Chapter 7
Multiple Orthopaedic Injuries
Written by N. Plani, H. van Aswegen and B.M. Morrow
An increase in death rate due to traumatic injury is projected by the World Health Organisation by 2030, with road traffic accident mortality figures rising from 1.3 million in 2004 to 2.4 million in 2030. Patients who suffer high-energy traumatic injuries frequently have orthopaedic involvement and those who present with extremity fractures may also suffer from abdominal, chest, spinal cord or traumatic brain injuries.
This chapter discusses the following topics related to the management of traumatic orthopaedic injuries:
•The causes and mechanisms of fractures.
•Types of fractures.
•The orthopaedic injuries commonly encountered in the polytrauma patient.
•Classification of fractures.
•The complications associated with fractures.
•The medical and surgical management of a patient who sustained multiple orthopaedic injuries.
•Mechanism of bone healing.
•The physiotherapy aims of management of a patient in the intensive care unit and trauma ward who sustained orthopaedic injuries.
•The contraindications and precautions related to the physiotherapy management of a patient with orthopaedic injuries.
•The physiotherapy interventions for patients who have suffered fractures.
•Adult and paediatric clinical case scenarios.
7.1. Causes and Mechanisms of Injury
7.1.1. Causes of injury in adults
In countries such as South Africa, trauma-related injuries are common occurrences. There are approximately 20 non-fatal incidents that result in disability for each violent fatality (Groenewald et al., 2008; South African Medical Research Council, 2008). Motor cycle, motor vehicle and pedestrian vehicle accidents, as well as assault, are listed as the main causes of injury in adults. Many of these patients are critically injured and require extensive treatment in an intensive care unit (ICU).
The American College of Surgeons’ national trauma data bank indicated that, in 2013, motor vehicle-related injuries accounted for 27% of cases in the data bank, especially in persons aged 19. Across the data bank, the leading two causes of death were fall-related injury followed by motor vehicle-related injury. Case fatality rates were reported to increase with the severity of injury sustained (National Trauma Data Bank Report, 2013). Multiple orthopaedic injuries account for approximately 10% of inpatient rehabilitation admissions in the USA (Uniform Data System for Medical Rehabilitation, 2004; Dubov et al., 2008).
High-energy injuries, such as road traffic accidents or a fall from a height, may result in traumatic brain injury or spinal cord injury together with pelvic, femoral shaft or tibial plateau fractures, as well as hip or knee dislocations in young adults. Elderly patients may sustain pelvic, femur or tibial plateau fractures from low energy injuries, such as a simple fall (Ip, 2008).
7.1.2. Causes of injury in paediatrics
Common sites of injury in children with polytrauma are the head, chest, abdomen, genitourinary and musculoskeletal systems. Mortality in these children is usually associated with traumatic brain, abdominal or chest injuries (Kay and Skaggs, 2006; Abdelgawad and Kanlic, 2011).
The most common orthopaedic injuries in children with polytrauma are open fractures (about 10% of fractures in children with multiple injuries), compartment syndrome, pelvic injuries, multiple bone fracture, fracture-associated vascular injuries and spinal injuries (Abdelgawad and Kanlic, 2011). In the setting of high-energy or multiple traumas, children should always be assumed to have a spinal injury unless proven otherwise (Skaggs and Flynn, 2006). The presence of a pelvic fracture indicates that the child has been exposed to high-energy trauma and careful exclusion of other injuries is essential (Abdelgawad and Kanlic, 2011).
Most fractures are sustained during falls, motor vehicle accidents and other accidental injuries, including crush injuries (Rennie et al., 2007). However, non-accidental injury (NAI) should always be suspected in children presenting with multiple injuries, unless a clear and validated history to the contrary is obtained (Kemp et al., 2008; Abdelgawad and Kanlic, 2011). Warning signs of NAI include humeral fractures in children under three years and femur or tibia and fibula fractures in children less than 18 months of age (Pandya et al., 2009; Abdelgawad and Kanlic, 2011). Other fracture locations with a high specificity for NAI include the ribs, scapula, lateral end of the clavicle and vertebrae. In addition, the presence of fractures in different stages of healing, digital fractures in non-mobile children and bilateral fractures should raise a high index of suspicion for NAI (Jayakumar et al., 2010).
