Ventricular tachycardia is often a recurrent problem and may lead to sudden death. An implantable defibrillator may be indicated, particularly in patients with poor ventricular function.
Right ventricular outflow tract and fascicular tachycardias arise in structurally normal hearts, have a good prognosis and are ideally amenable to radiofrequency ablation. Accelerated idioventricular rhythm is ventricular tachycardia at a rate less than 120 beats/min: treatment is not required.
Wherever possible, obtain and save a 12-lead ECG during tachycardia for diagnostic purposes.
ECG characteristics
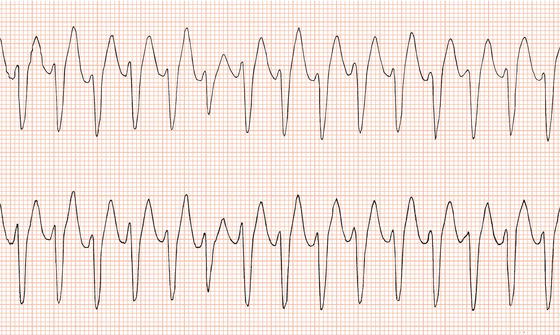
The arrhythmia consists of a rapid succession of ventricular ectopic beats each with the same configuration, hence the term monomorphic (Figure 12.1). As with single ventricular ectopic beats, the complexes will be abnormal in shape, and the duration of each complex will be more than 0.12 s and usually greater than 0.14 s. The rhythm is regular unless there are capture beats (see below) which cause minor irregularities in the rhythm. The rate ranges from 120 to 250 beats/min.
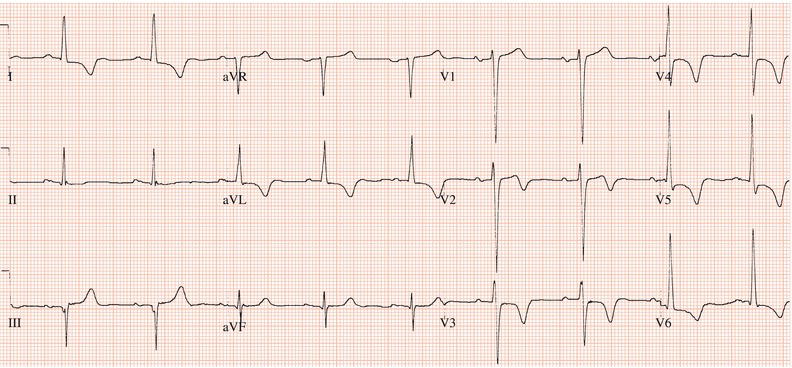
Atrial activity during ventricular tachycardia
With many ventricular tachycardias, the sinus node continues to initiate atrial activity, which is therefore independent of, and slower than, ventricular activity (Figure 12.2). In others, the AV node conducts each ventricular impulse to the atria so a P wave follows the ventricular complex. The P wave is often concealed by the superimposed terminal portion of the ventricular complex (Figure 12.3). Rarely, second-degree block may occur at the AV junction so only some ventricular impulses are conducted to the atria (Figure 12.15b).
Identification of independent atrial activity during tachycardia excludes an origin at AV node level or above and will thus distinguish ventricular tachycardia from supraventricular tachycardia with broad ventricular complexes. There may be direct or indirect evidence of independent atrial activity.
Direct evidence of independent atrial activity
P waves at a slower rate than and dissociated from ventricular activity are direct evidence of independent atrial activity (Figure 12.2). Inevitably, some P waves will be concealed by superimposed ventricular complexes. Furthermore, not all leads will clearly show atrial activity. A rhythm strip is often inadequate, and scrutiny of a simultaneous recording of several different leads may be necessary. Sometimes there will be doubt whether small waves on the ECG during tachycardia are caused by atrial activity. If they are, they will be separated by similar intervals, or multiples of that interval.
Figure 12.1 Monomorphic ventricular tachycardia. There is a rapid, regular succession of broad complexes after four sinus beats (lead III suggests inferior myocardial infarction).
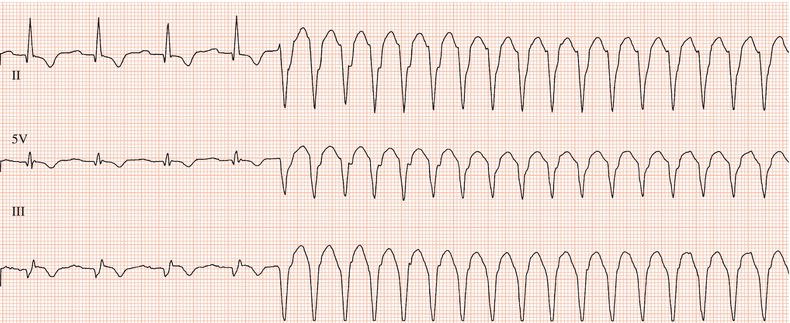
Figure 12.2 Ventricular tachycardia with direct evidence of independent atrial activity. P waves are separated by intervals of 0.75 s, and can clearly be seen after the first, third, sixth, eighth, tenth, thirteenth, fifteenth and seventeenth ventricular complexes.
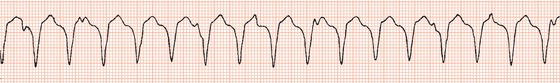
Figure 12.3 Ventricular tachycardia (lead aVF) with retrograde atrial activation. In this case, a P wave can be clearly seen to be superimposed on the T wave of each ventricular complex.

Indirect evidence of independent atrial activity
Capture or fusion beats are indirect evidence of atrial activity. Just one is sufficient to confirm ventricular tachycardia.
Capture beats occur when the timing of an atrial impulse generated by the sinus node during ventricular tachycardia is such that it can be transmitted via the AV junction and activate the ventricles before the next discharge from the ventricular focus. The resultant ventricular complex will be normal in shape and duration and will occur slightly earlier than the next ventricular ectopic beat would have been expected (Figure 12.15a). Fusion beats are caused by a similar process. However, the atrial impulse activates the ventricles slightly later in the cardiac cycle leading to simultaneous activation of the ventricles by the transmitted atrial impulse and the ventricular focus. The result is a ventricular complex with an appearance intermediate between a normal QRS complex and a ventricular ectopic beat (Figure 12.4).
Broad complexes (≥ 0.12 s and usually > 0.14 s)
Ventricular complexes of uniform appearance
Independent P waves may be present
Capture or fusion beats may be present
Causes
Ventricular tachycardia is most often the result of myocardial infarction or of heart muscle disorders.
Past myocardial infarction
Dilated cardiomyopathy
Hypertrophic cardiomyopathy
Arrhythmogenic right ventricular cardiomyopathy
Myocarditis
Mitral valve prolapsed
Valvular heart disease
Repair of tetralogy of Fallot
Sarcoidosis
Chagas’ disease
Digoxin toxicity
Idiopathic
Mechanisms of ventricular tachycardias
Two main mechanisms cause tachycardias: re-entry, which is the commonest mechanism for ventricular tachycardia, and enhanced automaticity, which may be spontaneous or triggered.
Re-entry
Two conditions are necessary for a re-entrant tachycardia to occur. The first is the presence of a potential circuit composed of two pathways of tissue with differing electrical characteristics. The second condition is transient or permanent block in one direction in one of the pathways so an impulse arriving at the circuit can be conducted along one pathway and return via the other pathway, thereby re-entering the circuit. The activating impulse is repeatedly conducted around the circuit, exciting the surrounding myocardium at a rapid rate.
Re-entrant ventricular tachycardia
Re-entrant ventricular tachycardia can result from fibrosis or ischaemia that causes delay in activation and hence recovery of an area of myocardium, i.e. one component of the re-entrant circuit. Tachycardia is initiated by a premature beat arriving at the abnormal area to find it is refractory to excitation following the last heartbeat. The impulse is conducted around the damaged area by the adjacent, normally responsive myocardium. By the time the impulse has circumvented the damaged area, the abnormal myocardium has become excitable again and conducts the impulse in the opposite direction, giving rise to a re-entrant circuit. Perpetuation of this process results in ventricular tachycardia.
Ventricular re-entrant tachycardias can be initiated and terminated by precisely timed premature ventricular pacing stimuli.
Enhanced automaticity
Damage or disease can result in a group of myocardial cells acquiring enhanced automaticity, i.e. the cells discharge at a higher rate than the sinus node, taking over control of the heart rhythm. Enhanced automaticity can either be spontaneous or be triggered by after-depolarisations that lead to early reactivation of the myocardium: ‘early after-depolarisations’ occur at the end of the action potential (phase 3) and ‘late after-depolarisations’ occur during electrical recovery of myocardial cells (phase 4).
Initiation of tachycardia
A re-entrant circuit or focus of enhanced automaticity provides the substrate for ventricular tachycardia. Initiation of the arrhythmia is usually triggered by an ectopic beat. Ischaemia, increased sympathetic nervous system activity or electrolyte imbalance may influence the arrhythmia substrate and may account for a tachycardia occurring at a particular time.
Investigations
The nature and extent of investigations have to be tailored to the individual clinical situation. The aims should be to identify the cause, which may well be of therapeutic and/or prognostic importance, and to assess the role and efficacy of any therapy that may be required.
Twelve-lead ECG
An ECG during sinus rhythm may reveal the cause of tachycardia, e.g. myocardial infarction, or marked left ventricular hypertrophy which in the absence of severe valve disease or hypertension points strongly to hypertrophic cardiomyopathy (Figure 12.5).
Whenever possible, a 12-lead ECG during tachycardia should be recorded. The configuration of the ventricular complexes during tachycardia may indicate its site of origin. A tachycardia with left bundle branch block morphology, i.e. a complex which is positive in V5 and V6 and which is akin to left bundle branch block in its appearance, will usually have a right ventricular origin. A positive complex in lead V1, i.e. with right bundle branch block morphology, points to a left ventricular free wall or septal source. If complexes are negative in V4–V6, a left ventricular apical origin is likely, while Q waves in the inferior leads suggest that the tachycardia is arising from the base of the left ventricle. The ECG appearances of right ventricular outflow tract tachycardia and fascicular tachycardia are diagnostic for those arrhythmias (see below).
Imaging
Echocardiography may help establish the cause of the arrhythmia: for example, by demonstrating dilated or hypertrophic cardiomyopathy, or arrhythmogenic right ventricular cardiomyopathy (ARVC). Magnetic resonance imaging is becoming used more widely. Some regard it as the ‘gold standard’ for the diagnosis of ARVC. Coronary angiography may be indicated, particularly if myocardial ischaemia might be the cause of the arrhythmia or if surgery is contemplated.
Ambulatory electrocardiography
Ambulatory electrocardiography may be required to assess the frequency and duration of episodes of ventricular tachycardia and the effect of therapy in those patients who have had frequent episodes.
Occasionally, ventricular tachycardia is triggered by bradycardia. This may be revealed if the onset of the arrhythmia is recorded. Prevention of bradycardia in this situation will often prevent ventricular tachycardia.
Exercise testing
Exercise-induced tachycardia is not uncommon. An exercise test can be useful both in its diagnosis and in assessment of response to therapy.
Ventricular stimulation study
Stimulation of the ventricles with up to three precisely timed premature stimuli delivered by a temporary pacing lead introduced via the femoral vein will usually initiate ventricular tachycardia in patients who are prone to this arrhythmia (see Figure 13.15). Stimulation protocols involve progressively aggressive attempts to initiate ventricular tachycardia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree