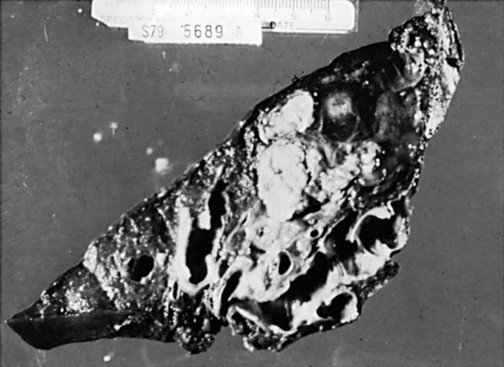
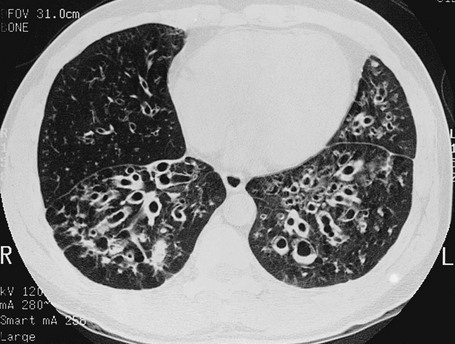
7 Another factor that plays a role in some patients is a defect in the ability of the airway to clear itself of, or protect itself against, bacterial pathogens (see Chapter 22). Such a defect predisposes a person to recurrent infections and eventually to airway dilation and bronchiectasis. The abnormality may involve inadequate humoral immunity and insufficient antibody production (hypogammaglobulinemia) or defective leukocyte function. Another problem that has received significant attention is dyskinetic cilia syndrome, in which ciliary dysfunction affects the ability of the ciliary blanket that lines the airway to clear bacteria and protect the airway against infection. The ciliary dysfunction is not limited to the lower airways; it also affects the nasal mucosa and, in males, may affect sperm motility and hence fertility. Pathologically, the dynein arms that are a characteristic feature of the ultrastructure of cilia are frequently absent in this disorder. One specific syndrome associated with bronchiectasis and ciliary dysfunction is Kartagener syndrome, which includes a triad of sinusitis, bronchiectasis, and situs inversus (usually discovered because of the presence of dextrocardia). The primary pathologic feature of bronchiectasis is evident on gross inspection of the airways, which are markedly dilated in the involved region (Fig. 7-1). Three specific patterns of dilation have been described: cylindrical (appearing as uniform widening of the involved airways), varicose (having irregularly widened airways resembling varicose veins), and saccular bronchiectasis (characterized by widening of peripheral airways in a balloonlike fashion). These terms are still used when describing radiographic patterns but are much less relevant clinically. The dilated airways are generally filled with a considerable amount of secretions that may be grossly purulent. Microscopic changes of the bronchial wall epithelium, consisting of ulceration and squamous metaplasia, are seen. Coexisting disease in the remainder of the tracheobronchial tree is common. Other areas of bronchiectasis may be present, or generalized changes of chronic bronchitis may be seen (see Chapter 6). High-resolution computed tomography (HRCT) provides a definitive diagnosis and is the initial procedure used to define the presence, location, and extent of bronchiectasis (Fig. 7-2). HRCT (with sections 1-2 mm thick) provides excellent detail and is particularly useful for detecting subtle bronchiectasis. In the past, the definitive diagnosis depended on bronchography, a radiographic procedure in which an inhaled opaque contrast material was used to outline part of the tracheobronchial tree (Fig. 7-3). This procedure is uncomfortable, can induce bronchospasm, and is not performed today. Figure 7-3 Bronchogram of patient with extensive saccular bronchiectasis, primarily in right upper lobe. The three major aspects of treatment of bronchiectasis are antibiotics, bronchopulmonary drainage (clearance of airway secretions), and bronchodilators. Antibiotics are used in various ways. Some patients are treated only when the quantity or appearance of the sputum clearly changes. Other patients, especially those who have severe disease and frequent exacerbations, are given a regimen of intermittent or even continuous antibiotics in an attempt to control chronic infection. Oral agents such as amoxicillin and trimethoprim-sulfamethoxazole, which are effective against many strains of Streptococcus pneumoniae and Haemophilus influenzae, are often used in patients with bronchiectasis. Inhaled tobramycin is sometimes used prophylactically to diminish the growth of gram-negative organisms. When these patients are infected with Pseudomonas organisms, treatment is generally more difficult. Oral fluoroquinolones such as ciprofloxacin have become useful therapy for Pseudomonas infection as an alternative to parenteral antibiotics, but secondary development of resistance to this class of antibiotics is common. Infection with M. avium complex requires prolonged therapy with multiple drugs (see Chapter 24
Miscellaneous Airway Diseases
Bronchiectasis
Etiology and Pathogenesis
Pathology
Diagnostic Approach

Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Miscellaneous Airway Diseases