information the physician will obtain. The ECG is often, and should be, obtained very early in the patient’s presentation to the ED, ideally within 10 minutes after the patient’s arrival. Many EDs have protocols in place in which the ECG may be obtained prior to a physician’s assessment based on the patient’s presenting symptoms. ST-segment depression has been shown to be a significant risk indicator for mortality and MI (10). Approximately half of the patients with ST-segment depression will develop MI within hours after presentation to the ED. Transient ST-segment elevation also portends high risk for the patient, likely signifying transient coronary artery occlusion by thrombus. Patients with new T-wave inversion on the initial 12-lead ECG have a less-adverse prognosis in patients with ACS as compared to ST-segment depression. Approximately 5% of these patients will have an MI or die within 30 days. Bundle-branch blocks that are new or presumed to be new can indicate a high-risk presentation in the emergency setting. A new bundle-branch block, which serves as a criterion for STEMI in the appropriate clinical setting such as prolonged ischemic chest pain, indicates a need for rapid reperfusion therapy. Old bundle-branch blocks are more challenging to interpret in the setting of patients with suspected ACS. The old bundle-branch blocks may suggest underlying coronary disease; however, they also may indicate primary conduction system disease. Finally, patients with a paced rhythm can be a challenge when it comes to diagnosing ACS. The paced rhythm may mask underlying electrocardiographic high-risk features. A normal 12-lead ECG on presentation to the ED does not rule out ACS. Although a normal ECG represents the lowest risk for a given patient, up to a 6% rate of NSTEMI still exists for these patients. The initial ECG results, therefore, provide the clinician with substantial risk stratification information. The ACC/AHA guidelines support obtaining serial 12-lead ECGs in the ED to improve sensitivity for detecting ACS if the initial ECG is nondiagnostic (3).
After the ECG is obtained, blood is obtained from the patient. A complete blood count, renal profile with creatinine, PT/INR, PTT, and cardiac biomarkers are the standard labs ordered. The cardiac biomarkers troponin (I and T) and CK-MB represent the second principal method for identifying patients with ACS at risk for significant complications. Although CK-MB has been the predominant marker of myocardial necrosis used in the past, the troponins I and T in many centers have replaced this traditional marker in accordance with the recent criteria for the redefinition of acute MI promulgated by the European Society of Cardiology and the ACC (11,12,13,14,15). During the last decade, numerous studies have demonstrated that any detectable elevation of troponin identifies patients at high risk for ischemic complications, including patients with renal failure (16,17). Elevated troponin in the setting of ischemic symptoms indicates that the patient has experienced the myocardial necrosis of MI. Elevation of troponin is associated with increased risk of death, and the risk of this complication increases proportionately with the absolute level (18). Like the 12-lead ECG, troponin serves as an independent predictor of substantial patient risk. Studies also have confirmed that patients with ACS and elevated troponins derive greater benefit from treatment with platelet glycoprotein (GP) IIb/ IIIa inhibitors, low-molecular-weight heparin, and early percutaneous coronary intervention (PCI) than those not having elevated troponin levels. It should be emphasized that a normal level of troponin (or CK-MB) on ED presentation, particularly within 6 hours of chest pain onset, does not exclude MI. Serial testing in the ED at 0, 3, and 6 hours and at an interval of 6 to 10 hours once in hospital is necessary to exclude myocardial injury. It should also be noted that an elevated troponin is indicative of cardiac injury but not necessarily ischemic cardiac injury (19). If the clinical presentation is not one of acute ischemic heart disease, then a careful search for alternative causes of cardiac injury is essential, such as congestive heart failure or pulmonary embolus.
Point-of-care testing (POCT) of cardiac markers is becoming more popular in the emergency setting. The benefits of POCT are both speed to diagnosis and to therapy. Point-of-care testing typically accelerates decision making in the ED by providing CK-MB and troponin levels within 15 to 20 minutes after presentation (20). An added benefit is that these results are often directly handed to the treating physician, thus eliminating postlaboratory analysis delays. Many point-of-care devices, however, are less sensitive than are central laboratory analyzers, and thus some patients with minor and/or modest
elevations in troponin may be missed (21). When central laboratory testing is used, the turnaround time for laboratory results should not exceed 1 hour (3). This 1-hour time period refers to the time the blood is drawn to the time the physician is aware of the results. This time interval has been referred to as “vein-to-brain.” This information for ED evaluation is summarized in Figure 5-1.
elevations in troponin may be missed (21). When central laboratory testing is used, the turnaround time for laboratory results should not exceed 1 hour (3). This 1-hour time period refers to the time the blood is drawn to the time the physician is aware of the results. This time interval has been referred to as “vein-to-brain.” This information for ED evaluation is summarized in Figure 5-1.
