Neurologic Effects of Cardiopulmonary Bypass
Eduardo S. Rodrigues
David J. Cook
This chapter will provide an overview of the neurologic effects of cardiac surgery and cardiopulmonary bypass. First, the extent and nature of bypass-related neurologic injury will be presented, emphasizing the importance of patient demographics and comorbidities. In this context etiologies will be considered. Second, basic cerebral physiology during cardiopulmonary bypass will be reviewed. Third, interventions having the potential to reduce neurologic morbidity will be considered and fourth, the applicability of neurologic monitoring techniques for cardiopulmonary bypass will be briefly presented.
THE POPULATION AT RISK, DEMOGRAPHICS, AND COMORBIDITIES
Cardiac operations requiring cardiopulmonary bypass (CPB) are among the most commonly performed surgical procedures in Europe and North America. Studies describing more than 20,000 cardiac surgical patients indicate that significant morbidity may be experienced by 20% to 25% of patients (1,2,3). These morbidities include cardiac and pulmonary failure, neurologic injury, renal insufficiency, bleeding, and infection. Complications have predictable adverse effects on duration and cost of hospitalization (4,5,6) as well as on patient quality of life and functional capacity on discharge (6,7,8).
When considering cardiac surgical neurologic morbidity, it is important to understand that many adult cardiac surgical patients have preexisting risk factors for stroke and cognitive impairment even without the added risk of cardiac surgery and CPB. Cardiac or noncardiac surgery superimposes incremental risk. The recent European study of cognitive outcomes after noncardiac surgery superbly illustrated this risk (9). In that study, 1,218 elderly patients having major noncardiac surgery underwent neurocognitive assessment preoperatively, before discharge, and at 3 months postoperatively. A large (n = 321) nonsurgical control group was also enrolled. That study reported a 26% incidence of cognitive dysfunction 1 week after surgery and a 10% incidence at 3 months. Cardiac surgery poses greater risks because cardiac surgical patients experience more serious neurologic morbidity than age- and health-matched controls undergoing noncardiac surgery (Table 15.1) (8). Consequently, it is useful to regard the perioperative period as one of acute neurologic stress in a subpopulation chronically at risk.
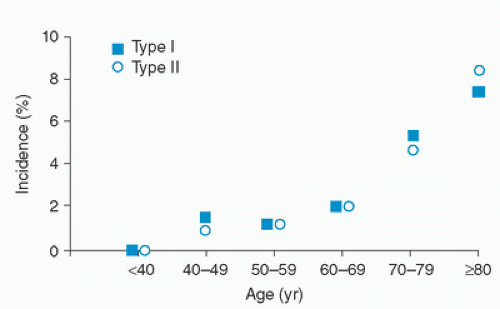
There is general agreement about preoperative patient-related factors that increase the likelihood of perioperative stroke, but the role of many intraoperative factors is much less clear. Preoperative risk factors include advanced age, history of prior neurologic events, aortic atherosclerosis, low cardiac output states, atrial arrhythmias, hypertension, and diabetes. Advanced age, the most dramatic risk factor, appears to magnify the other risk factors. The importance of this risk factor cannot be overemphasized, because over the last two decades the number of cardiac surgery patients over age 60 doubled and the percentage of patients over age 70 increased 7-fold (10). The proportion of cardiac surgical patients over age 80 will grow faster than any other group. Age alone is an independent risk factor for stroke, with patients under age 60 having ≤1% incidence of stroke across studies (1,10,11), while those over age 70 have a 4% to 9% incidence of stroke or coma following operation (Fig. 15.1) (1,10,11,12). This is
important because the increasing age of the surgical population and the successes provided by the initial heart surgery are increasing the incidence of redo heart surgery (13) which is known to increase neurologic risk. In a recent multicenter, retrospective study, Biancari et al. (14) evaluated the risk factors for stroke in a population undergoing redo heart surgery. This study included seven centers in three different European countries with a total of 741 patients. The overall incidence of stroke was 6.5%, but extremely variable depending on patient gender and perioperative events.
important because the increasing age of the surgical population and the successes provided by the initial heart surgery are increasing the incidence of redo heart surgery (13) which is known to increase neurologic risk. In a recent multicenter, retrospective study, Biancari et al. (14) evaluated the risk factors for stroke in a population undergoing redo heart surgery. This study included seven centers in three different European countries with a total of 741 patients. The overall incidence of stroke was 6.5%, but extremely variable depending on patient gender and perioperative events.
TABLE 15.1. Severity of postoperative neuropsychological deterioration in CABG and surgical control patients | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
As the surgical population has aged, the proportion of patients with multiple risk factors for neurologic injury has increased. Hypertension and diabetes occur in approximately 55% and 25% of cardiac surgical patients (10,15,16,17,18,19). Fifteen percent demonstrate ≥50% carotid stenosis and up to 13% may have had a TIA or prior stroke (15,19). When compared to previous cardiac surgical patients, these intercurrent diseases may double the risk of perioperative stroke for the present and future patients (10,20).
The Cardiovascular Health Study (CHS) enhances appreciation for preexisting cerebral morbidity and cerebral risk in the general population (21). In that investigation, a community population of 3,360 individuals over 65 years of age underwent MRI. Of these, 31% had “silent” cerebral infarcts (21). These infarcts were primarily subcortical, lacunar, and strategically placed or small enough so that clinical signs of stroke were not evident. However, detailed neurologic testing suggested the possibility that these infarcts may have accounted for cognitive and gait abnormalities (21). These lesions likely are related to chronic hypertension, which narrows the penetrating vessels supplying deep white matter, thereby rendering these regions vulnerable to focal ischemia (22,23). This type of cerebral vascular disease is clearly linked to late-onset dementia (24,25).
These findings have implications for the cardiac surgical population. Of the 5,888 men and women enrolled in the CHS, those who underwent MRI were “younger… and were more likely never to have smoked and less likely to have prior cardiovascular disease, hypertension … and diabetes than those who did not undergo scanning” (21,26). As such, the cardiac surgical population probably has an incidence of preexisting “silent” cerebral infarction in excess of 31%. One study of 31 neurologically asymptomatic CABG patients reported a 16% incidence of thromboembolic infarcts and a 58% incidence of lacunar infarcts on preoperative MRI (27).
In addition to the clear predisposition of chronic cerebrovascular disease to adverse neurologic outcome in cardiac surgery, investigation into other patient factors that may determine or modulate brain outcomes continues. Females tend to have worse neurologic outcomes (14,28,29), perhaps in part because of referral bias and small vessel size, but genetic sexlinked factors may also play a role (16,30). Another active area of investigation is genomics. To date, only apolipoprotein E4 (ApoE4) has been the subject of significant investigation in cardiac surgical outcomes (31,32,33,34,35). ApoE4 is a protein that plays an important role in cholesterol transport and metabolism, with three common alleles resulting in E2, E3, and E4 isoforms (36). The apolipoprotein alleles define a spectrum of LDL (low-density lipoprotein) cholesterol levels (37). Of the isoforms, the ApoE4 allele has a clear link to the development of atherosclerosis, cerebrovascular disease, and dementia (37,38,39,40).
In cardiac surgical patients, the relationship of patient factor ApoE4 to cerebral autoregulation (33), inflammatory cytokines (35), as well as markers of brain injury S100 and neuron-specific enolase (NSE) has been investigated (31). Because the absence of ApoE4 has been linked to better recovery from neurologic injury, the most interesting investigation to date was by investigators from Duke University who identified an association of the ApoE4 allele with worse cognitive outcomes in 65 patients who underwent cardiac surgery (32). However, the frequency of the E4 allele was only 13%; so the study was underpowered. Additionally, the authors (32) point out that an association of E4 and adverse neurologic outcomes, or markers of neurologic outcomes (31,36), might simply be related to a greater burden of atherosclerotic disease in the E4 patients rather than a more specific interaction of the gene and neurologic outcome.
Neurologic Complications in Cardiac Surgery
Neurologic injury following cardiac surgery has been a source of concern since its inception and this injury can be generally divided into frank stroke, encephalopathy, and neurocognitive disorders. The incidence of major neurologic morbidity related to cardiac surgery is 1% to 6% (5,11,14




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree