Neuroblastoma, Ganglioneuroblastoma, and Ganglioneuroma of the Mediastinum
Borislav A. Alexiev, M.D.
Jennifer M. Boland, M.D.
Allen P. Burke, M.D.
Introduction
Neural tumors constitute 15% of mediastinal tumors in adults, and around one-third in children. They are almost always in the posterior mediastinum.1,2 In children, 80% of mediastinal neural tumors are neuroblastomas or ganglioneuroblastomas, whereas in adults, most are benign peripheral nerve sheath tumors (see Chapter 134) and ganglioneuromas.1,2
Neuroblastoma and Ganglioneuroblastoma
Classification
The neuroblastic and schwannian stromal cells in neuroblastoma are derived from genetically identical neoplastic cells and support the classical paradigm that neuroblastoma arises from tumoral cells capable of development along multiple lineages.3
The neuroblastic tumors are a family of neoplasms composed of various degrees of immature and maturing neural elements. The International Neuroblastoma Pathology Committee has adopted a prognostic system for neuroblastic tumors modeled on the classification proposed by Shimada et al.4 It is an age-linked risk stratification system dependent on the degree of differentiation observed in the neuroblasts (if present), the cellular turnover index in the neuroblastic component (mitosis- karyorrhexis index), and the presence or absence of schwannian stromal development.4,5,6
Based on morphologic criteria, neuroblastic tumors are classified into four categories: (1) neuroblastoma (schwannian stroma-poor); (2) ganglioneuroblastoma, intermixed (schwannian stroma-rich); (3) ganglioneuroblastoma, nodular; and (4) ganglioneuroma (schwannian stroma-dominant).
Neuroblastomas are defined as neuroblastic, schwannian stroma-poor tumors, although scattered Schwann cells can be detected in the fibrovascular septa demarcating more- or less-defined lobules of neuroblastic cells.5,6 By definition, the proportion of tumor tissue with schwannian stroma-rich histology should not exceed 50%.4
Ganglioneuroblastomas have identifiable nests or nodules of neuroblasts and have schwannian stroma that constitutes >50% of the tumor. Ganglioneuroblastomas can be further subcategorized into intermixed type (randomly distributed nests of neuroblastic cells in varying stages of development in a background of schwannian stroma) or nodular type (one or more clonal nodules of neuroblasts in a background of ganglioneuroma-like or intermixed ganglioneuroblastoma-like tumor).
The neuroblastic component of neuroblastoma and nodular ganglioneuroblastoma should be further subclassified based on degree of differentiation. The undifferentiated subtype has no neuropil and no recognizable differentiation based on morphology (entirely small round blue cells). The poorly differentiated subtype has neuropil in the background of the tumor, with <5% of cells composed of differentiating neuroblasts (resembling ganglion-like cells, vesicular chromatin with prominent nucleoli and more ample cytoplasm). The differentiating subtype is composed of >5% differentiating neuroblasts, sometimes accompanied by mature ganglion cells.
Incidence and Clinical
Neurogenic tumors can arise from neural cells in any location; however, they commonly are found in the mediastinum (15.3%).7 The posterior mediastinum is the second most common primary site for neuroblastoma and ganglioneuroblastoma (after the adrenals/abdominal paravertebral sympathetic chain).8
Neuroblastoma commonly occurs in children but is rare in adults.9 Approximately one in six pediatric neuroblastomas occur in the mediastinum, the majority of the remainder occurring in the abdomen.10
The median age at presentation is 0.9 years, with 42% of patients presenting at <1 year of age.11 There is a slight female predominance.12 A posterior mediastinal mass is diagnosed on incidental chest roentgenograms performed for non-tumor-related symptoms in 49% of the cases. The patients may present with neurologic symptoms, acute respiratory distress, and elevated urinary catecholamines. Less common presentations include Horner syndrome and opsoclonus-myoclonus.13
Gross Pathology
Neuroblastoma is typically tan-grey with invasive margins. Tumors often show hemorrhagic and necrotic regions with calcifications.
Microscopic Pathology
Neuroblastomas are histologically separated from ganglioneuroblastomas by the proportion of neuroblasts and schwannian stroma: neuroblastomas have >50% neuroblasts (<50% schwannian stroma), while ganglioneuroblastomas have <50% neuroblasts (>50% schwannian stroma). Neuroblastomas and ganglioneuroblastomas should be subtyped into one of the following categories based on histologic characteristics4:
Neuroblastoma, undifferentiated subtype is composed of undifferentiated small to medium-size cells with round or elongated nuclei and “salt-and-pepper” chromatin, distinct nucleoli, and scant cytoplasm. Identifiable background neuropil is absent.
Neuroblastoma, poorly differentiated subtype is a tumor with background of neuropil (Fig. 135.1). Most tumor cells appear undifferentiated; only 5% or less of the tumor cell population has morphologic features of differentiation towards ganglion cells.
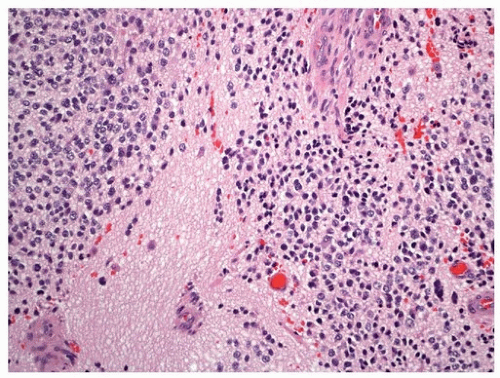
FIGURE 135.1 ▲ Neuroblastoma, poorly differentiated subtype. Note background of neuropil and absence of ganglion cells.
Neuroblastoma, differentiating subtype has abundant neuropil, with 5% or more of the tumor cells showing differentiation towards ganglion cells.
Ganglioneuroblastoma, intermixed (schwannian stroma-rich) shows a transitional appearance, often seeming to be on its way toward full differentiation/maturation; however, the process is not complete, as evidenced by scattered microscopic foci of neuroblastic cells, which occur in small nests, admixed with the schwannian stroma. The proportion of ganglioneuromatous component to neuroblastic foci should exceed 50% of the tumor volume.
Ganglioneuroblastoma, nodular (composite schwannian stroma-rich/stroma-dominant and stroma-poor) is composed of macroscopic, usually hemorrhagic neuroblastic nodule(s) (stroma-poor) coexisting with ganglioneuroblastoma, intermixed (schwannian stroma-rich) or ganglioneuroma (schwannian stroma-dominant) components. The term composite implies that the tumor is composed of biologically different clones.
Neuroblastomas are composed of neuroblasts exhibiting variable degrees of differentiation up to ganglion cells. Neuroblasts have small round nuclei with stippled (“salt and pepper”) chromatin, distinct nucleoli, scant eosinophilic cytoplasm, and indistinct cell borders. Scattered large cells with nuclei 1.5 to 2 times larger than those of typical neuroblasts are usually seen in the undifferentiated and poorly differentiated subtypes of neuroblastoma.14 Ganglion cells have large round nuclei with prominent nucleoli and abundant eosinophilic cytoplasm with Nissl substance (basophilic granules/bodies composed of endoplasmic reticulum). The tumoral background stroma also shows different levels of differentiation, and may consist of neuropil (pink, fibrillary extracellular material) and/or spindle cell schwannian stroma. Calcifications and dense lymphoid infiltrates are occasionally present. One characteristic feature of neuroblastoma is the formation of Homer-Wright rosettes, which are circular or ovoid collections of tumor cells arranged around a central core of neuropil. Homer-Wright rosettes are typical of neuroblastoma, but they are not always present.
The mitosis-karyorrhexis index (MKI) (number of mitoses and karyorrhectic nuclei per 5,000 neuroblastic cells) is a useful prognostic indicator and should be determined as an average of all tumor sections available.5,6 According to the International Neuroblastoma Pathology Classification, morphologic features (grade of neuroblastic differentiation and MKI) along with patient’s age at the time of diagnosis are taken into account for the prognostic distinction of neuroblastoma into favorable histology or unfavorable histology groups.5,6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


