Coronary artery disease in patients with rheumatologic diseases
Origins
• Atherosclerosis, thrombosis, arteritis, vasospasm
Epidemiology
Systemic lupus erythematosus (SLE)
• The prevalence of ischaemic heart disease (IHD) is 6–10% (true prevalence of subclinical disease not known). Women with SLE are overall 5–6 times more likely to have a myocardial infarction (MI) than non-lupus women of similar age.
Rheumatoid arthritis (RA)
• Incidence 4.8–5.9/1000 person-years. Patients with RA are 2–3 times more likely than matched controls to have a MI, after controlling for traditional risk factors.
• Epicardial disease is more common than microvascular disease.
• Patients with acute coronary syndrome (ACS) have a twofold recurrence rates risk and mortality compared with age- and sex-matched controls.
• Coronary arteritis is uncommon; it affects epicardial and small/medium-sized intramyocardial arteries and usually presents as ACS.
Inflammation and atherogenesis
• There is evidence that inflammation has a fundamental role in the initiation and progression of atherosclerosis.
• Increased risk of IHD cannot be fully explained by traditional atherogenic risk factors (hypertension, hyperlipidaemia, diabetes mellitus, smoking, obesity, sedentary lifestyle).
• Disease or treatment-related risk factors: elevated homocysteine, glucocorticoid use, renal disease (SLE), seropositive disease (RA), and non-steroidal anti-inflammatory drug (NSAID) use (probably by increasing blood pressure).
Differential diagnosis of chest pains
• IHD: maintain lower than normal threshold for investigating and appreciate it as a cause in younger patients
• Primary coronary artery thrombosis (antiphospholipid syndrome)
• Upper gastrointestinal problems associated with NSAID use
• Costochondritis
• Osteoporotic rib/vertebral fracture
• Pleuropericarditis
• Large-vessel vasculitis causing aortic dissection or aneurysm
Management
• Physician awareness and patient education
• Manage traditional risk factors: aggressive blood pressure control, lipid-lowering agents, smoking cessation
• Individualized aerobic exercise programme
• Disease-specific potential risk factors: reduce homocysteine levels (consider folate supplementation), minimize glucocorticoid use, recognize thrombotic potential; consider antiphospholipid antibodies
See Table 13.1.
Table 13.1 Cardiac manifestations of rheumatic diseases
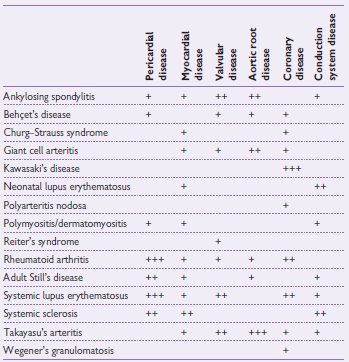
Taken from Manzi S, Kao AH, Wasko MM Oxford Textbook of Rheumatology, Chapter 1.3.4 The cardiovascular system. Oxford: Oxford University Press.
Rheumatoid arthritis
• RA is a multisystem inflammatory autoimmune disease characterized by a symmetrical and progressive deforming, peripheral arthropathy.
• Prevalence 1%; male:female = 1:3, peak onset in the fifth decade.
Clinical features
• Constitutional symptoms such as fever, malaise and fatigue
• Symmetrical polyarthritis with insidious or abrupt onset
• Early morning and rest stiffness
• Subcutaneous nodules
• Pleuritis, interstitial lung disease, intrapulmonary nodules
• Scleritis, episcleritis, dry eyes
Cardiac disease
Coronary artery disease
• See p. 618.
