
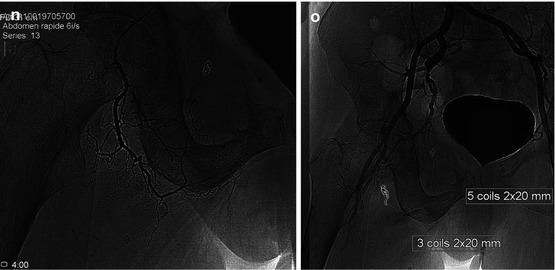
Fig. 24.1
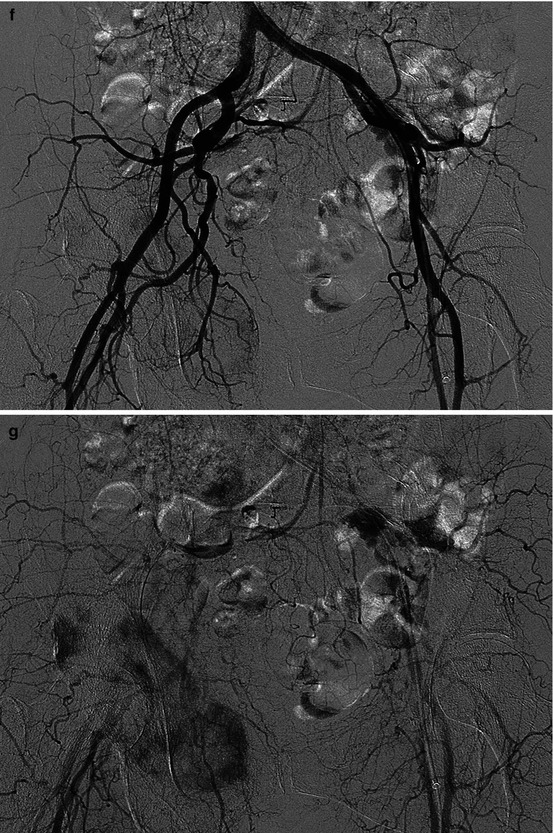
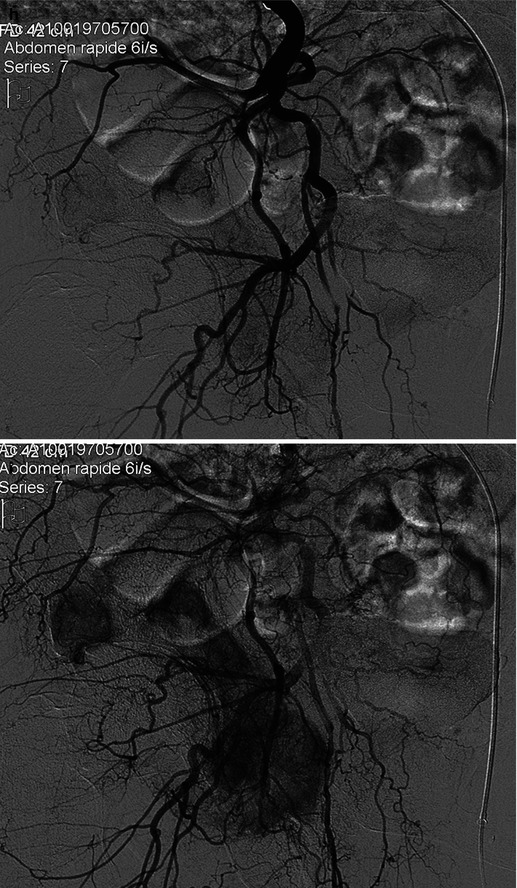
A 63-year-old, osteolytic metastases of the right ischiopubic branch and the right acetabular roof, complicating a thyroid cancer. A total hip replacement was planned, after a preoperative embolization to reduce the risk of bleeding complication. (a: standard view) and (b–e: CT) Large lytic metastasis, partially necrotic but hypervascular. (f, g) Aortoiliac bifurcation injection, to identify the iliofemoral arterial network; late phase: heterogeneous enhancement of metastatic areas. (h, i) Selective catheterization of the right hypogastric artery from a left femoral puncture (early phase, late phase). (j–l) Hyperselective catheterization of the obturator artery. (m) Exclusion by microparticles and then coils. (n) Selective catheterization of an enlarged branch of the common femoral artery involved in tumor vascularization: this artery was excluded by coils + particles. (o) Ultimate control after devascularization by particles + coils of collateral branches involved in tumor vascularization

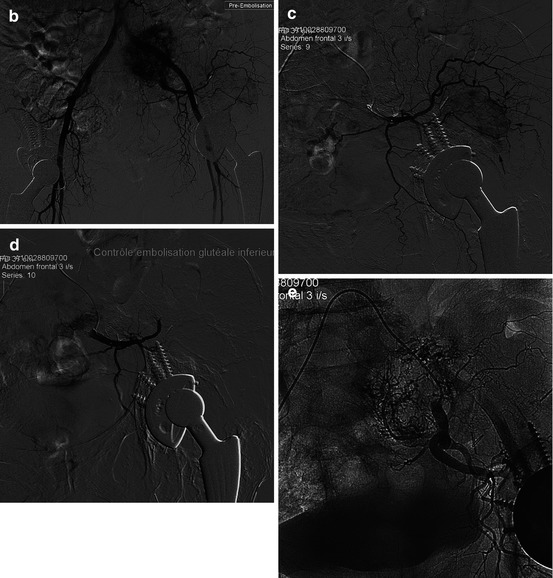
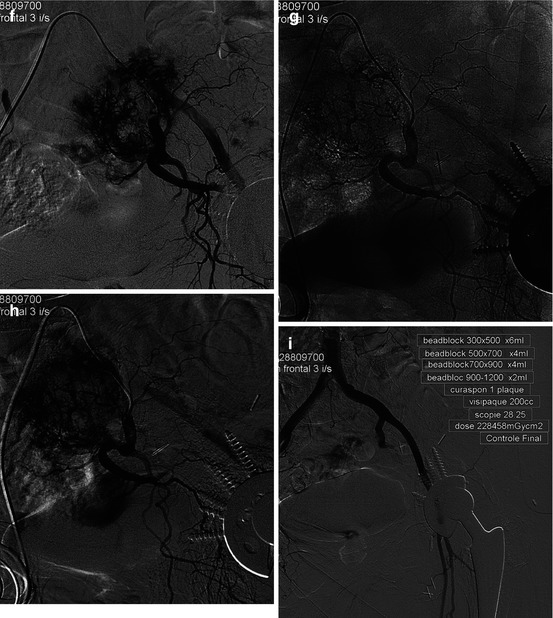
Fig. 24.2
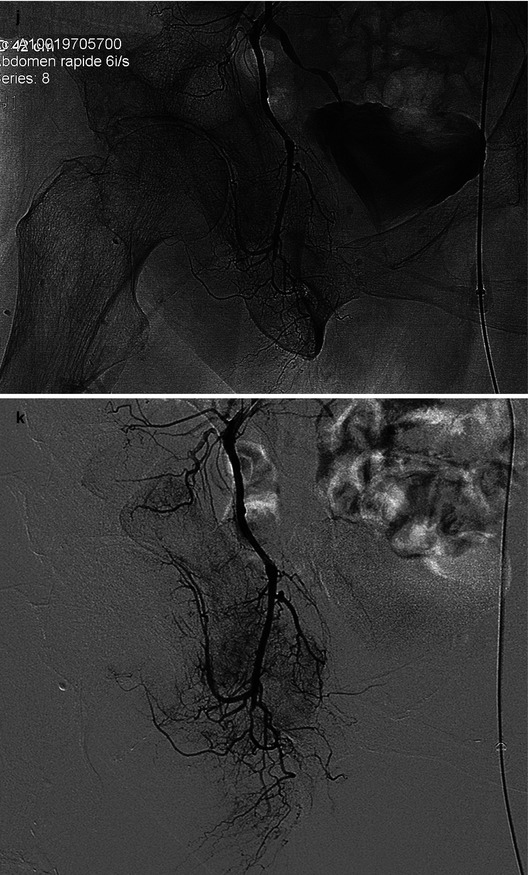
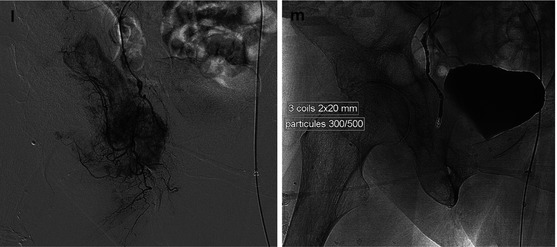
A 74-year-old, pelvic lytic bony metastases of a renal tumor, complicated by the dislocation of a total left hip replacement with fracture of the roof of the acetabulum: a preoperative embolization was requested before osteosynthesis. (a) Standard pelvic view: lytic lesions of the iliac wing, left acetabular roof, and left sacral ala. (b) Opacification of the aortoiliac bifurcation (right femoral access). Late phase: moderate hypervascularization of the acetabular roof; intense enhancement of a bifocal tumoral hypervascularization, fed by the lateral sacral artery for the larger lesion, and by the gluteal artery for the other. (c) Hyperselective catheterization of the inferior gluteal artery (Blush: arrows). (d) Selective control after exclusion with particles of the territory of the gluteal artery (frontal view). (e–h) Frontal and RAO views: identification of the left hypogastric artery, followed by selective catheterization and embolization by particles of the lateral sacral artery, which abundantly vascularize the metastatic lesion. (i) Aortoiliac control opacification at the end of the procedure showing the arterial exclusion of the two metastases, allowing reconstructive surgery with less bleeding
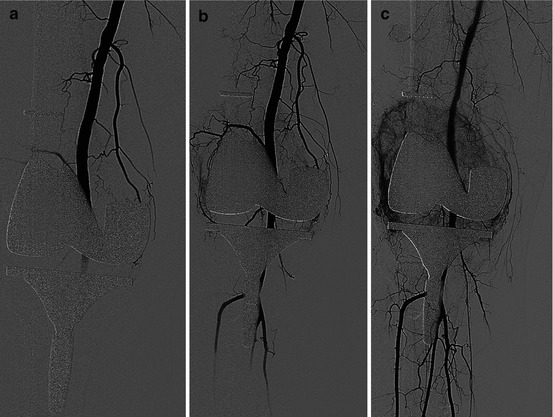
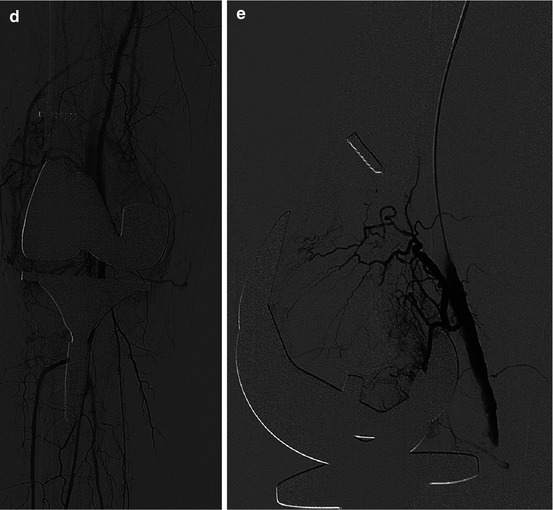
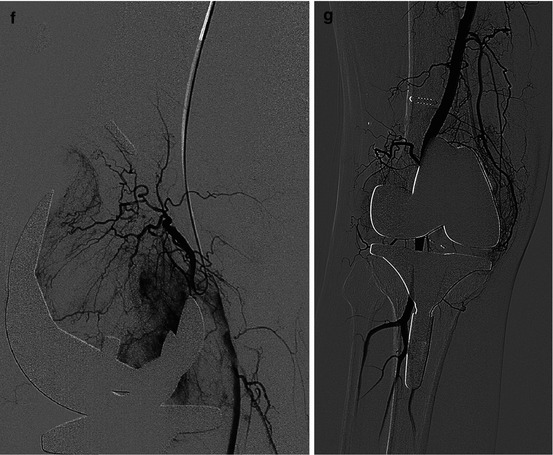
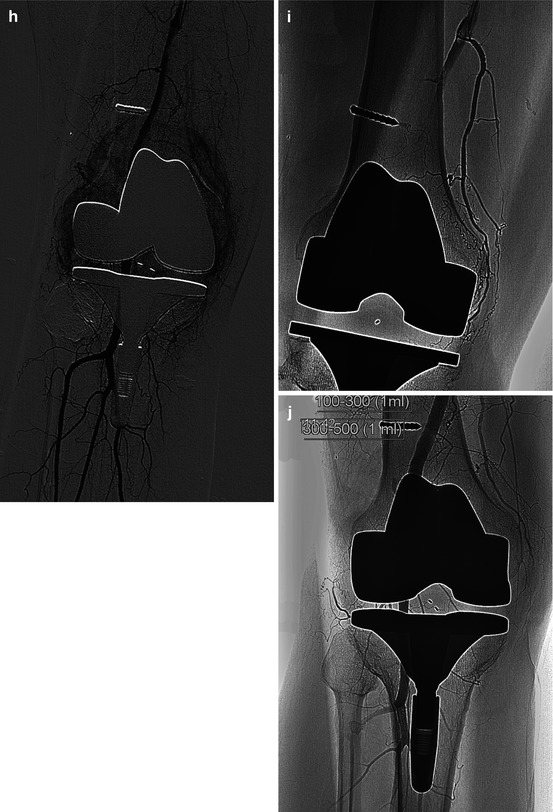
Fig. 24.3




A 62-year-old active patient who was operated 9 months ago of a total knee replacement to a multi operated left knee. After uneventful few weeks, a swelling of the left knee, without biological anomaly, has led to three successive punctures, finding hemarthrosis. There was not any disorder of hemostasis. (a–d) Antegrade groin puncture of the right common femoral artery, injection on the knee level, early and late phases: articular hyperemia in internal and external compartments. (e–i) This hypervascularization was essentially provided by two collateral arteries belonging to the periarticular circle of the knee: one emerging anteriorly from the popliteal artery above the prosthesis, which vascularize the outer compartment (e and f: selective injection in lateral view) and the other arising from the internal lateral edge of the distal SFA, supplying the inner compartment (g, h, and i: frontal view). These both two arteries were embolized by microparticles (diameter: 100–300 μm and then 500–700 μm). (j) Final angio control
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


