13
Mining
The occupation of mining was one of the first to attract attention for its occupational diseases, with records going back to Roman times. In the tenth century miners were noted to be suffering from an illness called ‘bergsucht’ which was probably a composite illness caused by exposures to mercury, arsenic and silica and by hookworm infestation. The role of dust as a major factor in the illnesses of miners was recognized in the seventeenth century and was probably associated with the increase in respirable dust in the mines induced by the introduction of gunpowder and of primitive drilling apparatus in that century. As mines became deeper and explosives and drilling became more efficient towards the end of the nineteenth century, the effect of silica-containing dusts dominated and miners, especially those working at the rock face, became ill and died from acute silicosis and silico-tuberculosis. The life expectancy of a miner working at the rock face in mines with hard rock (quartz) was often no more than 5 years from the start of work. Since the latter half of the twentieth century, mines have been subject to regulations and laws which govern their environment and working conditions. Nevertheless in smaller mining operations and mines in industrializing countries, working conditions can be poor and the prevalence of occupational diseases high. When considering lung diseases in current or former mine workers, it is common to concentrate on mineral dust exposure such as silica, coal and asbestos, but the mine environment is complex and workers are exposed to contaminated water, gases, fumes and other particulates. This chapter deals with the topic of pneumoconiosis (mineral dust-induced lung fibrosis) and also the broad range of thoracic disorders and diseases which may be associated with mining.
It is difficult to know how many people are currently employed as miners. Mining has progressively become more mechanized with a resultant reduction in the number employed in mines. Many national statistics provide data for the number of workers at risk from diseases such as silicosis and do not necessarily separate those who work in nonmining environments from those who work as miners. In the USA it has been estimated that 1.7 million workers are exposed to respirable silica in industries including mining, quarries, foundries, construction, concrete rehabilitation, masonry and agriculture. In the USA the number of coal miners has decreased from 130,000 to 100,000 over the last 20 years, while coal production has increased by 169 million to 1.15 billion tons per year. The world production of coal in 2007 was over 7 billion tons. Mines outside of USA are less mechanized and thus employ many more miners; for example, it is estimated that there are 6 million coal miners in China, which produces 2.8 billion tons of coal per year. Asbestos is still being mined, with approximately 2.4 million tons produced each year. The number of miners employed in asbestos mines is uncertain. In the USA, where asbestos mining has ceased, 1.3 million workers are currently exposed to asbestos in other occupations.
In general, the number of those currently employed as miners is less relevant than the number who have worked in these occupations over the past several decades. Miningrelated occupational lung diseases, especially pneumoconioses, may first become apparent many years after cessation of exposure, and even if all mining were to stop immediately, there would be a substantial incidence of pneumoconioses and other mining-associated diseases for many decades.
The mining environment is complex and is contributed to not only by the activities directly associated with mining, but also by a very large support system including access, ventilation, refrigeration, humidification, electrical supply and equipment, waste disposal and activities associated with exploration and development. Specific aspects of a mine environment vary according to the substance being mined and whether the mine is a surface or an underground mine.
In general, underground mines have a more hazardous environment than surface mines, but substantial risks for exposure to dust and trauma exist for surface miners. Miners may be exposed not only to mineral dusts, notably crystalline silica, coal dust and asbestos, but also to general dust, diesel, radon, arsenic, mercury and other fumes and hazardous gases. Hazardous gases encountered in mining include nitrous oxides generated from explosions, welding and diesel, chlorine used for water treatment and gaseous products from other material, including cadmium, which can have a serious impact on the respiratory tract and the lungs. Microbiological agents including nontuberculous mycobacteria and parasites may be in the soil or carried into the mining environment by the water used to control dust. Mine living conditions, especially in industrializing countries, may include hostel living, which can be associated with the risk of transmissible diseases including tuberculosis, typhoid, meningococcal disease and pneumococcal pneumonia. Infection with HIV has become a major illness associated with mining where miners are migrant laborers separated from their families. The occupation of mining is also strongly associated with the risks of trauma and burns and of heat-associated disorders. Average geothermal gradients are 25° C per kilometer, which would translate into rock temperatures of 50° C in a modestly deep mine 1000 m below the surface. At these high rock temperatures failure of the ventilation and cooling system can cause heatrelated illnesses which may indirectly affect the respiratory tract through loss of consciousness, seizures and aspiration, while acute respiratory distress syndrome has been noted in some patients with heat stroke. Less obvious causes of illness in the mining environment include water borne diseases from the use of nonpotable water and poor toilet arrangements. Diseases in these categories include leptospirosis which can cause lung hemorrhage. Humidifier fever, which is thought to be caused by inhalation in a humidified environment of bacteria, endotoxins, fungi and protozoa in water, has not been reported in miners, but the environment is comparable with others where this disease has been prevalent. Similar exposures have also been related to hypersensitivity pneumonitis (extrinsic allergic alveolitis). Metalworking fluids, which may be aerosolized in the mining environment from drills and other machinery used in confined spaces, have also been associated with hypersensitivity pneumonitis and occupational asthma. Other materials used in mines, including methylene diphenyl diisocyanate (MDI) and other resins used in roof bolting systems, have the potential to cause occupational asthma and that diagnosis should be considered in a current or former miner with late-onset asthma. Cobalt, a component of tungsten carbide used for drills, is a recognized cause of occupational asthma and hypersensitivity pneumonitis, but is more likely to affect those who manufacture or sharpen drills than miners who use them. In general, although there are no clear data, it is appropriate to remain alert to the possibility of an association between mining and occupational asthma or hypersensitivity pneumonitis (extrinsic allergic alveolitis). Other specific respiratory illnesses associated with mining will be detailed.
The common pneumoconioses, silicosis, asbestosis and coal workers’ pneumoconiosis, are the best known of the occupational lung disorders associated with mining. These diseases are caused by the inhalation of respirable particles of crystalline silica (usually quartz), coal dust and asbestos fibers, and the resultant inflammatory and fibrotic reaction in the lung issue. Mine dust levels are generally well controlled at a level expected to be below that associated with pneumoconiosis, but these diseases still occur, although now they occur more frequently in nonmining settings. Even in mines where dust control levels are, on average, within the required threshold limits, new cases of pneumoconiosis continue to be reported and it has been estimated that 1% of career miners exposed to the NIOSH recommended exposure limit of 0.05 mg/m3 respirable crystalline silica, as a time-weighted average, for up to a 10 hour workday during a 40 hour working week will develop silicosis. In reality, because average dust levels can hide significantly higher exposures and because dust measuring may not be a true reflection of the working environment, outbreaks of pneumoconiosis are still reported. There are also some data to suggest individual susceptibility to the adverse effects of mineral dusts and a diagnosis of pneumoconiosis should not be rejected on the basis of work in an apparently well-controlled environment. In North America cases of pneumoconiosis in miners continue to be reported and in a recent report coal workers’ pneumoconiosis in young miners seems to be associated with work in small mines, which suggests that there might be an issue with dust control. Pneumoconiosis is often seen in older people who were exposed to mine dust at a time when dust control and recommended exposure limits were much less stringent. In those circumstances, even short periods of exposure such as pre-university or summer jobs might have produced sufficient lung dust burden. Pneumoconiosis may only become apparent years after cessation of exposure and occupational histories should not discount apparently remote work in mining. Working miners with pneumoconiosis should be encouraged to avoid further mineral dust exposure.
In general, pneumoconiosis is defined and categorized by the chest radiograph. A high-resolution computerized tomogram (CT) of the chest can be used in cases of doubt, but the plain chest radiograph is usually used for surveillance and for diagnosis of pneumoconiosis. The International Labour Office produces a set of standard radiographs and an instruction manual that are widely used to establish and categorize pneumoconiosis in individuals with an appropriate occupational history.
Silicosis is caused by the inhalation of dust containing crystalline silica, usually in the form of quartz. Quartz is found in many mines, notably gold mines but also in other mines including uranium, zinc, tin and copper mines and in coal mines where the coal seam is narrow and the grade of coal is high, as in anthracite.
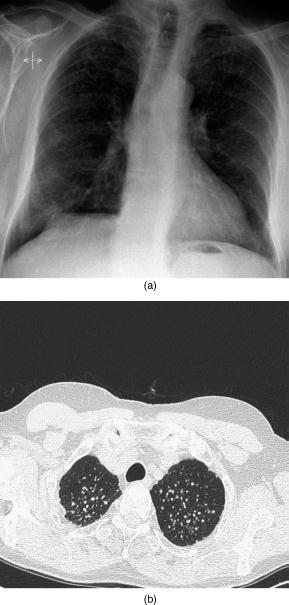
Silicosis in miners is nearly always the chronic and rarely the accelerated variety. Chronic silicosis usually becomes apparent after two or more decades of exposure, and is characterized by small nodular lung opacities which predominate in the upper lung zones (Figure 13.1). Hilar and mediastinal lymph node enlargement may not be obvious on the plain chest radiograph but is often noted on chest CT. Lymph node calcification of the eggshell variety may be present and is characteristic but not unique for silicosis. Accelerated silicosis will develop with more intense dust exposure of less than 15 years duration and also produces nodular opacities which are usually more uniformly distributed.
Figure 13.1 The chest radiograph (a) demonstrates an example of chronic silicosis with rounded opacities measuring between 3 mm (q) and 5 mm (r) with nodule profusion assessed by comparison with the ILO standard radiographs of 2 to 3 – 2/3 q/r. The apparently cystic lesion in the right upper mid zone was of concern regarding tuberculosis, but no suggestive lesion was seen on the CT, a representative example of which is seen in (b). The subject was assessed for tuberculosis. Sputum induced with nebulized 5% saline was negative on smear and culture for mycobacteria. Assessment for latent tuberculosis infection was done by a tuberculin skin test which measured 10 mm. This was thought to relate to his vaccination with Bacille Calmette-Guérin (BCG) as a schoolboy because an interferon γ release assay was negative
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


