Table 3.1 Common Clinical Questions.
| Common clinical questions | Primary modality | Secondary modalities |
| What is the LVEF? | TTE, MUGA | CT, CMR, PET |
| Are wall motion abnormalities present? | TTE | PET, CMR |
| Does my patient have coronary artery disease? | CTA Stress testing | MRA, CTA, |
| Are congenital abnormalities present? | TTE | CT, CMR |
| Does my patient have valvular disease? | TTE | TEE (invasive) |
| Are the pacemaker/defibrillator leads in the right place? | CXR | CT |
| Does my patient have constrictive or restrictive cardiomyopathy? | TTE | CMR, CT |
| Is the pericardium normal? | CT, CMR | CXR |
| Does my patient have aortic dissection? | CT TEE (invasive) | CMR |
| Does my patient have evidence of myocardial viability? | PET | CMR |
Not all tests are appropriate for all patients. In addition to knowing the clinical question, it is useful to review relative and absolute contraindications to imaging modalities prior to choosing a specific study for a particular patient. In this chapter, we focus on non-stress test-related imaging studies as stress tests are discussed elsewhere.
3.2 NON-STRESS IMAGING STUDIES
3.2.1 Chest X-Ray (CXR)
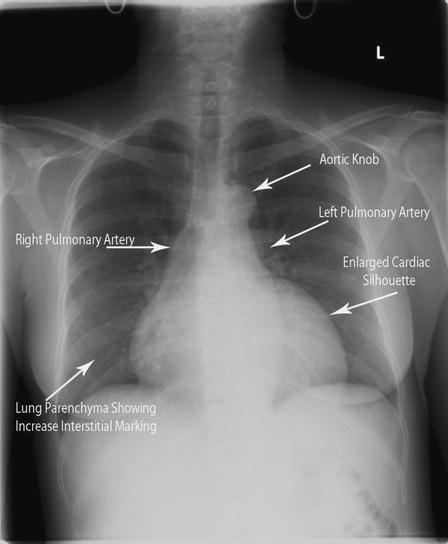
The CXR offers valuable but often nonspecific information on cardiovascular disease (Table 3.2). CXR is indicated in any patient with suspicion of structural heart or lung disease. CXR can be performed at the bedside (standard anterior-posterior (AP) projection) or in a radiology lab (standard posterior-anterior (PA) projection and lateral projections). PA CXR is generally more accurate, as the standard 6-foot projection length allows for clearer resolution of borders (Figure 3.1). In addition, most PA CXRs are performed at end-inspiration for maximum delineation of structures; this is difficult to achieve in an AP projection with the patient lying in a hospital bed.
Table 3.2 CXR.
| Indications | Heart and lung disease; pericardial evaluation |
| Contraindications | Pregnancy (relative) |
| Key structures visualized | Cardiac silhouette, lung parenchyma, ascending aorta silhouette, pericardial calcification |
| Key structures not visualized | Individual chambers of heart, valves |
| Limitations | No information on cardiac motion of hemodynamics Body habitus or patient positioning can lead to poor image quality |
CXR is most useful in the diagnosis of congestive heart failure, primarily by demonstrating evidence of pulmonary congestion (pleural effusions, Kerley B lines, and pulmonary edema), pericardial disease (pericardial calcifications), aortic dissection (enlarged mediastinum), pulmonary hypertension (enlarged pulmonary arteries), and complications of cardiac procedures (pneumothorax, hemothorax). It has a high sensitivity for pneumothorax and hemothorax post-cardiovascular procedures. CXR is also useful for determining location of pacemaker leads and other intravenous catheters. CXR can be helpful in assessing left ventricular dilation, although AP CXR, as compared to PA CXR, tends to overestimate true heart size.