Pericarditis
• 50% of cases have a benign fibrinous pericarditis with effusions seen in 40% of cases on echocardiography
• 1–2% of cases are symptomatic
• Usually independent of disease duration and may precede it
• Cardiac tamponade and constrictive pericarditis are rare
• Responds to treatment with steroids and disease-modifying drugs
Myocardial and endocardial granulomas
• Found in more than 50% of patients with subcutaneous nodules
• Rarely, they compromise cardiac function through mitral valve deformity and regurgitation
• Rarely, they cause conduction problems like first-degree (commonest), left bundle branch, and complete heart blocks
Myocarditis
• 20% of patients with severe disease have a diffuse myocarditis with non-specific inflammatory infiltrates, myocyte necrosis, and fibrosis
• May rarely cause biventricular failure, arrhythmias, and conduction problems
• Ventricular function may also be compromised by secondary amyloidosis
Valvular disease
• Non-specific valvitis producing fibrotic, hyalinized valves with occasional incompetence. The aortic valve is affected more commonly than the mitral valve
Treatment
• Immunosuppressive therapies such as disease-modifying anti-rheumatic drugs (DMARDs) (e.g. methotrexate), Anti-TNF (tumour necrosis factor) therapies and rituximab
• Early intensive treatment (often with combinations of therapies) to tightly control disease activity prevents joint damage and progression to disability
Systemic lupus erythematosus
• Multisystemic autoimmune disease affecting predominately women; female:male = 9:1, peak onset in 20s and 30s,
• Prevalence per 100 000 estimated at 35 in Caucasian and 177 in African-Caribbean individuals in the UK1
• Associated with accelerated atherosclerosis (see p. 212)
• Pulmonary hypertension may occur though more frequent in scleroderma and mixed connective tissue disease (see p. 627)
Pericarditis
• Symptomatic pericarditis occurs in approximately 25% of SLE sufferers at some point in their disease. Autopsy studies show pericardial disease in 61–100%. The pericardial fluid is usually exudative.
• Pericarditis is commonly associated with pleurisy and/or pleural effusion.
• It is frequently associated with active disease in other organs, so full assessment of disease activity is required, including urinalysis, urine protein/creatinine ratio, anti-dsDNA, and complement levels.
• Unusually for SLE, the C-reactive protein (CRP) is usually high, and there may also be a fever.
• Rub is rarely audible; diagnosis is confirmed by electrocardiography (ECG) or ECHO.
• Complications such a pericardial tamponade and constrictive pericarditis are rare, and invasive therapy is not usually required.
• There is usually a prompt response to prednisolone therapy; this may suggest the need for escalation of other disease-modifying therapy.
Myocarditis
• Myocarditis is a vasculopathy rather than true myositis; creatine kinase (CK) is usually normal.
• Diagnosis is usually clinical, based on global ventricular hypokinesis in the context of active disease. Myocardial biopsy, despite the risk of sampling error, remains the gold standard for diagnosis.
• Prevalence by echocardiography is 1–20%.
• Clinically apparent disease usually requires high-dose corticosteroid therapy and escalation of therapy to include other immunosuppressive therapy (such as pulsed cyclophosphamide) in addition to standard heart failure therapy.
Valvular heart disease
• Valve abnormalities are found in 28–74%, most commonly of the mitral valve followed by the aortic valve. Other valves and endocardial surfaces may also be affected. It may cause valve regurgitation; stenosis is rare.
• Libman–Sack’s (verrucous) endocarditis occurs in 4–43% of cases; it is more frequently found in those with antiphospholipid antibodies. Valve leaflet thickening occurs in 19–52% of cases, with associated regurgitation in 73%.
• There is no evidence for the use of immunosuppression or anticoagulation therapy despite the association with complications.
Conduction defects
• Conductions defects can be detected in up to 5% of patients but complete heart block is restricted to case reports.
Antiphospholipid syndrome
• This is an acquired autoimmune thombophilia that causes both arterial and venous thrombosis and pregnancy morbidity.
• Diagnosis requires the detection of anti-cardiolipin, anti-β2-protein antibodies, or lupus anticoagulant, confirmed after 12 weeks to ensure persistence.
• It may be primary or secondary to other connective tissue diseases, particularly SLE.
Valvular disease
• Valve abnormalities are found in 30–32% of cases, particularly those with peripheral arterial thromboses. Vegetations occur in 6–10% and thickening in 10–24%.
• As with SLE, the mitral valve is most frequently affected, followed by the aortic valve. There is no evidence for immunosuppression or anticoagulation.
Thrombotic disease
• Although rare, MI may occur due to primary thrombotic disease despite normal angiography. Pulmonary veno-occlusive disease may cause pulmonary hypertension. A micro-angiopathic cardiomyopathy has also been described.
Neonatal lupus
• Neonatal lupus is associated with the transplacental transmission of anti-Ro antibodies and anti-La antibodies.
• It is not limited to women with lupus, and frequently the mothers have other connective tissue diseases or are asymptomatic.
