(1)
Department of Neuroscience, University of Turin Ospedale Molinette, Turin, Italy
Abstract
The middle cerebral artery (MDA) arises as a secondary branch from the ACA and develops to the largest artery, supplying a large part of the cerebral hemispheres and basal ganglia. The development of the MCA correlates with the great extension of the cortical mantel in the mammalian (Kier 1974). It can be divided into four segments (Figs. 5.1 and 5.2):
The middle cerebral artery (MDA) arises as a secondary branch from the ACA and develops to the largest artery, supplying a large part of the cerebral hemispheres and basal ganglia. The development of the MCA correlates with the great extension of the cortical mantel in the mammalian (Kier 1974). It can be divided into four segments (Figs. 5.1 and 5.2):
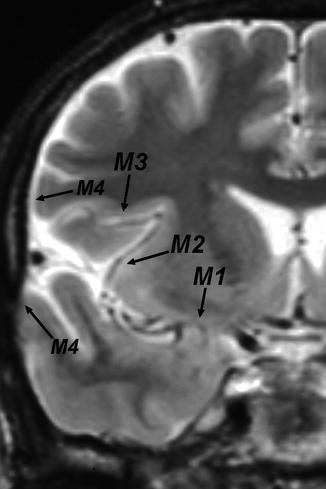
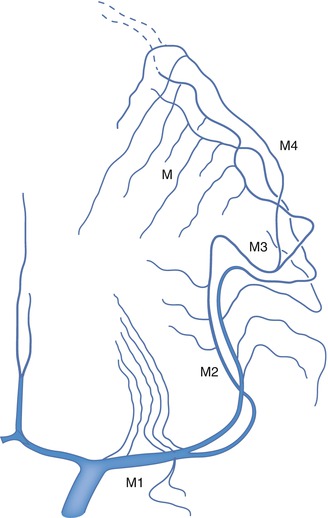
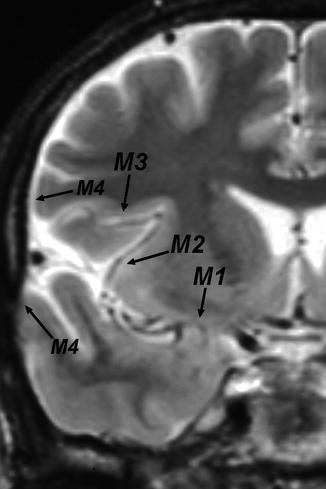
Fig. 5.1
RM Coronal: The MCA runs first horizontally in the sylvian cistern (M1), then on the surface of the insula (M2), further laterally (M3) exiting the insular cistern, and reaching the convexity (M4)
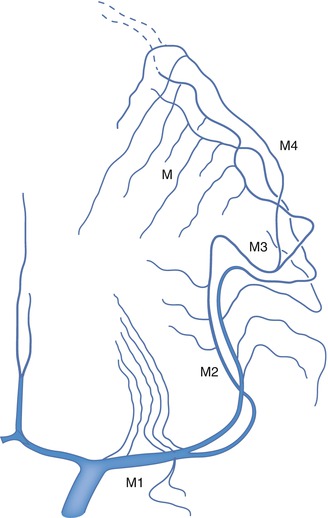
Fig. 5.2
Segments of the MCA: M1, M2, M3, and M4. Deep perforators arising from the M1. Medullary arteries (short and long branches) arising from the cortical branches (M). Anastomoses with the anterior cerebral artery (———-)
M1 segment, running horizontally in the sylvian fissure
M2 segment, running vertically on the surface of the insula
M3 segment, running laterally and exiting the insular cistern
M4 segment, which comprises the distal cortical branches
5.1 M1 Segment
The first segment (M1) arises at the ICA bifurcation and runs horizontally and laterally in the sylvian fissure below the anterior perforated substance (APS) toward the insula. Also called the sphenoidal segment because it runs parallel 1 cm posterior to the sphenoid ridge, the M1 ends at the limen insulae, where it sharply turns superiorly and posteriorly to form the M2 segment. The M1 divides distally into two or three branches (bi-trifurcation). Its length varies; it is, on average, 16 mm in length (Umansky et al. 1985). It can be very short, and so the bi-trifurcation may be located near the bifurcation of the ICA. It gives off two types of important branches.
Perforators. Since the first anatomical description of perforating branches by Duret (1874), many detailed studies have been performed. Also called the lenticulostriate arteries, these branches arise along the length of the M1 from its superior surface. They arise prevalently from the prebifurcation segment, more rarely from the post-bifurcation or M2 segment (Westberg (1966); Rosner et al. 1984). The branches can be subdivided into medial, intermediate, and lateral groups. The medial are the least constant and can be replaced by the artery of Heubner (Rosner et al. 1984). In the microanatomical study of Umansky et al. (1985), the perforators of the MCA were partially replaced by the perforators of the anterior cerebral artery (ACA), especially by the artery of Heubner, in 26 % of cases. The medial branches have a straight course, the intermediate a slightly tortuous course, and the lateral display the typical S-shaped aspect (Fig. 5.3).
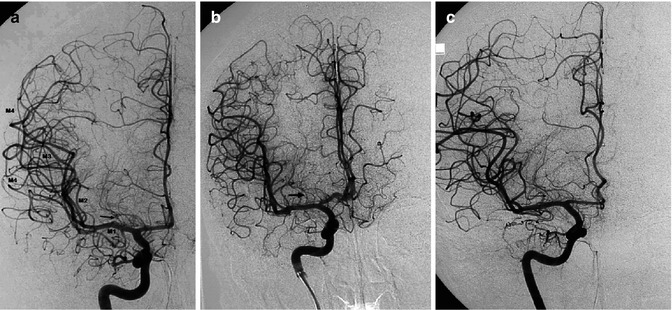
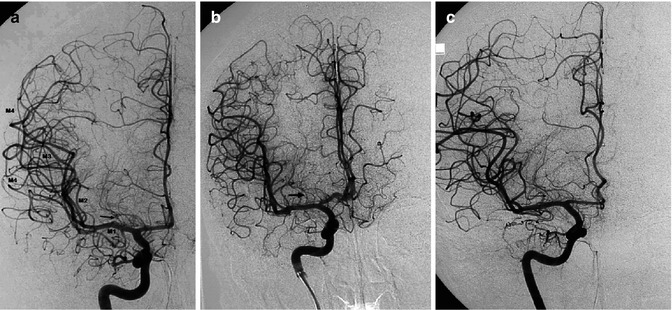
Fig. 5.3
AP angiograms (a, b, c): Examples of a long M1 segment, from which arise the perforators prevalently grouped in the intermediate segment of the M1. The more distal perforators show the typical S shape (arrow). In (a), a temporal branch arising from the M1 is also present, running anteriorly and inferiorly to the temporal pole. Distally to the bifurcation, the branches of the middle cerebral artery run on the surface of the insula (M2), turn further laterally (M3), exiting finally from the insular cistern, and reaching the convexity (M4). In (b), there is minimal fenestration of the A1
The shorter the M1 segment with an early bifurcation, the greater is the number of perforators arising near its bifurcation, immediately proximal or distal to it from one of the post-bifurcation branches (Kaplan 1965; Lazorthes et al. 1976; Rosner et al. 1984; Umansky et al. 1985) (Figs. 5.4 and 5.5). Perforators can originate as a common trunk (Umansky et al. 1985), and we have observed cases in which perforators and distal cortical branches arose from a common trunk (Fig. 5.5b).
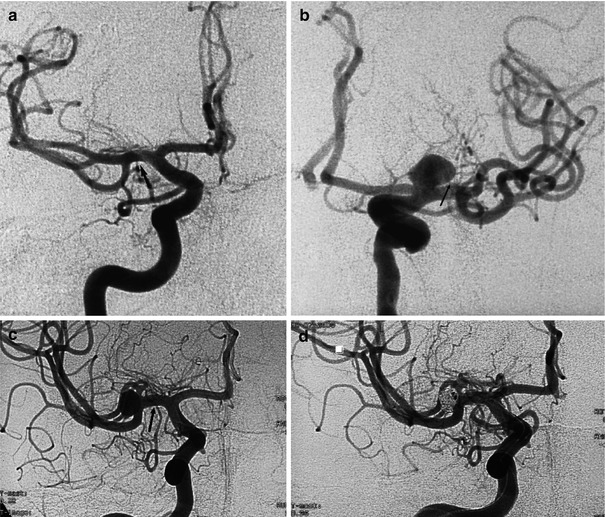
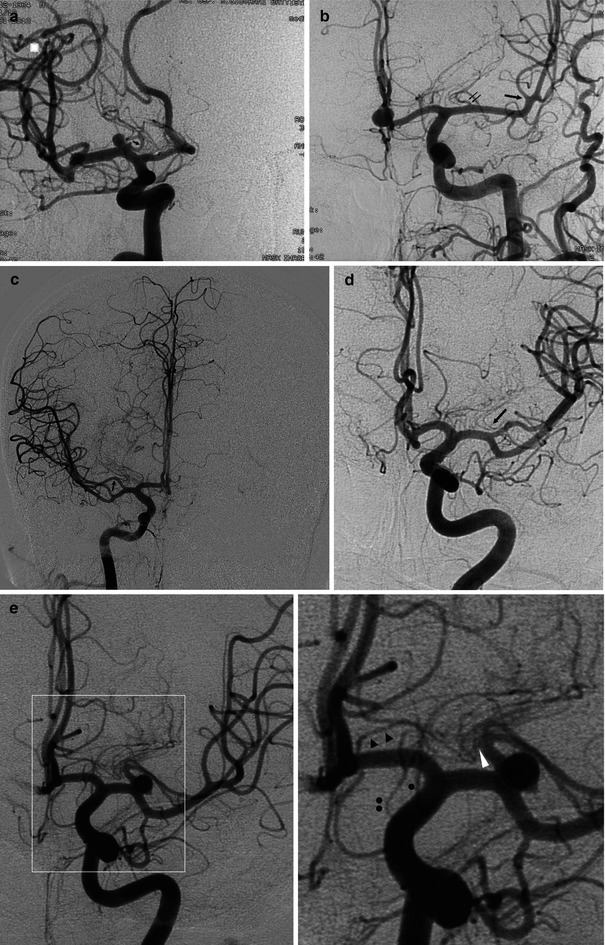
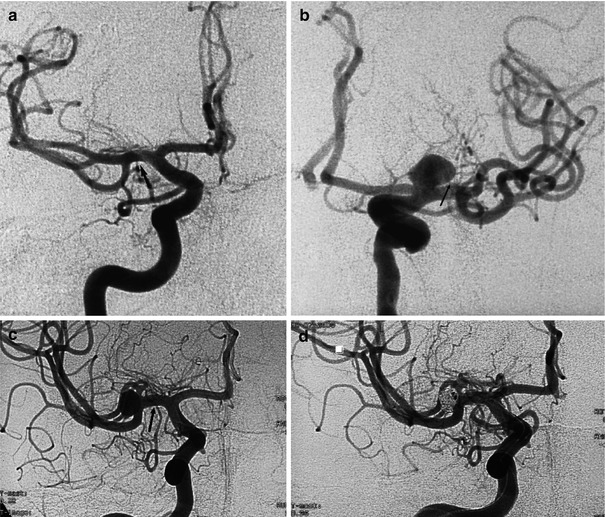
Fig. 5.4
(a) An apparently very short M1 (arrow) owing to the early arising of a large temporal branch. The main trunk from which arise the perforators bifurcates more distally. (b) Large aneurysm with a neck at the carotid bifurcation, showing partial involvement also of the proximal middle cerebral artery. Because of the short M1, the origin (arrow) of the perforators is close to the aneurysm. (c, d) A very short M1 (arrow) gives off perforators that are close to the trifurcation, from which arises an aneurysm, treated with coils
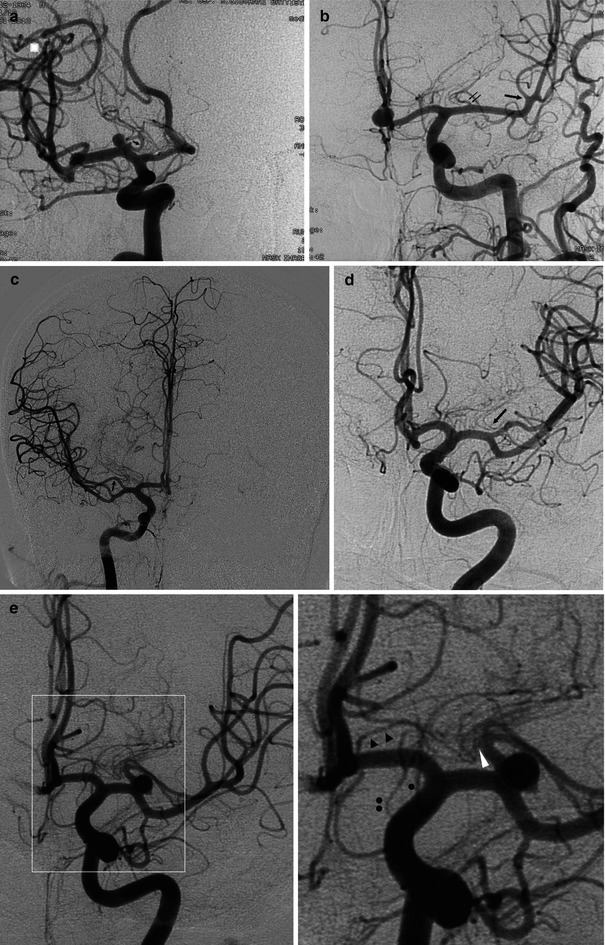
Fig. 5.5
(a) Oblique view in a patient examined for an unruptured aneurysm with a neck located on the M1 segment at the junction of a large perforator. This seems to be almost the only trunk (arrow) from which all distal perforators arise. (b) AP view in a patient examined for ruptured aneurysm of the anterior communicating artery. There is a long M1 with a trifurcation, from which the M2 branches arise located distally (large arrow). From the M1 arises a common trunk (arrows), giving off perforators and distal insular and temporal branches. A few other perforators seem to originate from the A1. (c) Another example of anomalous bifurcation, AP view. The M1 segment is very short. It divides into a smaller superior branch (arrow), from which the perforators arise, and into a large inferior branch, which divides further distally. (d) On this right carotid angiogram, the medial perforators arise from the short M1, while the most lateral (arrow) originate from the superior branch distal to the bifurcation. (e) Left carotid angiogram discovering an incidental aneurysm of the middle cerebral artery. AP view and magnification. The aneurysm is located at the bifurcation of a short M1. The perforators of M1 (white arrow head) arise from the superior branch. One perforator seems to arise from A1. Heubner’s artery (black arrow heads). A.Ch.A. (a small black point). Hypoplastic PcomA (two small black points)
These different aspects concerning the deep perforators should be carefully considered in the surgical or endovascular treatment of aneurysms of the M1 segment. In addition, they explain the different patterns of ischemic lesions in the case of occlusion of the M1.
Perforators commonly enter the lateral part of the APS (Rosner et al. 1984; Rhoton 2002) and supply the superior part of the head of the nucleus caudatus and its body. They entirely supply the superior part of the internal capsule as well as the globus pallidus and putamen.
Cortical Branches. From the M1 segment arise frequently a branch for the pole of the temporal lobe and sometimes also an orbitofrontal branch for the pars orbitalis of the inferior frontal gyrus. In exceptional cases, a temporal branch arises from the ICA.
5.2 M2, M3, and M4 Segments
The M2 segment, also called the insular segment, begins at the limen insulae and runs on the surface of the insula in the sylvian insular cistern with a superior–posterior direction. The M2 segment consists of two or three branches that arise from the bi-trifurcation of the M1. After reaching the top of the insula, these branches turn inferolaterally and exit from the sylvian insular cistern, forming the M3 segment. The last segment, the M4, comprises the distal cortical arteries. From their course and the area they supply, the cortical branches can be divided into the orbitofrontal artery, the ascending frontal arteries (operculofrontal artery, central arteries), ascending parietal arteries (anterior and posterior), descending arteries (temporal branches), and the terminal group (gyrus angularis artery) (Ring and Waddington 1967; Ring 1974; Huber 1979; Gibo et al. 1981b). Overlaps in the course of the cortical branches and variations in their size and origin make it difficult in a given case to identify precisely the different arteries on an angiogram. On the basis of anatomical and angiographic studies, Michotey et al. (1974) and Salamon and Huang (1976) described two basic patterns that can help in identifying these arteries (Fig. 5.6a, b).
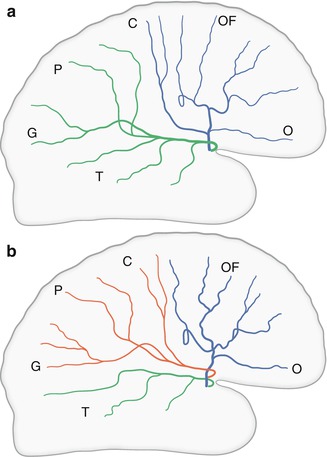
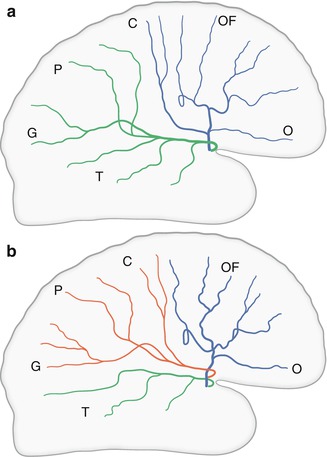
Fig. 5.6




(a) In the bifurcation pattern, the orbitofrontal (O), operculofrontal (OF), and central arteries (C) arise from the anterior trunk. All other branches—anterior and posterior parietal (P), gyrus angularis (G), and temporal (T) arteries—arise from the posterior trunk. (b) In the trifurcation pattern, the orbitofrontal (O) and operculofrontal (OF) arteries arise from the anterior trunk. The central (C), anterior and posterior parietal (P), and gyrus angularis (G) arteries arise from the middle trunk and the temporal (T) branches from the posterior branch
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