7.1.3. Mechanism of injury in adults
Bone has complex mechanical properties, combining strength, elasticity and adaptability. It has a unique ability to repair itself, but fails when overloaded. The rate at which a bone is loaded, and the orientation of the bone microstructure in relation to the direction of the applied force, influences the amount of load it can withstand. Direct injury to the bone may result in a fracture. With indirect traumatic loading, bone might be subjected to a combination of axial, bending and torsional loads that can lead to fractures (McRae, 2006). Fractures occur when the local stress or strain exceeds the strength of the bone in that area. Fracture patterns will depend on the type and direction of load applied and may be complex. In addition, high loads might cause comminution of the fracture (Hipp and Hayes, 2009).
The mechanical properties of bone slowly degrade with age. There is net bone mass loss and increased brittleness with decreased ability to absorb energy, leading to an increased fracture risk. The most significant change in ageing bone is the ease with which a fracture progresses through the bone (Hipp and Hayes, 2009). Fragility fractures, such as neck of femur fractures, become more common as age progresses. Increasing age has been shown to play a role in the inhibition of fracture healing (Gaston and Simpson, 2007).
7.1.4. Mechanism of injury in paediatrics
There are a number of differences between paediatric and adult bone structure that influence the injuries incurred during trauma. Children have a thicker periosteum, which commonly results in an intact periosteum on one side of the bone following a fracture, making closed reduction easier. The intact periosteum decreases the amount of fracture displacement, even in response to high-energy trauma. However, the limited bulk in children (fat and muscle mass) means that the bone is often more vulnerable to injury, as it is less protected than in adults (Musgrave and Mendelson, 2002). In children, a larger sub-periostial haematoma forms, which, together with the thicker periosteum, enhances the rapid formation of callus and hence bone healing (Gaston and Simpson, 2007).
In flat bones, bone formation occurs by either membranous, appositional bone formation or by endochondral ossification. Endochondral ossification in long bones occurs at the growth plates (physes), which allows longitudinal bone growth until skeletal maturity (about 14 years in girls and 16 years in boys) (Musgrave and Mendelson, 2002). Injury to the growth plates is common in children (about 25% of all paediatric fractures), whereas in adults the ligaments and insertions are the weakest periarticular structures. In children the growth plates are significantly weaker than the ligaments; therefore therapists should be aware that ‘sprains’ in children might be unrecognised fractures (Musgrave and Mendelson, 2002). Physeal injuries in skeletally immature bone may lead to the formation of physeal bridges, a well-recognised complication of physeal fractures (Khoshhal and Kiefer, 2005). Physeal bridge formation leads to growth plate arrest (closure), especially in early adolescence when the physis is at its thickest and the cartilage at its weakest (Khoshhal and Kiefer, 2005). Some physeal bridges resolve spontaneously but others may result in the shortening of the affected limb (leg length discrepancy) if the growth plate closure is complete, or angular limb deformity if the closure is incomplete (Khoshhal and Kiefer, 2005; Abdelgawad and Kanlic, 2011). Some physeal bridges lengthen spontaneously with growth (Khoshhal and Kiefer, 2005). Physeal fractures tend to heal faster than metaphyseal or diaphyseal fractures, so the window for remanipulation of a physeal fracture is short: generally no more than five days after injury (Skaggs and Flynn, 2006).
7.2. Types of Fractures
Table 7.1 outlines the types of fractures commonly seen in patients who have suffered traumatic injury, as well as a description of each fracture type (McRae, 2006; Staheli, 2006; Ratini, 2014).
7.3. Orthopaedic Injuries Commonly Encountered in the Polytrauma Patient
7.3.1. Shoulder girdle
A variety of shoulder injuries can result from high- or low-energy trauma. Table 7.2 provides a summary of the structures of the shoulder girdle that may be injured, the mechanism of injury and associated injuries.
Rotator cuff tears are surgically repaired only after the patient’s life-threatening injuries are stabilised. This might be after discharge from the acute care setting. Rehabilitation protocols for rotator cuff repairs are well described in the literature and the reader is referred to Section 7.12 for further information.
Table 7.1:Description of fracture types.
| Type of fracture | Description |
| Simple transverse | These fractures run at a 90° angle to the long axis of a bone. There is minimal displacement of bony ends at the fracture site and shortening of the bone is not a concern. |
| Simple oblique | These fractures run at an oblique angle (30° or more) along the long bone. |
| Simple spiral | These fractures result from indirect torsional forces to a long bone. The fracture line runs around the bone and displacement is minimal because large areas of bone remain in contact. |
| Greenstick | This is an incomplete fracture of the bone in which the bone is bent. It is a common type of fracture in children. |
| Buckle | The ends of the bones in the fractured site are driven into each other with this type of fracture. It is often called an impacted fracture and is commonly seen in children. |
| Compression (crush) | These occur when cancellous (spongy) bone is compressed beyond its tolerance limit. Crush fractures of the vertebral bodies are associated with spinal flexion injuries. Crush fractures of the ankle are encountered when a person falls from a height. |
| Comminuted | This type of fracture has more than two fragments. Examples of comminuted fractures are: •Spiral wedge fracture caused by torsion forces (Fig. 7.1) •Bending wedge fracture caused by direct or indirect violence After reduction, the main fragments will still have bony contact. Comminuted fractures are rare in children due to higher proportions of cellular and porous bone, which reduce tensile strength and the tendency to propagate. |
| Compound | Compound fractures are fractures with an associated open wound of the skin. They are classified as Grade I, II or III depending on the size of the open wound. Compound fractures are more prone to infection, and open reduction and internal fixation (ORIF) of these fractures may be associated with chronic sepsis. |
| Multifragmentary complex | These types of injuries are caused by significant violence and are difficult to manage. Three types of complex fractures are identified: •Complex spiral fractures (more than two spiral fragments) •Complex segmental fractures (minimum of one separate complete bone segment) (Fig. 7.2) •Complex irregular fractures (the fractured segment is split into many irregular fragments) After reduction there is no contact between the main bone fragments, and delayed union and joint stiffness are common complications. |
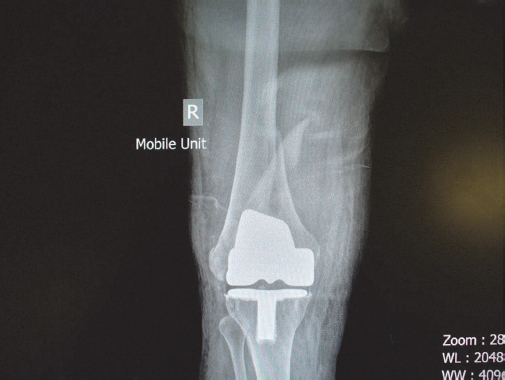
Fig. 7.1:A patient with a comminuted spiral wedge femur fracture and previous total knee replacement.
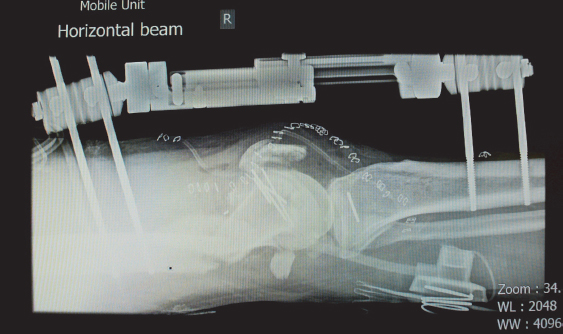
Fig. 7.2:A patient with multifragmentary complex fractures of the distal femur managed with an external fixator.
Table 7.2:Commonly encountered injuries to the shoulder girdle.
| Structure | Mechanism of injury | Associated injuries |
| Clavicle | Injury may result from a fall on the side of the shoulder or from a heavy blow to the front of the shoulder. | •Assessment for acromioclavicular joint involvement is important, especially if the lateral end of the clavicle is fractured (McRae, 2006). •Clavicle fractures may result in injury to the brachial plexus and careful assessment for decreased usage of the affected upper limb is essential for diagnosis (Dandy and Edwards, 2009). |
| Scapula | Injury may result from a direct blow to the scapula. Scapula blade and scapula spine fractures heal quickly without complications. | If the scapula neck is injured, the integrity of the glenohumeral joint should be assessed closely. The glenoid can be fractured from a direct blow on the lateral side of the shoulder (McRae, 2006; Dandy and Edwards, 2009). |
| Rotator cuff tear | May be present in a patient with upper limb trauma (McRae, 2006). | Not applicable. |
| Anterior shoulder dislocation | It is the most common form of shoulder dislocation. It often occurs due to a fall that leads to external rotation and abduction of the shoulder and is also seen with motorcycle accidents. | Axillary nerve palsy may occur with anterior shoulder dislocation (McRae, 2006). |
7.3.2. Humerus
Table 7.3 outlines typical humerus fractures seen in patients who suffered traumatic injury.
Table 7.3:Commonly encountered injuries of the humerus.
| Structure | Mechanism of injury | Associated injuries |
| Fracture of the surgical neck of the humerus or greater tuberosity | A fall onto an outstretched arm. | The axillary nerve and the posterior circumflex artery may be damaged. |
| Fracture of the humerus shaft | Direct or indirect blows to the arm. | Radial nerve palsy is commonly associated with fractures of the middle third of the humerus (McRae, 2006; Dandy and Edwards, 2009; Carroll et al., 2012). |
| Supracondylar fractures (most common humeral fractures seen in children) | Hyperextension of the elbow when a child tries to catch themselves during a fall. | Radial or ulnar nerve injury (15%), vascular compromise (20%) and compartment syndrome (infrequent) are reported as associated injuries (Skaggs and Flynn, 2006). Injury to the median nerve may also occur. |
| Lateral condyle fractures of the distal humerus (second most common humeral fractures in children) | Fall onto an extended elbow leads to the impaction of the head of the radius into the distal humerus. | Fewer complications and less associated soft tissue injury are reported (Skaggs and Flynn, 2006). |
7.3.3. Radius and ulna
Incidents such as a fall or direct blow to the elbow often result in a fracture of the radial head, the radial neck or both. Direct violence to the forearm, such as when warding off a blow during assault, results in shaft fractures of the radius or ulna. Commonly, fracture of one leads to dislocation of the other. A Monteggia fracture is a fracture of the ulna with dislocation of the radial head and is the most common fracture-dislocation injury in the forearm. Conversely, a Galeazzi fracture is a fracture of the radial shaft accompanied by a dislocation of the distal radio-ulna joint (McRae, 2006; Dandy and Edwards, 2009).
7.3.4. Hand and wrist
Hand and wrist injuries are complex due to the number of articular joints, innervation and blood supply. Even minimal injury may lead to large dysfunction. If immobilisation is required, this may severely impact on function and recovery time may be extended (Adams and Hamblen, 2005). Hand and wrist injuries commonly occur in children. Growth plate injuries are commonly seen in hand fractures, but growth problems are rare. The reader should refer to Section 7.12 for more information on various types of hand and wrist injuries.
7.3.5. Pelvis
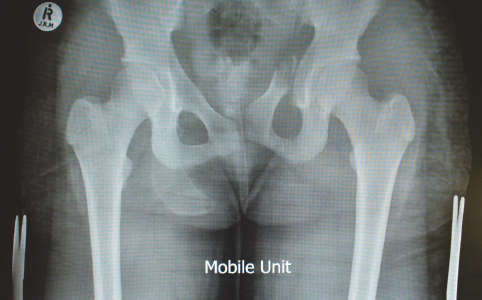
Fractures of the pelvis are often associated with significant haemorrhage due to the rich blood supply to the pelvis. Internal haemorrhage may be severe and pelvic fractures carry a mortality rate of up to 40% if the haemorrhage is not timely managed (Mejaddam and Velmahos, 2012). Unstable pelvic fractures are those in which the pelvic ring is broken at two levels and free to open out (‘open book’). An ‘open book’ pelvic fracture leads to significant blood loss due to damage to vascular structures and is associated with a high mortality rate. Stable pelvic fractures involve isolated injuries to the pelvic ring, e.g. superior or inferior pubic rami fractures, and do not include displacement (McRae, 2006). Figure 7.3 shows an example of a left superior pubic ramus fracture.
In the long term following complex pelvic fractures, patients may experience lingering pain, pelvic instability, leg length discrepancies, nerve and soft tissue damage and difficulty in sitting or, for females, giving birth (Adams and Hamblen, 2005; Hall and Brody, 2005).
