Bicuspid aortic valve (BAV) is a common congenital malformation with the known sequela of ascending aortic dilation. The morphology of the BAV and the elasticity of the adjacent ascending aorta appear to influence the outcome. We prospectively examined 48 pediatric patients with an isolated, native BAV for the morphology and size of the aortic valve, aortic root, sinotubular junction, and ascending aorta and their elasticity indexes. A cohort of 48 matching subjects with tricuspid aortic valves was investigated as controls. A comparison of the aortic valve subtypes showed normal-size aortic dimensions in the tricuspid aortic valves. In contrast, in the BAVs, the ascending aorta and aortic valve itself tended to dilate with age and aortic elasticity deteriorated. In the BAVs, the stiffness was significantly greater (4.43 ± 1.82 vs 3.43 ± 0.81 in the tricuspid aortic valves; p = 0.001). The distensibility indexes decreased inversely in the BAVs (6.57 ± 2.83 vs 7.84 ± 2.04 cm 2 × dynes −1 × 10 −6 , p = 0.013; and 53.5 ± 26.0 versus 64.3 ± 17.9 kPa −1 × 10 −3 , p = 0.020). The anteroposterior-oriented phenotype of BAVs showed significantly stiffer and less distensible elasticity even after correction for congenital valve dysfunction, which was more frequent in the left–right-oriented phenotype. In conclusion, the morphology of the BAV seems to play a major role in the outcome of BAV disease, although the left–right phenotype is more prone to congenital valve dysfunction, the anteroposterior phenotype showed worse elasticity quality.
In the past, many publications focused on the morphology and elasticity indexes of bicuspid aortic valves (BAVs) and their adjacent aortic tissue in adulthood to determine risk stratifications. However, the combined data for the population of infants, children, and adolescents are lacking. The present study sought to give data about the morphology and elasticity indexes of native, isolated BAVs in children and adolescents and their correlation to valve function and aortic dilation.
Methods
The patients were selected through a review of the institutional pediatric cardiology and echocardiography database of the Pediatric Heart Center (Vienna, Austria). The inclusion criteria were age <20 years and isolated BAV without coarctation of the aorta. The exclusion criteria were earlier valvular operations or balloon valvuloplasty and Marfan or Turner syndrome. Of the 51 children and adolescents fulfilling these criteria, 48 patients were eligible for the present prospective echocardiographic investigation of the morphology, function, and elasticity of their aortic valves from February 2010 to September 2011.
A cohort of 48 matching healthy patients with tricuspid aortic valves (TAVs) in the same age range as our study group that had been referred to our institution for routine checkups, mostly because of an innocent heart murmur, were prospectively recruited as the control group. All subjects included in both groups were in sinus rhythm and had a normal left ventricular ejection fraction of ≥60%. The institutional review board of the Vienna University Hospital committee on human research approved the study protocol. All patients or their relatives provided written informed consent, which was mandatory.
Echocardiographic evaluation—performed using a Vivid E9 GE Medical (Horton, Norway) echocardiographic machine with transducers ranging from 1.5 to 12 MHz—confirmed the diagnosis of BAVs and gave the exact morphology of the valve in a parasternal short-axis view. The diameters of the aortic valve (AV), aortic root (AoR), sinotubular junction, and ascending aorta (AA) were measured perpendicular to the aortic flow in the parasternal long axis using the inner edge to inner edge method. Valvular function was classified as normal, stenotic, regurgitant, or combined by color and continuous wave-Doppler measurements. Aortic stenosis was determined by the maximum instantaneous Doppler gradient, and for the aortic regurgitation classification, a composite evaluation of the proximal jet width, left ventricular end-diastolic dimension, and retrograde descending and abdominal aortic Doppler flow was used. The patients were judged as having none, trivial, mild, moderate, or severe aortic stenosis, and, for regurgitation, we referred to the criteria set by the American Society of Echocardiography.
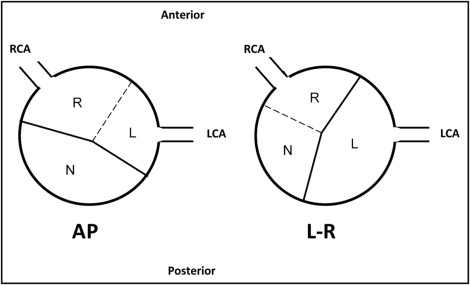
BAV was defined as partial or complete fusion of 2 of the aortic valve leaflets, fusion of right coronary and noncoronary cusps formed the left–right (L–R) phenotype of the valve and fusion of the right and left coronary cusps anteroposterior (AP) phenotype ( Figure 1 ). No left coronary and noncoronary cusp fusion was present in our patient cohort.