For the patient with suspected ACS that has a nondiagnostic ECG and normal levels of cardiac biomarkers, what other diagnostic modalities are available to the treating physician for help in the risk stratification of the patient? Tests such as echocardiography for wall motion abnormality, contrast echocardiographic perfusion imaging, and radionuclide perfusion imaging with agents such as sestamibi can be performed at rest, providing compelling risk stratification information for patients presenting to the ED. When performed while the patient is complaining of chest pain or within several hours after discomfort has ceased, these studies can provide excellent negative predictive value for acute myocardial ischemia. Patients with chronic ECG changes such as bundle-branch block or ST-segment/T-wave abnormalities also can be evaluated more extensively using these modalities. The routine use of these diagnostic techniques at a given hospital depends on the availability of cardiologists or nuclear radiologists at the hospital and the particular interests and expertise of the cardiologists or nuclear radiologists at the institution. Standard graded exercise testing and stress echocardiography can be performed in patients with nondiagnostic ECGs, negative cardiac biomarkers, and no recent (<6 hours) pain at rest; however, exercise testing is contraindicated in patients with acute ischemia. Discharge of a patient from the ED may be appropriate for patients without high-risk features presenting to the ED, negative serial cardiac biomarkers, no evidence of ST-segment or T-wave changes, and a negative perfusion imaging test at rest. Careful follow-up by cardiology as an outpatient is necessary so that provocative testing can be performed to rule out a fixed coronary lesion causing crucial stenosis.
The practical implementation of the 2002 ACC/AHA UA/NSTEMI guidelines approach provides an algorithm for the evaluation and management of patients suspected of having an ACS in the ED (Fig. 5-2) (7,8). This information should provide the foundation for any critical pathway developed for ACS/NSTEMI patients. In addition to routine therapy, such as continuous cardiac monitoring, oxygen if needed, and intravenous access, the following therapies are recommended by the 2002 ACC/AHA guidelines: nitrates, morphine, beta-blockers, nondihydropyridine calcium channel blockers (verapamil or diltiazem), ACEIs, antiplatelet agents, and antithrombin agents. Each of these will be reviewed later.
Nitrates, a Class IC recommendation, should be given first by the sublingual route followed by intravenous administration for the relief of ischemia and its associated symptoms. Although there are no randomized, placebo-controlled clinical trials of nitrate use in unstable angina, there are small studies from the prethrombolytic era that suggest a reduction in mortality rate of approximately 35%. As a result of no adequate studies for the use of nitrates in NSTEMI, the recommendations are largely extrapolated from pathophysiological principles and uncontrolled observations (22).
Like the nitrates, morphine is a Class IC recommendation and has no randomized, placebo-controlled clinical trials to support its use. Morphine sulfate remains a recommendation because of its venodilation properties and modest reductions in heart rate. It also may be used to help relieve a patient’s anxiety or when acute pulmonary congestion is also present.
The intravenous administration of beta-blockers, a Class IB recommendation, should be used when there is ongoing chest-pain without contraindications to beta-blockade and the patient is not already taking beta-blockers before presentation. An overview of double-blind, randomized, controlled trials in patients with threatening or evolving MI suggests an approximately 13% reduction in risk of progression to MI for patients. There are no trials with sufficient power to evaluate beta-blockade in patients with unstable angina; however, the proven efficacy of beta-blockers in patients with acute MI, recent acute MI, congestive heart failure, and angina led to their use as being recommended in unstable angina (23). Nondihydropyridine calcium channel blockers, a Class IB recommendation, are recommended in patients with continuing or frequently recurring ischemia when beta-blockers are contraindicated and there is no left ventricular (LV) dysfunction, hypotension, or other contraindication to their use. When administered to patients with LV dysfunction, there is strong evidence that they are detrimental (Class III) (24,25,26).
ACEIs are a Class IB recommendation. ACEIs are recommended when hypertension persists despite treatment with nitroglycerin and beta-blockers in patients with LV systolicdysfunction or congestive heart failure. They are also recommended for patients with ACS and diabetes. Initiation of ACEIs in the ED is appropriate in the preceding circumstances; however, it is not necessary that this agent be started in this setting. Angiotensin renin blockers can be substituted if the patient is ACEI intolerant (27,28,29).
Antiplatelet agents that inhibit the aggregation of platelets play an important role in the prevention of thrombosis in the 2002 ACC/AHA UA/NSTEMI guidelines. Three different classes of agents have distinct and separate mechanisms of action: aspirin, clopidogrel, and the GP IIb/IIIa receptor inhibitors. Each will be discussed separately because of these important different mechanisms of action.
Aspirin, an inexpensive and effective antiplatelet agent, acts by blocking the thromboxane A2 pathway. Aspirin is a Class IA recommendation and should be administered to the ACS patient as soon as possible. It is now common practice for prehospital care providers to administer this drug prior to the patient’s arrival in the ED. Several studies have shown aspirin to be beneficial in the setting of ACS, showing an approximately 50% reduction in death and MI in patients receiving this therapy (3,30,31).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree