Fig. 17.1
Operative Set-up. A right fourth intercostal space mini-thoracotomy is used for access. Cardiopulmonary bypass is established using femoral canulation. A trans-thoracic cross clamp is used to arrest the heart. A trans-thoracic atrial retractor exposes the mitral valve and an endoscopic camera provides visualization
Anesthesia Management
Since 2006 we have used “fast track” anesthesia in our minimal invasive MV program. We have seen faster patient recovery from shorter ventilation durations. Regarding this surgical procedure, there are no additional anesthetic requirements such as single lung ventilation. We deflate the lungs only after cardiopulmonary bypass (CPB) is started.
Neochord Implantation: “Leipzig Loop Technique”
Neochord Length
It is of utmost importance to implant neochordae of correct lengths. A custom suture ruler calliper (Geister Medizintechnik GmbH, Tuttlingen, Germany) (Fig. 17.2a) is used to measure (mm) the distance between the papillary muscle body and leaflet “free margins” at chord insertion sites. This device can also be used to make the loops (Fig. 17.2b). For a reference point, we use the P1 segment routinely (Fig. 17.3). In most cases P1 does not prolapse: however, when it is redundant the MV annular plane is used as an alternative reference. Pre-fabricated PTFE loops (10–26 mm) are available in the operating room for immediate use (Fig. 17.4). Loops are pre-fabricated by our nurses using a specialized knotting device (Geister Medizintechnik GmbH, Tuttlingen, Germany) or the suture ruler shown in Fig. 17.2.
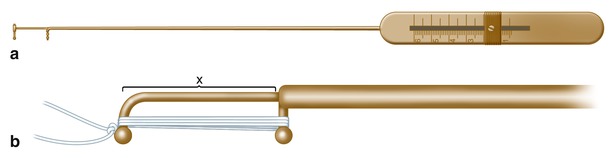
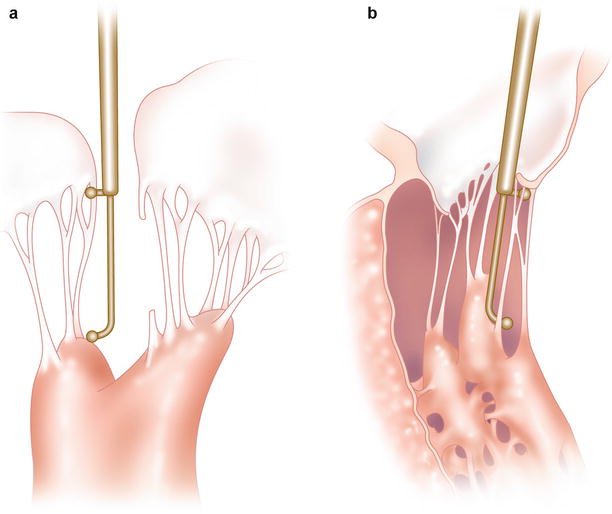
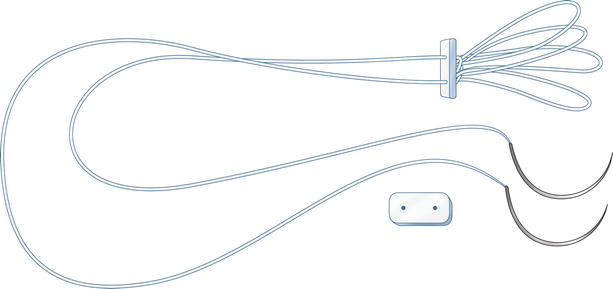
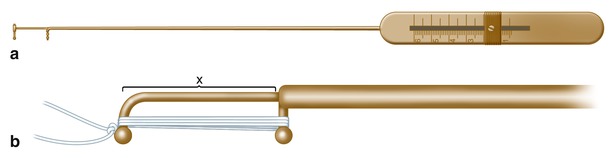
Fig. 17.2
(a) This suture ruler (mm) is used to measure the distance between papillary muscles and a non-prolapsing leaflet reference point. (b) After determining the appropriate loop lengths, the ruler can be used to fabricate the loops. Alternatively, the same company makes a facilitating “bench” apparatus
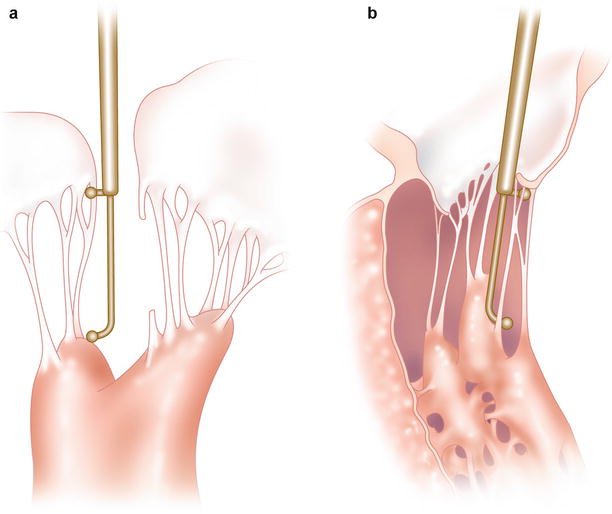
Fig. 17.3
(a) the suture ruler is measuring the distance between papillary muscle tip and a non-prolapsing leaflet reference point. The prolapsing leaflet is seen opposite the reference point. (b) In patients with a thin papillary tip the measurement should start at the mid-body to anchor the loops securely
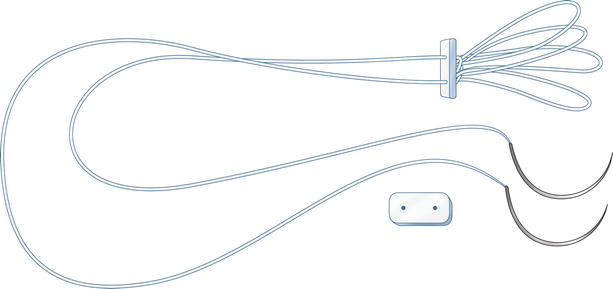
Fig. 17.4
Bundle of four loops “knot-anchored” at a small pledget
Anchoring “PTFE Loops” to Papillary Muscles
Neochord-papillary muscle security is obligatory and must mirror native chord anatomy and function. The two “base” sutures should be passed in an anterior to posterior direction through the papillary muscle in parallel and toward the respective prolapsed segment (Fig. 17.5a). The knotted end of the loop should be tied opposite the prolapsing leaflet surface (Fig. 17.5b). We have a motto, “Take it (the knot) to the other side”; thus free loop ends must arise from the papillary muscle and project toward the mitral valve orifice center. They should not cross the midline of the anterior leaflet (Fig. 17.6). Correct loop spacing must be established along the leaflet edge to avoid interaction and/or distortion of native chords. At the papillary muscle site, PTFE ends should tied be over a small felt pledget to avoid ischemia (Fig. 17.5b).
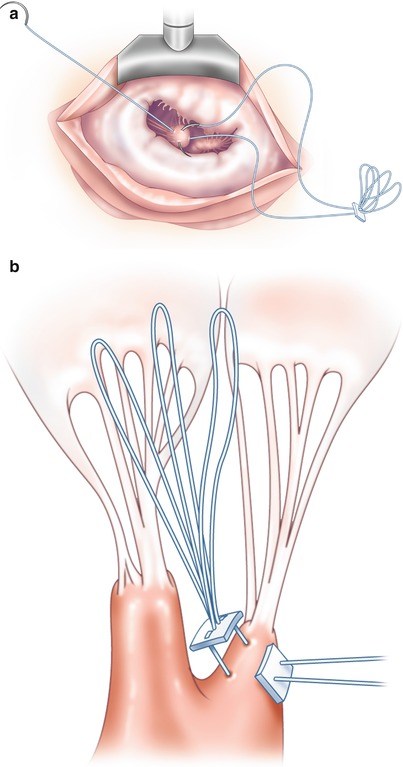
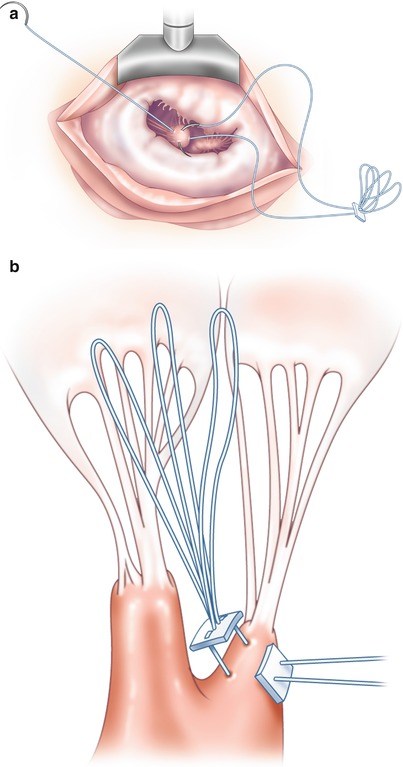
Fig. 17.5




(a) Needles from the long-end of the PFTE loop apparatus are passed in parallel through the papillary muscle in anterior-posterior direction and away and from the prolapsing leaflet. (b) A second pledget is passed over the PTFE suture and the anchoring knot tied. It is important for the “knot is on the other side” opposite of the prolapsing leaflet
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