The z scores for the inner edge to inner edge values were used to judge the degree of dilation of the aortic dimensions, corresponding to the body surface area. Compared to the normal values, z scores of ≥3 were considered as significant dilation.
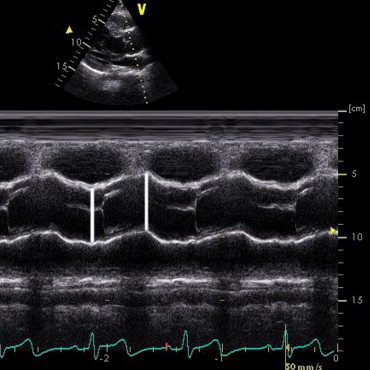
The elastic properties of the aortic root were gained using M-mode imaging in the parasternal long-axis view to measure off-line ≥5 to ≤15 systolic and diastolic diameters to calculate a mean value of the systolic and diastolic diameters ( Figure 2 ). The blood pressure was measured simultaneously during an echocardiographic investigation using a Philips SureSigns VS2 machine (Andover, Massachusetts). The stiffness index was calculated using the formula: aortic stiffness index = ln (SBP − DBP)/[(AoDS − AoDD)/AoDD)], where ln is the natural logarithm, SBP, the systolic blood pressure (mm Hg), DBP, the diastolic blood pressure (mm Hg), AoDS, the aortic diameter in systole, and AoDD the aortic diameter in diastole (mm).
For the distensibility calculations, 2 formulas were used: first using the diameter and second the area of the aortic dimensions: (1) aortic distensibility = 2(AoDS − AoDD)/[AoDD(SBP − DBP)] × 10 −3 [cm 2 dynes −1 × 10 −6 ]; (2) aortic distensibility = (AoAS − AoAD)/[AoAD(SBP − DBP) × 1333] × 10 −7 [kPa −1 × 10 −3 ], where AoAS and AoAD are the aortic areas in systole and diastole calculated by the formula: AoAS = π x (AoDS/2) and AoAD = π x (AoDD/2) , respectively.
Data analysis was performed with PASW Statistics, version 18.0 (SPSS, Chicago, Illinois). For continuous variables, Student’s t test and for nonparametric 2-way testing, the Mann–Whitney U test was used. Analysis of variance was used to test the univariate regression correlations. Unless noted otherwise, values are presented as the mean ± SD; p <0.05 was considered statistically significant. The reliability of the elasticity indexes was calculated as the positive difference between the measurements divided by the mean of these measurements, with values given as the mean percentage of error.
Results
The baseline characteristics are listed in Table 1 . The patients were matched by age subgroup and gender. No differences were found in the systolic or diastolic blood pressure between the male and female patients in the 2 aortic valve groups. Only minor gender differences in AV and STJ z scores in the control subjects and AV and AoR diameter in the BAV subgroup were found, and most were all due to the notably smaller female subgroups. The elastic properties showed no gender differences at all. The comparison of patients with BAVs and TAVs demonstrated that the BAV population had significantly larger dimensions in all 4 aortic sections compared to the TAV population. Likewise, the elastic properties were significantly worse in the patients with BAVs ( Table 2 ).
| Variable | BAV (n = 48) | TAV (n = 48) | p Value |
|---|---|---|---|
| Male children (%) | 39 (81) | 32 (67) | NS |
| Weight (kg) | 50 ± 23 | 44 ± 23 | NS |
| Height (cm) | 150 ± 32 | 143 ± 34 | NS |
| Body surface area (m 2 ) | 1.4 ± 0.5 | 1.3 ± 0.5 | NS |
| Age overall (years) | NS | ||
| Mean ± SD | 11.9 ± 4.8 | 11.1 ± 4.8 | |
| Range | 0.1–19.7 | 0.0–17.7 | |
| Age of male children | NS | ||
| Mean ± SD | 12.8 ± 4.7 | 10.6 ± 4.8 | |
| Range | 0.1–19.7 | 0.3–17.7 | |
| Age of female children | 0.05 | ||
| Mean ± SD | 8.4 ± 3.7 | 12.2 ± 4.6 | |
| Range | 0.1–12.8 | 0.0–16.9 | |
| Age group (n) | |||
| <5 years | 5 | 5 | |
| ≥5–10 years | 10 | 13 | |
| ≥10–15 years | 18 | 17 | |
| ≥15 years | 15 | 13 | |
| Systolic blood pressure (mm Hg) | 106 ± 15 | 105 ± 12 | NS |
| Diastolic blood pressure (mm Hg) | 59 ± 8 | 59 ± 7 | NS |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


