Although transcatheter aortic valve implantation has been available for 10 years, reports of cardiovascular morphologic studies after the procedure are virtually nonexistent. The investigators describe such findings in 2 patients, both 86 years of age, who died early (hours or several days) after transcatheter aortic valve implantation. Although the prosthesis in each was seated well, and each of the 3 calcified cusps of the native aortic valves was well compressed to the wall of the aorta, thus providing a good bioprosthetic orifice, the ostium of the dominant right coronary artery in each was obliterated by the native right aortic valve cusp. Atherosclerotic plaques in the common iliac artery led to a major complication in 1 patient, who later died of hemorrhagic stroke. The other patient developed fatal cardiac tamponade secondary to perforation of the right ventricular wall by a pacemaker catheter.
Although transcatheter aortic valve implantation (TAVI) was first introduced by Cribier and colleagues in 2002, virtually no studies have appeared describing cardiovascular morphologic findings in patients who have had fatal consequences early after the procedure. This report describes necropsy findings in 2 patients who had this procedure several hours or days earlier.
Case Descriptions
Pertinent findings in the 2 patients are listed in Table 1 . Both were 86 years of age, 1 woman and 1 man. Both had evidence of heart failure. Neither had had chest pain. By coronary angiography, both had “luminal irregularities,” but neither had significant narrowings, even though patient 2 had had a stent placed in the right coronary artery 17 years earlier, when 69 years of age. Both patients had decreased renal function: patient 2 had had a unilateral nephrectomy, apparently for cancer, many years earlier. The cardiac index in case 1 was 3.0 L/min/m 2 and in case 2 was 2.4 L/min/m 2 ; the left ventricular ejection fraction in each patient was 40%. A Medtronic CoreValve (Medtronic, Inc., Minneapolis, Minnesota) was used in case 1 and an Edwards SAPIEN valve (Edwards Lifesciences, Irvine, California) in case 2. Before insertion of the bioprostheses, each had balloon aortic valvuloplasty. The bioprostheses reduced the peak systolic transvalvular pressure gradient from 64 to 0 mm Hg in patient 1 and from 65 to 23 mm Hg in case 2, and neither patient developed more than minimal aortic regurgitation after insertion of the bioprosthesis.
| Variable | Patient 1 | Patient 2 |
|---|---|---|
| Age (yrs) | 86 | 86 |
| Gender | Female | Male |
| Heart failure class (0–4+) | 3+ | 1+ |
| Co-morbidities | ||
| Peripheral neuropathy | + | 0 |
| Chronic kidney disease | + | + ∗ |
| Body mass index (kg/m 2 ) | 25.4 | 26.1 |
| LV ejection fraction | 40% | 40% |
| Pressures (mm Hg) | ||
| Left ventricle | 178/21 | 172/20 |
| Aorta | 114/37 | 107/70 |
| LV-aorta peak systolic gradient | 64 | 65 |
| Pulmonary artery wedge mean | 14 | 9 |
| Cardiac index (L/min/m 2 ) | 3.0 | 2.4 |
| Coronary arteries narrowed | 0 | 0 † |
| Aortic valve area (cm 2 ) | 0.62 | 0.77 |
| Aortic valve area index (cm 2 /m 2 ) | 0.38 | 0.50 |
| Type of bioprosthesis used | CoreValve (Medtronic) | SAPIEN (Edwards) |
| Heart weight (g) | 390 | 470 |
| Mitral annular calcium (0–4+) | 2+ | 3+ |
| Aorta calcium (0–4+) | 2+ | 4+ |
| Coronary calcium (0–4+) | 1+ | 3+ |
| Aortic valve calcium (0–4+) | 3+ | 3+ |
| Dilated left ventricle | 0 | 0 |
| Dilated right ventricle | + | + |
| Obliteration of the ostium of the right coronary artery by the native right aortic valve cusp compressed against aorta | + | + |
| Interval TAVI to death | 6 days | 3 hours |
| Cause of death | Stroke | Tamponade |
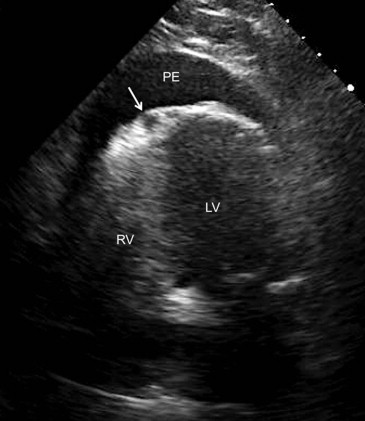
During the procedure, a common iliac artery was transected in patient 1, and as a consequence, this artery was operatively ligated, and a right-to-left femoral-to-femoral artery bypass was performed. Eight transfusions were given, and manual chest compression was applied (for 15 minutes). Although appearing to be recovering from this complication, 7 days post procedure, she suddenly deteriorated mentally: computed tomography disclosed a large hematoma in the left frontal lobe. She died 2 days later. Several hours after completion of the procedure on patient 2, bradycardia suddenly appeared, followed by shock and loss of electrical activity. Echocardiogram ( Figure 1 ) disclosed a huge pericardial effusion and right ventricular diastolic collapse. Resuscitative efforts were unsuccessful. Necropsy disclosed that the pacemaker catheter had extended through the wall of the right ventricle with extensive extravasation of blood into the subpericardial adipose tissue with eventual rupture of the visceral epicardium leading to pericardial tamponade.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


