Fig. 34.1
Serrated microdebrider blade

Fig. 34.2
Handpiece with suction tubing attached

Fig. 34.3
Console and foot pedal
History of the Microdebrider
Dr. Jack Urban is credited with the development of the first microdebrider. In the mid-1960s, Urban became interested in a better way to resect tissue in a small operative field and began work on a prototype of what he later called a “rotary vacuum dissector.” After further development, Urban secured a patent for his device in 1969. Though initially met with limited enthusiasm, the rotary vacuum dissector eventually gained credibility with physicians. Dr. William House began using the device in the early 1970s to remove acoustic neuromas. By the early 1980s, orthopedic surgeons began to employ the device to carry out arthroscopic procedures. The 1990s witnessed an explosion in the use of microdebriders, in part because of improved technology in debriders, but also in operating telescopes and microscopes. Currently, microdebriders are routinely employed by surgeons in a variety of procedures including nasal/sinus surgery, pharyngeal surgery, laryngeal surgery, tonsillectomy/adenoidectomy, airway interventions, joint surgery, and liposuction.
Proper Operative Technique
Patients undergo general anesthesia since microdebriders must be used with either a rigid bronchoscope or suspension laryngoscopy. The anesthesiologist and surgeon should develop a plan preoperatively and work in concert during the case to assure the best results. Once the case is underway, a telescope or microscope is employed in tandem with the microdebrider to give the surgeon proper visualization. This requires a bronchoscope, tracheoscope, or laryngoscope of sufficient diameter to accommodate the instruments. Commercially available airway blades range from 2.9 mm to 4 mm in diameter, while telescopes are typically 3 mm to 6 mm in diameter.
Scopes are selected based on the size of the patient and the anatomy of the lesion. For example, a mainstem bronchial lesion in an average-sized adult would be approached with a 12 mm diameter bronchoscope, whereas a proximal tracheal lesion might be approached with a 12 mm diameter tracheoscope. Lesions in the glottis or subglottis may be treated employing a Dedo laryngoscope.
Friable lesions are best resected with a serrated blade in an oscillating mode, while fibrous tissue is more amenable to a smooth blade with a unidirectional mode. Rotational speed controls the amount of tissue drawn into the blade aperture. Slow speeds (500–1,000 rpm) result in bigger tissue bites, while faster speeds (>1,000 rpm) result in smaller bites. Tissue is drawn into the blade aperture with suction; the operator can avoid inadvertent resection of normal airway tissue by employing this property to advantage. Newer microdebrider systems allow the surgeon to alter the direction of the tip of the blade by manipulating a dial on the handpiece, allowing even finer control of the blade aperture. Thermal modalities, such as argon plasma coagulation (APC), electrocautery (EC), or neodymium-doped yttrium aluminum garnet laser (Nd:YAG), must be available to deal with excessive bleeding should it occur. Employing rigid scopes wide enough to accommodate all the necessary instruments is paramount (Fig. 34.4).
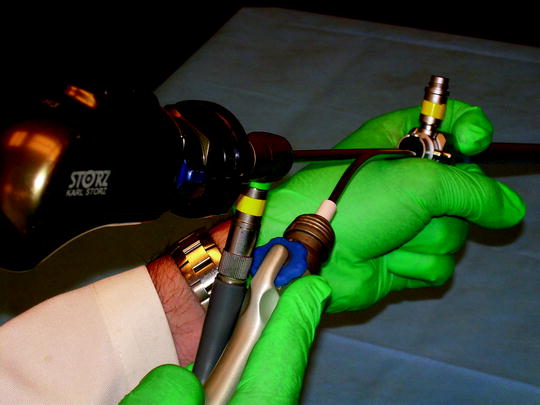
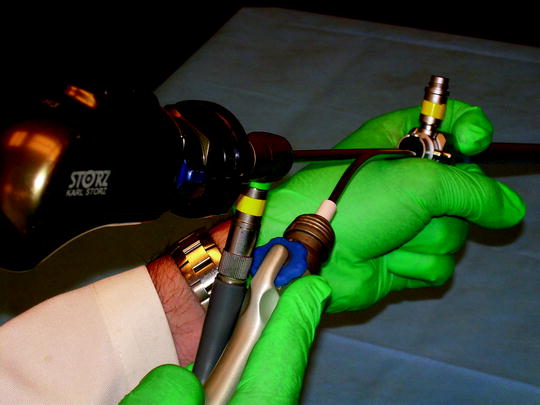
Fig. 34.4
Surgeon’s view of bronchoscope, microdebrider, and telescope
As with any surgical tool, misuse of the microdebrider may result in complications. There are three simple principles of microdebrider use in the airway. First, the surgeon should never deploy the blade past their field of vision: one cannot control what one cannot see. Figure 34.5 demonstrates proper positioning of the blade relative the operator. Second, the surgeon should avoid putting pressure on the airway wall with the microdebrider as this may lead to normal tissue being drawn into the blade aperture. Third, one must deploy the blade parallel to the airway wall, never perpendicular, as this may result in airway perforation. Perhaps the most-reported complication of employing microdebriders in all applications is accidental resection of or damage to surrounding normal tissue. Complications can be easily avoided by adhering to the principles above.


Fig. 34.5
Microdebrider resecting right mainstem bronchus tumor
Evolution of Use in the Airway
Since the microdebrider is a tool commonly employed by ENT surgeons in other applications, it should not be surprising that they found their way into the airway. In fact, surgeons had been using microdebriders for laryngeal problems and had even devised special “skimmer blades” for use on and around the vocal cords. Perhaps the best early demonstration of the utility of the tool in the airway was published by Simoni et al. in 2003. They described their experience using the microdebrider to rapidly establish a patent airway in 27 patients with advanced laryngotracheal carcinoma. All their patients received postoperative radiation therapy, with 24 of 27 avoiding tracheotomy. These results were so impressive that other surgeons were inspired.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