• The predominant manifestations are photosensitive neonatal lupus rash and congenital heart block, but other organs may be involved.
• With the exception of heart block and myocardial disease, the disease resolves with the clearance of maternal antibodies.
Congenital heart block
• Congenital heart block occurs in approximately 2% of the offspring of anti-Ro antibody-positive mothers, with a recurrence rate in subsequent pregnancies of around 17%.
• There is frequently associated myocardial disease.
• It usually presents between 18 and 30 weeks of gestation.
• Early mortality occurs in approximately 20%.
• Complete heart block is irreversible, 1st- and 2nd-degree heart block may respond to therapy. Betamethasone or dexamethasone should be considered.
• First-degree heart block detected in utero frequently resolves spontaneously. Pre-emptive therapy is not recommended, fluorinated steroids and beta-stimulation may be beneficial in fetuses that are compromised.
Systemic sclerosis
• Systemic sclerosis is characterized by scleroderma proximal to the metacarpal phalangeal joints, Raynaud’s, oesophageal dysmotility, calcinosis, and telangectasia.
• Limited systemic sclerosis: scleroderma is confined to the face and distal limbs in 70% of cases; associated with anti-centromere antibodies. Diffuse systemic sclerosis: patients are more likely to develop lung, cardiac, and renal disease and have a poorer prognosis in 30% of cases. Associated with anti-Scl70 antibodies.
• Following therapeutic advances (particularly for renal hypertensive crisis), cardiac disease and pulmonary hypertension have become more prominent causes of death, with pulmonary hypertension second only to pulmonary fibrosis.
Cardiac disease
• Myocardial fibrosis is found in 50–80% of cases in autopsy studies and in 2/3 of cases using delayed enhanced magnetic resonance imaging (MRI).
• No immunomodulatory therapy has been shown to alter the progression of myocardial fibrosis.
• It is associated with atrial and ventricular arrhythmias, cardiac failure and sudden death.
Pulmonary hypertension and connective tissue diseases
• Pulmonary arterial hypertension is the most frequent cause of death in systemic sclerosis (occurs more frequently in limited systemic sclerosis).
• It also occurs in the other connective tissue diseases, predominantly mixed connective tissue disease and SLE.
• In addition to pulmonary vascular disease, patients are also at risk of pulmonary hypertension secondary to interstitial lung disease or veno-occlusive disease related to the antiphospholipid syndrome.
• Patients at high risk, namely ribonucleoprotein (RNP)-positive mixed connective tissue disease and systemic sclerosis should be screened annually for pulmonary hypertension by echocardiography and lung function testing (including transfer factor).
• Due to the high pregnancy mortality in women with pulmonary hypertension, RNP-positive patients and those with systemic sclerosis should also be screened before conception.
• In contrast to systemic sclerosis, there are some retrospective data to suggest that a proportion of patients with SLE and mixed connective tissue disease may respond to cyclophosphamide therapy. Thus, in addition to the therapies discussed on p. 622, immunosuppressive treatment should be considered in these patients.
Polymyositis and dermatomyositis
• Cardiac disease is the main cause of death in polymyositis (PM) and dermatomyositis (DM) after malignancy and interstitial lung disease. However, it is unclear whether this is due to accelerated atherosclerosis or myocarditis.
• 25% of cases have myocarditis at post-mortem, with microscopic interstitial fibrosis, non-specific inflammatory infiltrates, and necrosis. Ventricular function is usually preserved. However, disease that is severe enough to cause cardiac failure is rare.
• Conducting tissues may be affected, producing non-specific ST- and T-wave changes, atrial arrhythmias, and atrioventricular and bundle branch block. These are more commonly seen in children.
• Clinically apparent pericarditis is rare but is seen in 25% on echocardiography.
• Cor pulmonale may occur secondary to primary lung disease or pulmonary hypertension.
• Overt myocarditis should be treated using steroids and immunosuppressive drugs.
Mixed connective tissue disease
• This group of patients has high-titre anti-RNP antibodies and clinical features of scleroderma, SLE, and inflammatory myositis. As such, they may have the cardiac manifestations of any of these connective tissue diseases. Pericarditis is the commonest cardiac manifestation, found in 10–30% patients. Pulmonary hypertension has a prevalence of approximately 13% and is a major cause of death. Patients should have annual screening for pulmonary hypertension.
Related
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


