Chapter 25
Myocarditis
2. What is the pathogenesis of myocarditis?
 Phase 1, sometimes called acute viral, occurs after viral entry and proliferation in the myocardium and results in direct tissue injury even before an inflammatory reaction.
Phase 1, sometimes called acute viral, occurs after viral entry and proliferation in the myocardium and results in direct tissue injury even before an inflammatory reaction.
 Phase 2, called subacute immune, is characterized by activation of the innate and acquired immune response. The innate immune response leads to upregulation of a variety of inflammatory mediators like interferons, tumor necrosis factor, and nitric oxide, which ultimately result in an influx of tissue-specific T and B cells (acquired immune response) into the heart. If the inflammatory response persists, a chronic myopathic phase (phase 3) with fibrosis and remodeling with dilation of the ventricles may develop in susceptible individuals.
Phase 2, called subacute immune, is characterized by activation of the innate and acquired immune response. The innate immune response leads to upregulation of a variety of inflammatory mediators like interferons, tumor necrosis factor, and nitric oxide, which ultimately result in an influx of tissue-specific T and B cells (acquired immune response) into the heart. If the inflammatory response persists, a chronic myopathic phase (phase 3) with fibrosis and remodeling with dilation of the ventricles may develop in susceptible individuals.
 In phase 3, immune activation may persist and contribute to progressive cardiomyopathy.
In phase 3, immune activation may persist and contribute to progressive cardiomyopathy.
In any phase, inflammation and fibrosis may lead to ventricular arrhythmias or heart block.
3. What is the clinical presentation of myocarditis?
In contrast to adults with myocarditis, children often have a more fulminant presentation and may require advanced circulatory support for ventricular failure in early stages of their disease. Despite a severe presentation, recovery after a period of hemodynamic support is not uncommon.
4. What is the incidence of myocarditis and who does it affect?
5. What are the causative agents of myocarditis?
Myocarditis can be triggered by many infectious pathogens, including viruses, bacteria, Chlamydia, rickettsia, fungi, and protozoans, as well as systemic toxic and hypersensitivity reactions (Table 25-1).
TABLE 25-1
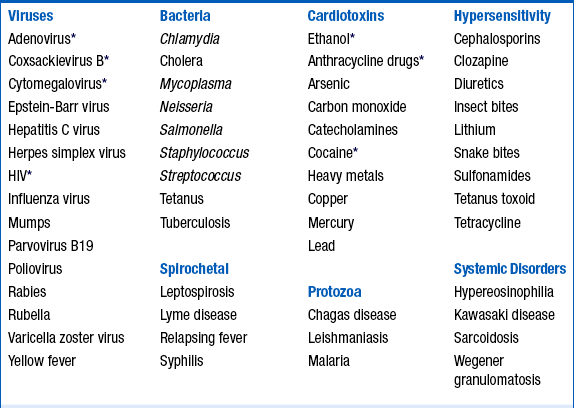
HIV, Human immunodeficiency virus.
∗Frequent cause of myocarditis.
From Elamm C, Fairweather D, Cooper LT: Pathogenesis and diagnosis of myocarditis, Heart 98:835-840, 2012.
Cytomegalovirus (CMV) can cause myocarditis in patients posttransplant and early infection posttransplant correlates with coronary allograft vasculopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