Because the pelvis in children is more elastic than adults (requiring higher force to fracture), pelvic fractures in young children are rare (Musgrave and Mendelson, 2002). Most pelvic fractures that do occur in children are stable, with no widening of the symphysis pubis or sacroiliac joints (Abdelgawad and Kanlic, 2011). The vast majority of pelvic fractures in children can be managed without surgical intervention, but associated serious injury may cause significant morbidity and mortality, with the mortality rate for children with closed pelvic fractures being as high as 9% and up to 50% in children with ‘open book’ pelvic fractures (Musgrave and Mendelson, 2002; Skaggs and Flynn, 2006).
7.3.6. Acetabulum
A direct blow to the side of the hip joint or to the front of the knee in a seated position (dashboard injury) may drive the femur head into the pelvis and result in an acetabulum fracture. In the elderly, low-energy injury such as a simple fall may lead to acetabulum fracture due to osteoporotic bone. Table 7.4 lists the most common types of acetabular fractures encountered, as well as associated complications (Kim et al., 2011; Wheeless, 2012; Weatherford, 2014).
Table 7.4:Acetabular fractures and their associated complications.
| Most common types of acetabular fractures | Injuries associated with acetabular fractures | Long-term complications |
| Posterior acetabulum wall fracture | Soft tissue detachment at the time of injury | Avascular necrosis of the femur head |
| Both anterior and posterior column fractures | Gynaecological, urinary or rectal injury | Heterotopic ossification of the acetabulum |
| Transverse acetabulum fracture with posterior wall fracture | Sciatic nerve injury (30% of cases) Vascular injury | Traumatic osteoarthritis of the hip |
| Transverse fracture only | ||
| Transverse fracture with medial acetabular wall fracture (also called T-shaped fracture) |
7.3.7. Hip dislocation
Hip dislocation may result from dashboard injuries during motor vehicle accidents, with energy transmitted up the femoral shaft into the hip joint. It may also occur with falls from a height or assault to the back of someone who is kneeling (McRae, 2006). Posterior dislocation of the hip (adduction and internal rotation abnormality) is most commonly seen with high-energy injury. Central hip dislocation may occur with acetabular fractures (Ip, 2008).
Traumatic hip dislocations are generally uncommon in children and fracture dislocations are seen in adolescents (Staheli, 2006). Hip dislocation in children may be from trivial trauma (in toddlers and young children), or from significant trauma in older children and teenagers. In young children without associated injury, closed reduction is usually performed and avascular necrosis is rare. In older children, however, avascular necrosis is more common and related to the severity of injury. If spontaneous reduction has occurred, the injury may be missed and tissue may be interposed within the joint. Adolescents with hip dislocation may have the additional problem of an unstable femoral epiphysis (Skaggs and Flynn, 2006).
Table 7.5:Femoral injuries and associated complications in adults and children.
| Type of fracture | Complications |
| Femur neck | •Neurovascular injury •Avascular necrosis (a third to half of hip fractures) •Growth disturbance with physeal damage •Coxa vara (not with internal fixation) |
| Femur shaft | •Closed femur fractures are associated with blood loss into the surrounding tissue of up to two litres in adults; greater blood loss is seen with open (compound) femur fractures •Femoral shaft fractures in children seldom lead to levels of blood loss requiring replacement, although signs of shock in children may still indicate occult bleeding |
7.3.8. Femur
Femoral injury is often the result of high-energy activity in younger adults or children (road traffic accidents, falls from a height, crushing injury), or low-energy activity such as a simple fall or trip in the elderly. Table 7.5 summarises the types of fractures and associated complications related to femur fractures (McRae, 2006; Staheli, 2006; Ip, 2008; Dandy and Edwards, 2009).
Always consider the possibility of NAI in a child presenting with a femur fracture if the history is not clear, particularly in non-ambulatory infants. About 70% of paediatric femur fractures are shaft (diaphyseal) fractures (Musgrave and Mendelson, 2002). Femur fractures in children are often not as problematic as their adult counterparts, owing to the thick periosteum and good remodelling potential, which usually leads to good long-term outcomes.
7.3.9. Knee dislocation
Knee (tibio-femoral) dislocation can be classified according to type, e.g. anterior, posterior, medial or lateral, and rotary dislocation, e.g. anteromedial, anterolateral, posteromedial and posterolateral. High-velocity knee dislocations are very likely to involve extensive neurovascular and soft tissue injury. Lower rates of injury and better functional recovery are associated with low-velocity knee dislocations (Henrichs, 2004). Table 7.6 lists the mechanism of injury for each type of knee dislocation (Henrichs, 2004).
Table 7.6:Mechanisms of injury associated with knee dislocation.
| Type of dislocation | Mechanism of injury |
| Anterior | Characterised by forced hyperextension of the knee caused by motor vehicle or pedestrian vehicle accidents, unexpectedly stepping into a hole in the ground or sporting activities such as rugby or football |
| Posterior | Characterised by a direct force applied to the tibia while the knee is in a flexed position, such as when an athlete falls or when the knee strikes the dashboard in a motor vehicle accident |
| Medial or lateral | Characterised by varus or valgus forces applied to the knee |
| Rotary | Characterised by rotary forces applied to the knee |
Anterior knee dislocation commonly occurs and is associated with significant knee ligament damage, vascular injury (especially the popliteal artery), common peroneal nerve palsy, displacement of menisci and fractures of the tibial spine (McRae, 2006; Ip, 2008).
Knee dislocations are rarely seen in children. They usually follow high-energy injuries and are more prevalent in older children and adolescents. There is a high risk of associated neurovascular injury, compartment syndrome and multiple ligamentous injury (Musgrave and Mendelson, 2002).
7.3.10. Patella injury
Any direct blow to the patella may result in joint cartilage damage, with or without fracture or dislocation. In the long term, patients may develop cartilage breakdown. Some may even develop erosion of the joint cartilage, with the associated development of degenerative joint disease.
Patellar sleeve injuries, characterised by avulsion of the patellar ligament from the distal pole of the patella, are unique to children and should be considered in any trauma patient who does not have full active knee extension (assuming the child is generally able to move actively) (Skaggs and Flynn, 2006; Staheli, 2006).
7.3.11. Floating knee injury
Ipsilateral fractures of the femur and tibia (combinations of diaphyseal, metaphyseal and intra-articular fractures) are called floating knee injuries. Floating knee injuries are generally the result of high-energy impact in the polytrauma patient. Concomitant knee ligament injury is often identified (Lundy and Johnson, 2001; Ip, 2008).
7.3.12. Tibial plateau
The tibial plateau is injured with violent blows (inwardly or outwardly) to the lateral side of the knee during weight bearing (also known as axial loading). This type of injury may occur as the result of a pedestrian vehicle or motor vehicle accident or with a fall from a height. Injuries that accompany tibial plateau fractures include meniscus, ligament and patella injuries (Ip, 2008).
7.3.13. Tibia and fibula
Direct trauma to the lateral side of the lower leg can result in fracture of the fibula alone. Dislocation of the fibula head may lead to peroneal nerve injury (Wheeles, 2012). Direct trauma to the lower leg (e.g. fall from a height) may result in a fracture of the tibia alone. Open fractures are common with tibial fractures in which the subcutaneous section of the tibia is injured. The popliteal artery may be damaged with fractures of the upper tibia. Commonly, both the tibia and fibula are fractured with road traffic accidents (McRae, 2006; Dandy and Edwards, 2009).
7.3.14. Foot
Traumatic injury to the foot can be categorised as forefoot, midfoot and calcaneal injury. Metatarsal bone fractures make up 80% of all fractures of the foot and ankle and extensive soft tissue injury is commonly seen (Clements and Schopf, 2013). Fractures to the first metatarsal bone and first metatarso-phalangeal joint are associated with significant functional impairment due to the limitation imposed on the amount of anatomical movement that usually takes place around these structures. Recovery from forefoot trauma can therefore be prolonged (Clements and Schopf, 2013). Calcaneus fractures are caused by high-energy impact injury such as fall from a height or motor vehicle accident. A twisting action often causes a crack in the calcaneus, whereas head-on collision (in the case of a motor vehicle) leads to shattering of the bone. The subtalar joint may be damaged with calcaneus injury and results in balance impairment when a patient walks on an uneven or slanted surface. Short-term outcomes after traumatic foot injury are influenced by the extent of the soft tissue damage, whereas long-term outcomes are affected by the extent of the bone injury (AAOS, 2010; Kinner et al., 2011).
Foot injuries account for up to 6% of all children’s fractures, with about half involving the metatarsal bones. Soft tissue injuries are relatively common, owing to the vulnerability of the paediatric foot (Musgrave and Mendelson, 2002).
7.4. Classification of Fractures
In many hospitals a fracture is described by site of anatomical injury, e.g. undisplaced fractured head of humerus; however, various classification systems for fractures can be used in orthopaedic practice to describe injury severity and the need for surgical intervention. Some of the most commonly used classification systems in clinical practice are discussed in this section.
7.4.1. Long bones
The most commonly used classification system is the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification of fractures of long bones. This complex system describes fractures of the humerus, radius and ulna, femur, tibia and fibula. Fracture types are described as least severe (Type A), intermediate (Type B) or most severe (Type C). This classification is used for each fracture that the patient suffers from. Comminuted fractures are generally described as Type B and complex fractures as Type C (McRae, 2006).
7.4.2. Pelvis
The Tile classification is used for pelvic fractures. Three categories with sub-categories are described (McRae, 2006) (Table 7.7).
7.4.3. Acetabulum
The AO classification system, which incorporates components of the Judet and Letournel classification, is used to determine the severity of acetabulum fractures (Table 7.8).
Table 7.7:Tile classification for pelvic fractures.
| Type A (stable) | Type B (rotationally unstable fractures of the pelvic ring that are vertically stable) | Type C (rotationally and vertically unstable) |
| A1: Pelvic fractures that do not involve the pelvic ring | B1: Open book fractures (antero-posterior compression fractures) | C1: Unilateral fractures |
| A2: Minimally displaced stable fractures of the pelvic ring | B2: Ipsilateral compression fractures | C2: Bilateral fractures |
| B3: Contralateral compression fractures | C3: Associated with acetabular fractures |
Table 7.8:AO classification of acetabulum fractures.
| Type | Description |
| Type A | Partial articular fracture, involving only one of the two columns of the acetabulum A1: Posterior wall fracture A2: Posterior column fracture A3: Anterior wall or column fracture |
| Type B | Partial articular fracture involving a transverse component B1: Pure transverse fracture B2: T-shaped fracture B3: Anterior column and posterior hemi-transverse fractures |
| Type C | Complete articular fractures involving both columns C1: High variety extending to the iliac crest C2: Low variety extending to the anterior border of the ilium C3: Extension into the sacroiliac joint |
7.4.4. Floating knee
The Waddell-Fraser classification system is used to determine the severity of floating knee injuries. Two types of injuries are identified with subcategories (Ip, 2008):
•Type I: extra-articular injury;
•Type IIA: femoral shaft fracture with intra-articular tibial fracture;
•Type IIB: Intra-articular distal femur fracture with tibial shaft fracture; and
•Type IIC: Ipsilateral intra-articular fractures of both the distal femur and tibial plateau.
7.4.5. Tibial plateau
The Schatzker classification is the most popular system used to describe tibial plateau fractures. Types IV–VI are related to high-energy impact injuries (Ip, 2008).
•Type I: lateral tibial plateau fracture without depression.
•Type II: lateral tibial plateau fracture with depression.
•Type III: focal depression of articular surface with no associated split.
•Type IV: medial plateau and tibial spine injury with associated ligament injury.
•Type V: bicondylar fracture with split fractures of both the lateral and medial plateaus.
•Type VI: meta-diaphyseal dissociation with associated proximal tibial shaft fracture.
7.4.6. Physeal fractures in children
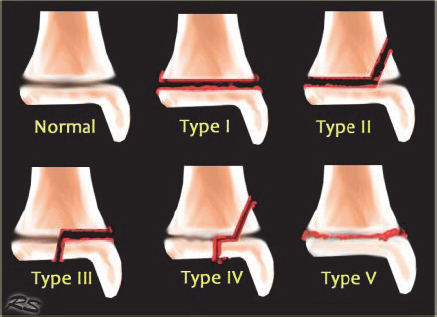
Physeal fractures are commonly classified using the Salter-Harris system (Musgrave and Mendelson, 2002) (Fig. 7.4).
•Type I: complete fracture through the hypertrophic zone of the physis (complete separation of the epiphysis and metaphysis). May be displaced or non-displaced.
Fig. 7.4:Salter-Harris classification of physeal fractures (printed with permission from the Radiological Society of the Netherlands).
•Type II: type I plus a metaphyseal spike attached to the epiphyseal fragment on the compression side of the fracture (Thurston-Holland sign).
•Type III: fracture through the physis that extends through the epiphysis, disrupting the articular surface.
•Type IV: fracture traversing the metaphysis, physis and epiphysis.
•Type V: compression fracture involving the physis (has the highest rate of growth plate disturbance).
The aim is to achieve anatomic reduction of the physis without further injury that could affect growth.
7.4.7. Open fractures
Open fractures are graded according to the Gustilo-Anderson classification system, which takes into account the amount of energy, extent of soft tissue injury and contamination in order to grade fracture severity (Gustilo et al., 1984). This classification system is still widely utilised and is described below.
•Type I: open fracture associated with skin laceration less than 1 cm, minimal periosteal stripping and muscle contamination and a relatively clean wound.
•Type IIIA: open fracture associated with skin laceration greater than 10 cm, with severe soft tissue damage, underlying segmental fracture, or high-energy injury; soft tissue coverage is adequate for delayed primary closure.
•Type IIIB: open fracture associated with skin laceration greater than 10 cm, with extensive soft tissue damage, periosteal stripping and gross contamination. A soft-tissue flap is needed to achieve delayed soft-tissue coverage.
•Type IIIC: open fracture associated with a vascular injury requiring repair.
7.5. Complications Associated with Orthopaedic Injuries
Patients with orthopaedic injuries are at risk of developing various complications associated with soft tissue damage, fractured bones, anaesthesia or prolonged immobility. Table 7.9 lists the complications associated with soft tissue damage and fractured bones (McRae, 2006; Brautigam et al., 2009; Dandy and Edwards, 2009).
Table 7.9:Complications associated with bony fractures and soft tissue injury.
| Fractures | Soft tissue injury |
Malunion, delayed union or non-union Joint stiffness Avascular necrosis Myositis ossificans Osteitis (inflammation of bone) Muscle tendon complications Fat embolism Compartment syndrome Implant complications | Internal or external bleeding Vascular injury and haemarthrosis Neural injury Ligamentous injury Muscle and skin injury Infection Metabolic responses to trauma such as electrolyte shifts and protein breakdown |
7.5.1. Avascular necrosis
Avascular necrosis refers to the death of bone cells due to a lack of blood supply. This complication occurs more frequently in younger adults (aged 45 or less) and typically affects the femoral head, knee, talus, humeral head and scaphoid (Gao et al., 2013). Avascular necrosis results mostly from glucocorticoid therapy, alcohol abuse, long smoking history and blood clotting disorders.
7.5.2. Myositis ossificans
Bone formation in the surrounding tissue outside the bony skeleton is referred to as myositis ossificans or heterotopic ossification. It is occasionally seen in patients with long bone fractures and causes severe pain and limited joint range of motion (ROM). Factors that predispose a patient to the development of myositis ossificans are still unclear. Precautions for the physiotherapy management of patients with this complication are discussed in Section 7.9.
7.5.3. Fat embolism
Fat embolism syndrome develops when fat molecules accumulate in the lung parenchyma and peripheral circulation. The syndrome develops within 72 hours of fractures of the long bones and pelvis or major trauma. It is more frequent in closed than open fractures (Gupta and Reilly, 2007). Patients with fat embolism syndrome develop distinct changes related to the respiratory system, neurological changes and petechial skin rash. Respiratory system changes include dyspnoea, tachypnoea and hypoxaemia, and some patients may require mechanical ventilation (MV) (Gupta and Reilly, 2007). Neurological changes develop after the onset of respiratory distress and may range from mild confusion to severe seizures (Gupta and Reilly, 2007). Petechial rash typically develops in the conjunctiva, oral mucus membranes, neck, axilla and skin folds of the upper body (Gupta and Reilly, 2007).
Key Message
A patient with bilateral closed femur fractures and no chest-related trauma that suddenly develops breathlessness may have a pulmonary embolism. The physiotherapist should immediately inform the orthopaedic or critical care team of the change in symptoms so that a ventilation-perfusion scan of the lungs can be performed to confirm or refute the presence of an embolism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree