In this study, we investigated medical history and symptoms before death in all subjects aged 1 to 35 years who died a sudden cardiac death (SCD) from arrhythmogenic right ventricular cardiomyopathy (ARVC) in Denmark in the years 2000 to 2006. All deaths (n = 6,629) in subjects aged 1 to 35 years in Denmark in the period 2000 to 2006 were included. A total of 16 cases of SCD due to ARVC were identified based on histopathologic examination. Information on medical history was retrieved from The National Patient Registry, general practitioners, and hospitals. Symptoms before death were compared with 2 control groups in the same age group and time interval: one consisting of subjects who died in traffic accidents (n = 74) and the other consisting of patients who died a SCD due to coronary artery disease (CAD; n = 34). In the case group, 8 of the 16 patients with ARVC experienced antecedent cardiac symptoms and 7 of them sought medical attention. None were diagnosed with ARVC before death. Only 1 patient in the healthy control group and 31 of the 39 patients with CAD experienced cardiac symptoms before death. A total of 6 patients of the 16 with ARVC died during strenuous physical activity and 4 of the deaths were sports-related SCDs. In conclusion, antecedent cardiac symptoms before SCD in the young were seen in 1/2 of the patients who died because of ARVC, and this is significantly higher than in the healthy control group. When considering the ARVC and CAD groups collectively, antecedent cardiac symptoms are seen in the majority.
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a heritable progressive disease of the myocardium with an estimated prevalence of 1:1,000 to 1:5,000. The disease is known as one of the leading causes of sudden cardiac death (SCD) in the young, accounting for up to 10% to 15% in Europe. Furthermore, in European populations it has been reported to be the cause of death in 22% to 27% of sports-related SCDs. The disease may first be diagnosed postmortem, which leaves little opportunity to study symptoms and number of medical contacts before SCD. Symptoms before SCD have previously been described in young patients with coronary artery disease (CAD). To date, no exact data exist on how many young patients who died a SCD due to ARVC experienced cardiac symptoms before death. We have previously conducted a nationwide study on SCD in patients aged 1 to 35 years in Denmark from 2000 to 2006 in which ARVC was the cause of death in 5% (16 of 314) of all SCDs. In this first nationwide study of SCD in the young due to ARVC, we examined symptoms and medical contacts before death in this cohort and compared them with a control group of patients in the same age group who died a SCD due to CAD and a healthy control group.
Methods
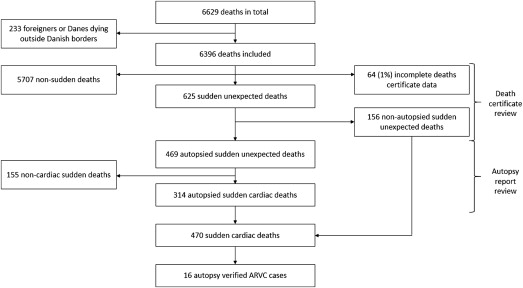
The method by which SCD cases were identified has previously been described in detail. In this study, we included all deaths from 2000 to 2006 (n = 6,629) in subjects aged 1 to 35 years. In total, 470 cases were classified as SCD, of which 314 patients were autopsied ( Figure 1 ). On autopsy and histologic examination, 16 cases were classified as SCD due to ARVC.
In brief, all citizens born or living permanently in Denmark are given a unique National Person Registry Identification number, which is used for all health-care related services. This identification number was used to retrieve information on medical history from the National Patient Registry, the death certificates, and the general practitioners (GPs) of both case and control groups. Since 1978, the National Patient Registry has contained information on all inpatient and outpatient activity at Danish hospitals, emergency rooms, and outpatient clinics, as well as International Classification of Diseases diagnoses for each visit. Furthermore, all citizens have a GP whom they contact when in need of nonemergency medical attention.
The death certificate includes a standardized death scene investigation, supplemented with data from the hospital records, interviews with relatives and witnesses, and an external examination of the body. In Denmark, if external examination does not establish the mode of death, a forensic autopsy is performed. This is performed by a forensic pathologist and is always supervised by another forensic pathologist. The procedure follows a standardized protocol in which all organs are systematically examined. In most cases of SCD in this study (96%), myocardial tissue was sent for histopathologic examination.
GPs and hospitals, in which the patients had been admitted, were contacted by letter. If an answer was not given within 3 weeks, they were contacted by telephone. In the case group, all available medical records from GPs and previous hospital admissions were retrieved independently from the death certificate. All but 2 GPs responded to our contact attempts. All contacted hospitals responded and medical records were available in all but 1 patient.
According to the generally accepted criteria, we defined SCD in the autopsied cases as the sudden, natural, unexpected death of unknown or cardiac causes; in unwitnessed cases, as a person last seen alive and functioning normally <24 hours before being found dead and in witnessed cases, as an acute change in cardiovascular status with the time to death being <1 hour. ARVC was defined according to the guidelines at the time of the study period. Hence, morphometric analysis of the tissue was not performed, and ARVC was defined by the histopathologic finding of moderate- to severe transmural replacement of the right or left ventricular myocardium with fibrofatty tissue with or without chronic inflammatory infiltrate. This assessment was made by the forensic pathologist after evaluation of the histopathologic findings along with the forensic autopsy, a procedure that was supervised by another forensic pathologist. Table 1 lists definitions of clinical terms, according to previous and generally accepted criteria, used in this study. In case of uncertainty regarding the cause of death after review of the autopsy report, the entire case and all its contents was reviewed by and discussed with a forensic pathologist.
| Term | Explanation |
|---|---|
| Sudden unexpected death (SD) | Sudden, unexpected, natural death after review of death certificate |
| Nonautopsied SD | Nonautopsied cases of SD after review of death certificates and medical history |
| Autopsied SCD | SCD concluded after review of autopsy report, consists explained and unexplained SCD |
| Explained SCD | Subgroup of autopsied SCD in which cardiac cause of death is established at autopsy |
| Unexplained SCD | Subgroup of autopsied SCD in which cause of death remains unknown after autopsy |
| Sports-related SCD | Nontraumatic SCD <1 h after moderate- to high-intensity exercise in a competitive athlete |
| Competitive athlete | Participates regularly in physically demanding sports and takes part in competitions |
| Antecedent symptoms | Symptoms in years to days leading up to death |
| Prodromal symptoms | Symptoms in hours to seconds leading up to death |
ARVC case group was compared with a control group of 74 subjects aged 1 to 35 years, who were randomly sampled from a population of 1,497 subjects who died in accidents in the same time period. Furthermore, the ARVC case group was compared with a group of 39 patients who died a SCD due to CAD, in the age group of 1 to 35 years, in the same time period. Information on antecedent cardiac symptoms was available for the entire lifespan of the healthy controls and for 12 months before death for the patients with CAD.
The study was approved by the local ethics committee (KF 01272484), The Danish Data Protection Agency (2005-41-5237), and the Danish National Board of Health (7-505-29-58/1-5).
Results
In the period 2000 through 2006, there were 16 SCDs with autopsy-verified ARVC in Danes aged 1 to 35 years. None of the 16 deaths were diagnosed with ARVC before death. Eight of the 16 patients had symptoms before SCD ( Tables 2 and 3 ), and 7 of these patients had sought medical attention because of these symptoms. The remaining 8 patients had no history of cardiac symptoms. In comparison, 31 of the 39 patients with CAD had experienced cardiac symptoms, 18 of them sought medical attention, and 4 were diagnosed with angina. In the healthy control group, only 1 of the subjects (n = 74) experienced cardiac symptoms before death and had been in contact with the health-care system ( Table 3 ).
| Age | Prodromal Symptoms | Antecedent Symptoms | Medical Evaluation | Diagnosis Given | Electrocardiogram | Echocardiography | Sports-Related SCD |
|---|---|---|---|---|---|---|---|
| 11 | 0 | 0 | 0 | 0 | Right before SCD: AV block | Dilated cavities | 0 |
| 16 | Dyspnea | 0 | 0 | 0 | 0 | 0 | 0 |
| 18 | Unwitnessed death | 0 | 0 | 0 | 0 | 0 | + |
| 18 | 0 | 0 | 0 | 0 | 0 | 0 | + |
| 24 | Unwitnessed death | Tachycardia, syncope | + | 0 | ECG and Holter normal | Normal | 0 |
| 24 | 0 | Fatigue | 0 | 0 | 0 | 0 | 0 |
| 26 | Feeling “unwell” | Angina, palpitations, and fatigue | + | Myocarditis | ST depression in leads V 5 , V 6 , and II, negative T wave in lead III | Discrete LVH and dilated ventricles | + |
| 27 | 0 | Angina, dyspnea | + | Asthma | 0 | 0 | 0 |
| 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 28 | Angina | Dyspnea, syncope, and fatigue | + | Asthma | ECG and Holter normal | 0 | + |
| 29 | Unwitnessed death | Resuscitated SCA, syncope | + | 0 | Sinus rhythm | 0 | 0 |
| 29 | Unwitnessed death | Angina | + | 0 | Negative T waves in leads II, III, aVF, and V 1 –V 6 ( Figure 2 ) | 0 | 0 |
| 30 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 31 | Unwitnessed death | Dyspnea | + | Asthma | 0 | 0 | 0 |
| 34 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 35 | Syncope | 0 | 0 | 0 | 0 | 0 | 0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