3.2.2 Echocardiography (TTE and TEE)
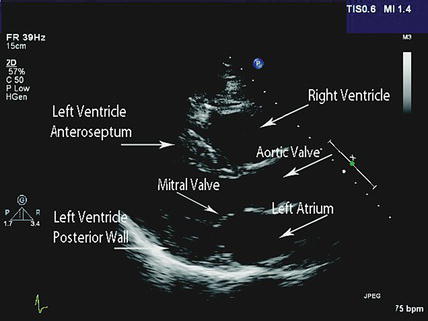
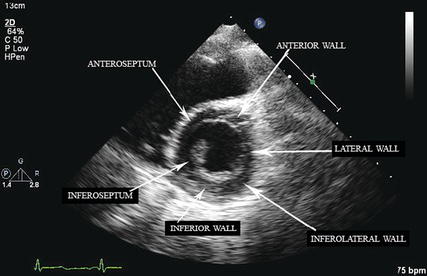
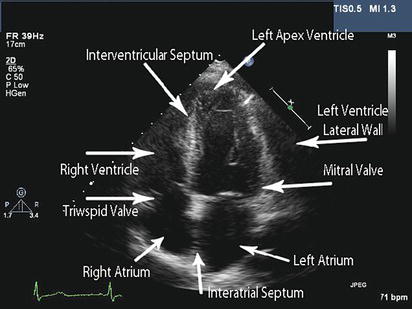
Transthoracic echocardiography (TTE) is the modality of choice for initial evaluation of cardiovascular structure, function, and hemodynamics (Table 3.3). Transthoracic echocardiography is a real-time 2D ultrasound of the heart and the reflection of ultrasound beams from cardiac structures offers information on their anatomy and motion (Figure 3.2, Figure 3.3, Figure 3.4).
Standard 2D images are acquired from multiple projections and typically consist of parasternal, apical, subcostal, and suprasternal views. In addition to real-time 2D images, Doppler imaging adds information on cardiovascular hemodynamics. Color Doppler imaging is used for assessment of myocardial blood flow and can identify pressure gradients. Pulse wave Doppler and continuous wave Doppler can accurately quantify velocities along a linear path in the ultrasound beam, which can then be used to estimate pressure gradients.
A TTE is very beneficial for the diagnosis of valvular disease, wall motion abnormalities that suggest coronary artery disease, cardiomyopathy, ascending aortic disease, valvular disease, and congenital defects (ventricular septal defect, atrial septal defect, patent foramen ovale). Agitated saline contrast given through a peripheral vein can also delineated intrapulmonary versus intracardiac shunts. Doppler imaging can be used to identify valvular stenosis, valvular regurgitation, and other intracardiac gradients including pulmonary artery pressures and left ventricular outflow tract obstruction. TTE can also be used to estimate or calculate left ventricular ejection fraction (LVEF). Finally, it is valuable for identifying the presence of pericardial fluid and its potential hemodynamic effects on cardiac structures.
Table 3.3 TTE.
| Indications | Structure, function, and hemodynamics |
| Contraindications | None |
| Key structures visualized | All heart chambers, all valves, ascending aortic root, aortic arch, pericardium, ventricular septum, inter-atrial septum |
| Key structures not visualized | Left atrial appendage, distal aorta |
| Limitations | Body habitus with poor image quality Inability to visualize entire aorta to exclude aortic dissection Inability to visualize left atrial appendage to exclude thrombus |
There are no contraindications to TTE and no known risks of cardiac ultrasound. However, TTE may be limited by poor image quality often seen in patients with obesity or lung disease. There are also important structures that TTE cannot fully assess, such as the left atrial appendage. It also is limited in examining the entire ascending aorta, aortic arch, and descending aorta with sufficient sensitivity required to exclude aortic dissection. Finally, imaging artifacts can occur during TTE acquisition and hamper interpretation of adjacent cardiac structures.
TTE has become routinely applied in clinical care and incidental findings are often reported. In general, referral to a cardiologist is warranted for moderate valve disease with symptoms, severe valve disease even in the absence of symptoms, cardiomyopathy, or congenital abnormality with symptoms or enlargement of the heart.
Transesophageal echocardiography (TEE) offers supplemental information to TTE. TEE is indicated for evaluation of valvular disease if an etiology is not well elucidated by TTE; this is particularly true when examining the mitral valve. It is also one the tests of choice for primary diagnosis of aortic dissection. TEE is the gold standard to assess for thrombus in the left atrial appendage as part of the evaluation of thromboembolic risk prior to cardioversion of atrial flutter or fibrillation. Finally, it is considered the test of choice in patients with concern of endocarditis or intracardiac mass given its superior visualization of valvular structures.