A parachute abnormality of the mitral valve is an extremely rare finding in adults. It is usually seen as part of Shone’s complex. The authors present multimodality imaging from a case of adult parachute abnormality of the mitral valve to illustrate and explain features such as the characteristic “pear” shape of the valve and “doming” of the subvalvular apparatus. The solitary papillary muscle that defines the condition may be difficult to identify on transthoracic echocardiography, but redundancy of the chordae is a key echocardiographic feature in the adult form of the condition.
A parachute abnormality of the mitral valve (PMV) occurs when all the chordae tendineae are inserted into a solitary papillary muscle or muscle group. It is usually seen as part of Shone’s complex. Childhood PMV is often severe, with marked thickening and shortening of the chordae, causing a crude funnel-shaped stenosis of the mitral valve. The severity of this dictates prognosis.
In contrast, adult PMV is extremely rare and is generally mild in terms of mitral stenosis. A small number of case reports have followed the initial adult publication in 2001. Several cases have emphasized chordal shortening and thickening, although the pathognomonic features such as “pear” shape and “doming” relate to chordal redundancy instead. Often, only one imaging modality is used to demonstrate the case.
We present multimodality imaging from a case that illustrates and explains the characteristic features of adult PMV.
Case Presentation
A 28-year-old man with known bicuspid aortic valve attended for routine transthoracic echocardiography (TTE). Following our experience with a previous case, features of his mitral valve previously labeled “redundant” or “unusual” were positively identified as PMV. Mitral valve area was calculated at 1.8 cm 2 using the pressure half-time method. Subaortic obstruction and left atrial membrane were not present. Three-dimensional echocardiography, transesophageal echocardiography, and multidetector cardiac computed tomography (MDCT) confirmed PMV, with a nonsignificant aortic coarctation discovered on MDCT.
In contrast to rheumatic stenosis, adult PMV is unlikely to increase in severity over time, but the patient still has flow restriction and embolic risk. Surgical revision of PMV is likely when he undergoes surgery for his bicuspid aortic valve.
Characteristic Imaging Features
Parasternal Short-Axis View
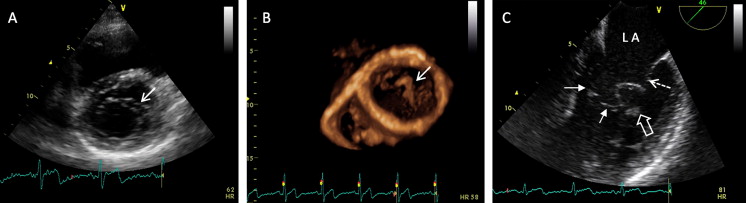
Although the defining feature of a PMV is a single papillary muscle, it may be difficult to positively identify on TTE. Careful examination of the parasternal short-axis view is required to confirm two papillary muscles in any patient with coarctation or bicuspid aortic valve. Apical two-chamber and three-chamber views are also helpful for locating papillary muscles. Redundant chordae may be seen anterior to the anterior mitral valve leaflet in the parasternal short-axis view, giving an appearance similar to a double-orifice mitral valve ( Figure 1 A). This case showed very marked anterior chordal redundancy, with the chords almost folding up double ( Figures 1 , B and 1 C, Video 1 ). Occasionally, the anterior chordal redundancy may produce left ventricular outflow tract obstruction.
“Pear-Shaped” Appearance of PMV
PMV is said to have a characteristic “pear” shape in the four-chamber view. This is illustrated in Figure 2 A. The left atrium usually forms the larger base of the pear, the mitral leaflets are the converging sides, and the redundant anterior chordae form the apex of the pear. In this case, the chordal redundancy is so marked that a “reverse pear” is seen, with the larger base of the pear formed by the chords. Later in diastole, the chordae fold up on themselves, giving rise to whorled patterns ( Figure 2 B). In cases in which visualization of the papillary muscle is difficult, MDCT ( Figure 2 C) or cardiac magnetic resonance imaging may be helpful.





