Neoplastic disorders
Neoplastic growths may be benign or malignant, depending on their ability to invade and metastasize to other areas of the body. Neoplastic thoracic disorders include laryngeal and lung cancer, and mesotheliomas.
LARYNGEAL CANCER
Squamous cell carcinoma constitutes about 95% of laryngeal cancers. Rare laryngeal cancer forms—adenocarcinoma and sarcoma—account for the rest. The disease affects males about nine times more commonly than females, and most patients are between ages 50 and 65.
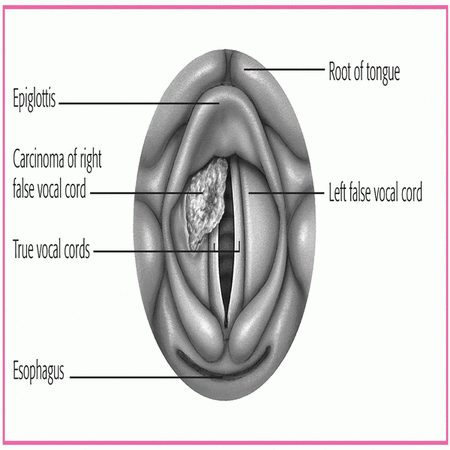
Patterns of metastasis in laryngeal cancer reflect the organ anatomy. Tumors of the glottis (true vocal cords) tend to remain localized because the underlying tissues lack lymph nodes. Supraglottic tumors, however, typically spread through the lymphatics to adjacent areas. Although these tumors can metastasize to distant sites, such as the lungs, localized disease may threaten survival because of airway problems. (See A look at laryngeal cancer, page 356.)
The cause of laryngeal cancer is unknown. Major risk factors include smoking and heavy alcohol consumption. Minor risk factors include chronic inhalation of noxious fumes and familial disposition.
Laryngeal cancer is classified by its location:
supraglottis (false vocal cords)
glottis (true vocal cords)
subglottis (rare downward extension from vocal cords).
Pathophysiology
Initially, the mucosa is exposed to an irritating substance and develops into a tougher mucosa by increasing its thickness or by the development of a keratin layer. Cellular changes also lead to the growth of abnormal epithelial cells that eventually become malignant. These areas of epithelial cells are commonly white and patchy or red and patchy. Metastasis of cancer of the head and neck depends on the primary site of the tumor and usually spreads to the mucosa, muscle, and bone. Systemic metastasis through the blood and lymphatic system is also possible. When this occurs, it’s typically to the lung or liver.
Complications
Increasing dysphagia
Pain
Airway obstruction
Assessment findings
Varied assessment findings in laryngeal cancer depend on the tumor’s location and its stage.
STAGE I
With stage I disease, the patient may complain of local throat irritation or hoarseness that lasts about 2 weeks.
STAGES II AND III
In stages II and III, he usually reports hoarseness.
He may also have a sore throat, and his voice volume may be reduced to a whisper.
STAGE IV
In stage IV, he typically reports pain radiating to his ear, dysphagia, and dyspnea.
In advanced stage IV disease, palpation may detect a neck mass or enlarged cervical lymph nodes.
Diagnostic test results
Biopsy identifies malignant cells.
Chest X-ray identifies metastasis.
Laryngoscopy allows definitive staging by obtaining multiple biopsy specimens to establish primary diagnosis, to determine the extent of the disease, and to identify additional premalignant lesions or second primary lesions.
Xeroradiography, laryngeal tomography, computed tomography scan, and laryngography confirm the presence of a mass.
Treatment
Early lesions may respond to laser surgery or radiation therapy; advanced lesions to laser surgery, radiation therapy, and chemotherapy. Treatment aims to eliminate cancer and preserve speech. If speech preservation isn’t possible, speech rehabilitation may include esophageal speech or prosthetic devices. Surgical techniques to construct a new voice box are experimental. (See Reviewing alternative speech methods, page 358.)
In early disease, laser surgery destroys precancerous lesions; in advanced disease, it can help clear obstructions. Other surgical procedures vary with tumor size and include cordectomy, partial or total laryngectomy, supraglottic laryngectomy, and total laryngectomy with laryngoplasty.
REVIEWING ALTERNATIVE SPEECH METHODS
During convalescence, your patient may work with a speech pathologist who can teach him new ways to speak using various communication techniques such as those below.
Esophageal speech
By drawing air in through the mouth, trapping it in the upper esophagus, and releasing it slowly while forming words, the patient can again communicate by voice. With training and practice, a highly motivated patient can master esophageal speech in about a month. Recognize that speech will sound choppy at first, but with increasing skill, words will flow more smoothly and understandably.
Because esophageal speech requires strength, an elderly patient or one with asthma or emphysema may find it too physically demanding. Because it also requires frequent sessions with a speech pathologist, a chronically ill patient may find esophageal speech overwhelming.
Artificial larynges
The throat vibrator and the Cooper-Rand device are basic artificial larynges. Both types vibrate to produce speech that’s easy to understand, although it sounds monotonous and mechanical.
Tell the patient to operate a throat vibrator by holding it against his neck. A pulsating disk in the device vibrates the throat tissue as the patient forms words with his mouth. The throat vibrator may be difficult to use immediately after surgery, when the patient’s neck wounds are still sore.
The Cooper-Rand device vibrates sounds piped into the patient’s mouth through a thin tube, which the patient positions in the corner of his mouth. Easy to use, this device may be preferred soon after surgery.
Surgically implanted prostheses
Most surgical implants generate speech by vibrating when the patient manually closes the tracheostomy, forcing air upward. One such device is the Blom-Singer voice prosthesis. Only hours after it’s inserted through an incision in the stoma, the patient can speak in a normal voice. The surgeon may implant the device when radiation therapy ends or within a few days (or even years) after laryngectomy.
To speak, the patient covers his stoma while exhaling. Exhaled air travels through the trachea, passes through an airflow port on the bottom of the prosthesis, and exits through a slit at the esophageal end of the prosthesis. This creates the vibrations needed to produce sound.
Not all patients are eligible for tracheoesophageal puncture, the procedure in which the prosthesis is inserted. Considerations include the extent of the laryngectomy, pharyngoesophageal muscle status, stomal size and location, and the patient’s mental and emotional status, visual and auditory acuity, hand-eye coordination, bimanual dexterity, and self-care skills.
Radiation therapy alone or combined with surgery is effective but can result in complications, including airway obstruction, pain, taste changes, and chronic dry mouth (xerostomia).
Chemotherapeutic agents may include methotrexate (Rheumatrex), cisplatin (Platinol-AQ), bleomycin (Blenoxane), fluorouracil (Adrucil), and paclitaxel (Taxol).
Nursing interventions
Provide supportive psychological, preoperative, and postoperative care to reduce complications and speed recovery.
Encourage the patient to discuss his concerns before surgery. Help him choose a temporary, alternative way to communicate, such as writing or using sign language or an alphabet board. If appropriate, arrange for a laryngectomee to visit him.
AFTER PARTIAL LARYNGECTOMY
Give I.V. fluids and, usually, tube feedings for the first 2 days after surgery; then resume oral fluids. Keep the tracheostomy tube (inserted during surgery) in place until tissue edema subsides.
Make sure the patient doesn’t use his voice until the physician gives permission (usually 2 to 3 days postoperatively). Then caution the patient to whisper until he heals completely.
AFTER TOTAL LARYNGECTOMY
As soon as the patient returns to his room from surgery, position him on his side, and elevate his head 30 to 45 degrees. If he has tissue flaps to close the wound, position him so that the side with the flaps isn’t dependent. When you move him, remember to support the back of his neck to prevent tension on sutures and possible wound dehiscence.
If the patient has a laryngectomy tube in place, care for it as you would a tracheostomy tube. Shorter and thicker than a tracheostomy tube, the laryngectomy tube stays in place until the stoma heals (about 7 to 10 days).
Watch the stoma for crusting and secretions, which can cause skin breakdown. To prevent crusting, provide adequate room
humidification. Remove crusts with petroleum jelly, antimicrobial ointment, and moist gauze.
Monitor vital signs. Be especially alert for fever, which indicates infection. Record fluid intake and output, and watch for dehydration. Also, be alert for and report postoperative complications. (See Recognizing and managing complications of laryngeal surgery.)
Provide frequent mouth care. Clean the patient’s tongue and the sides of his mouth with a soft toothbrush or a terry washcloth, and rinse his mouth with a deodorizing mouthwash. If a patient is receiving radiotherapy or chemotherapy, avoid alcohol
mouthwashes. Normal saline mouth rinses cleanse and maintain moisture.
Suction gently. Unless ordered otherwise, don’t attempt deep suctioning, which could penetrate the suture line. Suction through both the tube and the patient’s nose because the patient can no longer blow air through his nose. Suction his mouth gently.
After inserting a drainage catheter (usually connected to a blood drainage system or a GI drainage system), don’t stop suction without the physician’s consent. After removing the catheter, check the dressings for drainage.
Give analgesics as ordered. Keep in mind that opioid analgesics depress respiration and inhibit coughing.
If the physician orders nasogastric (NG) tube feedings, check tube placement, and elevate the patient’s head to prevent aspiration. Be ready to perform suction after NG tube removal or oral fluid intake because the patient may have difficulty swallowing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree