Miscellaneous Mediastinal Tumors (Paraganglioma, Vascular and Lipomatous Tumors, Other Sarcomas)
Borislav A. Alexiev, M.D.
Jennifer M. Boland, M.D.
Paraganglioma
Terminology
Paragangliomas are neuroendocrine tumors that arise in the extraadrenal sympathetic and parasympathetic paraganglia.
Incidence and Clinical
Paraganglioma in the mediastinum is extremely rare, accounting for 0.3% of all mediastinal tumors. The posterior mediastinum is the commonest site for mediastinal paraganglioma while anterior mediastinal localization is unusual.1 Paragangliomas are tumors of
adults, with a female predominance, and a peak incidence occurring during the third and fourth decade.1 Most paragangliomas are asymptomatic and present as painless masses.2,3 Clinical manifestations of mediastinal paraganglioma refer to a space-occupying mass and include hoarseness, dysphagia, chest pain, cough and, occasionally, superior vena cava syndrome. Patients may have symptoms related to excess secretion of catecholamines.4 Multiple paragangliomas occur in 22% of patients.4 Paragangliomas may occur sporadically or in association with several hereditary tumor syndromes, including neurofibromatosis type 1, von Hippel-Lindau disease, Carney triad, multiple endocrine neoplasia type 2, and pheochromocytoma-paraganglioma syndrome.5,6,7 Therefore, genetic testing should be considered in all patients with paraganglioma. Aggressive growth and metastases are observed in ˜20% of mediastinal paragangliomas.
adults, with a female predominance, and a peak incidence occurring during the third and fourth decade.1 Most paragangliomas are asymptomatic and present as painless masses.2,3 Clinical manifestations of mediastinal paraganglioma refer to a space-occupying mass and include hoarseness, dysphagia, chest pain, cough and, occasionally, superior vena cava syndrome. Patients may have symptoms related to excess secretion of catecholamines.4 Multiple paragangliomas occur in 22% of patients.4 Paragangliomas may occur sporadically or in association with several hereditary tumor syndromes, including neurofibromatosis type 1, von Hippel-Lindau disease, Carney triad, multiple endocrine neoplasia type 2, and pheochromocytoma-paraganglioma syndrome.5,6,7 Therefore, genetic testing should be considered in all patients with paraganglioma. Aggressive growth and metastases are observed in ˜20% of mediastinal paragangliomas.
Gross Pathology
Paragangliomas are solid tumors and are partially or completely encapsulated in a thin capsule. They frequently have a soft, heterogeneous, red-brown/mahogany cut surface.
Microscopic Pathology
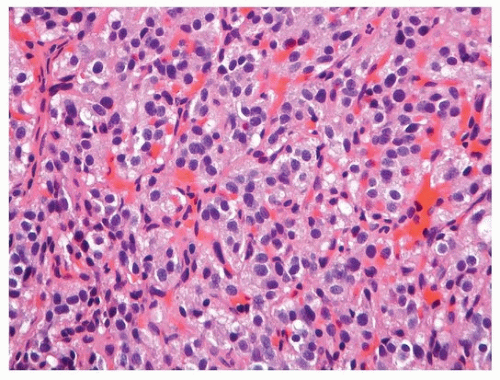
Histologically, the organoid-nested pattern (“zellballen”) of the normal paraganglion is seen in these tumors (Fig. 137.1). However, a wide range of variant morphology may be observed, including trabecular, spindled, or angioma-like patterns. Paragangliomas are composed of two cell types: (a) chief cells, which have abundant slightly granular cytoplasm with round or oval nuclei; and (b) sustentacular cells, which are inconspicuous spindled cells usually arranged around the periphery of the cell nests. There is a prominent delicate capillary vascular network. Mitotic figures are rare.
Special Studies
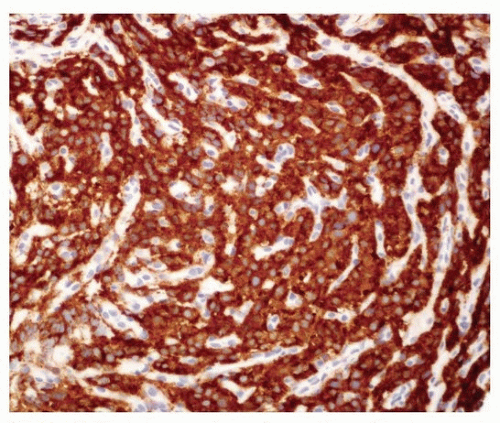
Immunohistochemically, neuroendocrine markers such as chromogranin A, synaptophysin, and CD56 are usually positive in chief cells (Fig. 137.2).1,4 S100 and GFAP immunostaining is present in sustentacular cells. Electron microscopy demonstrates neurosecretory granules in tumor cells.
Differential Diagnosis
Tumors that should be differentiated from mediastinal paragangliomas include well-differentiated neuroendocrine tumor (carcinoid), metastatic medullary thyroid carcinoma, and glomangioma. Carcinoid tumors typically express keratin, in contrast to paragangliomas, and lack sustentacular cells. Medullary thyroid carcinoma usually expresses calcitonin, and may have recognizable amyloid deposits. Glomangiomas lack expression of neuroendocrine markers and usually express smooth muscle actin.
Treatment and Prognosis
It is generally accepted that a paraganglioma is determined to be malignant only when metastases are demonstrated, as histologic criteria do not reliably predict malignancy. The treatment of choice for paraganglioma is surgical resection; most tumors are benign and can be excised totally.8,9 The surgery of anterior and middle mediastinal paragangliomas is challenging because of their close proximity to the central airways, heart, and great vessels, making complete resection difficult. Preoperative embolization is an established technique to reduce operative blood loss.2 In these cases, the pathology may see evidence of intra-arterial microspheres with a foreign body reaction adjacent to the tumor.
Lymphangioma
Terminology
Lymphangioma is a benign cavernous/cystic vascular lesion composed of dilated lymphatic channels. Early or congenital age of onset favors a developmental malformation.
Incidence and Clinical
Mediastinal lymphangioma is rare, accounting for 0.7% to 4.5% of all mediastinal tumors.10,11,12,13,14,15,16 The lesions may remain asymptomatic for years. Most are found incidentally in adulthood, or become apparent with manifestations related to compression of intrathoracic structures, including respiratory symptoms or dysphagia.15 Preoperative diagnosis is difficult and most of them are diagnosed intra- or postoperatively. Computed tomographic scans generally show a homogeneous, low-attenuation mass that often involves vascular or airway structures.
Gross Pathology
Lymphangiomas may be well capsulated, smoothly marginated, unilocular, or multicystic, with cavities containing watery/milky fluid. They may involve adjacent structures and viscera, or infiltrate soft tissue.
Microscopic Pathology
Lymphangiomas are characterized by thin-walled, dilated lymphatic vessels, lined by flattened endothelium, and frequently surrounded by lymphocytic aggregates. Stromal fibrosis with chronic inflammation, mast cells, and hemosiderin deposits are common.
Special Studies
The endothelium in lymphangiomas expresses D2-40, PROX1, CD31, and CD34.
Differential Diagnosis
The differential diagnosis includes hemangioma and various subtypes of hemangioendothelioma. D2-40 expression in the endothelial cells is helpful to support a lymphatic phenotype, and Prox1 is generally absent in capillary and cavernous hemangiomas. The lymphocyte aggregates commonly seen in lymphangioma are also not commonly seen in other vascular lesions.
Treatment and Prognosis
The standard treatment has been surgical excision, but frequent involvement of adjacent vital structures often makes total excision virtually impossible.15 Malignant transformation does not occur. However, recurrences occur in up to 20% of cases and are minimized by complete resection of the tumor.15 Deaths due to mediastinal lymphangioma are rare, and overall survival matches that of the general population.15
Hemangioma
Terminology
Hemangiomas have been traditionally classified according to the vessel size, into capillary and cavernous types, although most are mixed. Hemangiomas can be composed almost exclusively of veins of variable size, often having thick muscular walls (venous hemangioma).
Incidence and Clinical
Hemangiomas are rare benign vascular lesions estimated to constitute about 0.5% of all mediastinal tumors.17 Most mediastinal hemangiomas are located in the anterior mediastinum,18,19 and a few have been reported in the posterior mediastinum.17,19,20,21 A small number are of proven thymic origin.18,22 Seventy-five percent of the lesions appear before the age of 35 years, though they have been found between 2 months to 76 years of age.19,20,23,24 There is no gender preponderance. Nearly half of all patients are symptomatic. The main symptoms include cough, chest pain, dyspnea, hoarseness, and dysphagia. Rarely, patients with mediastinal hemangioma present with bloody pleural effusion.21
Gross Pathology
Microscopic Pathology
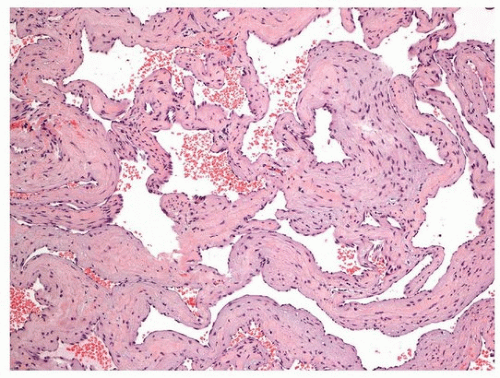
Histologically, the tumors can be divided into capillary and cavernous types based on vessel size, although these types are often intermixed and do not have clinical relevance. Capillary hemangiomas are characterized by a lobular and solid growth pattern featuring anastomosing and dilated small vascular channels lined by flattened endothelial cells without atypia. Cavernous hemangioma (Fig. 137.3) is characterized by large dilated vascular spaces filled with blood, often with areas showing interstitial inflammatory changes, fibrosis, and smooth muscle proliferation. Prominent regressive changes, including stromal hyalinization, dystrophic ossification, cystic and perivascular myxoid changes, and extensive fatty overgrowth, may be observed.19,24 In some cases, it may be difficult to determine whether the lesion represents a cavernous hemangioma or an arterial-venous malformation. The endothelial cells lining the vascular spaces are bland without atypia. Venous hemangiomas typically consist of large thick-walled muscular vessels, which are variably dilated and commonly display thrombosis.25 Widely dilated vessels can show attenuation of their walls, mimicking a cavernous hemangioma.
Special Studies
Elastic stains reveal the absence of an internal elastic lamina. Immunohistochemical examination of the lining cells shows positivity for CD31, FLI1, FVIII, and CD34, consistent with a lesion of endothelial origin.
Differential Diagnosis
The differential diagnosis includes lymphangioma, arteriovenous malformation, and various subtypes of hemangioendothelioma. Absence of an internal elastic lamina aids in the distinction from an arteriovenous malformation, and this distinction is often clear on radiographic grounds, so correlation with radiographic and clinical features is often helpful. D2-40 and Prox1 expression is present in lymphangioma and is generally absent in capillary and cavernous hemangiomas. Hemangioendotheliomas are vascular tumors of intermediate malignancy. The subtype most commonly encountered in the mediastinum is epithelioid hemangioendothelioma (EHE), which generally does not form extracellular vascular structures, and therefore is readily distinguished from hemangioma based on morphologic features (see Chapter 93).
Treatment and Prognosis
The treatment of choice for mediastinal hemangioma is surgical resection. In general, tumors are excised without significant complication, although rarely bony invasion necessitates complex surgery.26 Recurrences have not been reported for mediastinal hemangiomas.
Angiosarcoma
Terminology
Angiosarcoma is a malignant tumor that recapitulates the morphologic and functional features of endothelium to a variable degree.
Incidence and Clinical
Angiosarcoma is a rare neoplasm, accounting for only 1% to 2% of all sarcomas. It occurs most frequently in the skin and soft tissue and
rarely in the in the thoracic region. Those in the mediastinum occur most frequently in the pericardium, right side of the heart, and aorta.27 Rarely, they involve the anterior mediastinum without involvement of the pericardial space.28,29,30,31
rarely in the in the thoracic region. Those in the mediastinum occur most frequently in the pericardium, right side of the heart, and aorta.27 Rarely, they involve the anterior mediastinum without involvement of the pericardial space.28,29,30,31
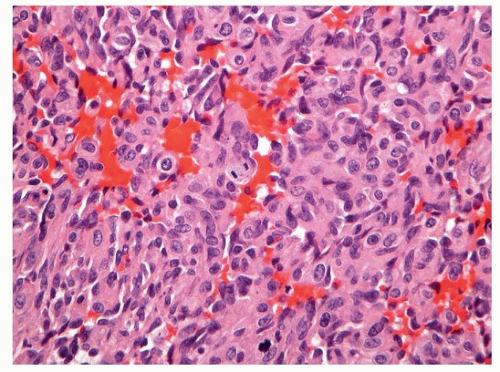 FIGURE 137.4 ▲ Angiosarcoma. Note high-grade epithelioid and spindled cells without clear vasoformation (H&E, ×200). |
Angiosarcomas affect patients of all ages (mean 40.7 years). There is a slight male predominance. The main presenting symptoms of mediastinal angiosarcomas include chest pain, dyspnea, and cough.
The occurrence of an angiosarcomatous component in mediastinal germ cell tumors is an uncommon phenomenon.30
Gross Pathology
Macroscopically, the lesions are multinodular hemorrhagic masses with ill-defined margins.
Microscopic Pathology
Angiosarcomas display a wide range of morphologic appearances, ranging from areas of well-formed, anastomosing vessels to solid sheets of high-grade epithelioid, hobnailed or spindled cells without clear vasoformation (Fig. 137.4).28,29,30,31 Multiple patterns may be present in the same tumor. Tumor cells have irregular, hyperchromatic, or vesicular nuclei and prominent nucleoli. Cytoplasm is eosinophilic with ill-defined borders. Hyaline globules may be seen. The tumor has infiltrative margins. Extensive hemorrhage is a characteristic feature.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree