Data regarding the efficacy and safety of zero or near-zero fluoroscopic ablation of cardiac arrhythmias are limited. A literature search was conducted using PubMed and Embase for relevant studies through January 2016. Ten studies involving 2,261 patients were identified. Compared with conventional radiofrequency ablation method, zero or near-zero fluoroscopy ablation significantly showed reduced fluoroscopic time (standard mean difference [SMD] −1.62, 95% CI −2.20 to −1.05; p <0.00001), ablation time (SMD −0.16, 95% CI −0.29 to −0.04; p = 0.01), and radiation dose (SMD −1.94, 95% CI −3.37 to −0.51; p = 0.008). In contrast, procedure duration was not significantly different from that of conventional radiofrequency ablation (SMD −0.03, 95% CI −0.16 to 0.09; p = 0.58). There were no significant differences between both groups in immediate success rate (odds ratio [OR] 0.99, 95% CI 0.49 to 2.01; p = 0.99), long-term success rate (OR 1.13, 95% CI 0.42 to 3.02; p = 0.81), complication rates (OR 0.98, 95% CI 0.49 to 1.96; p = 0.95), and recurrence rates (OR 1.29, 95% CI 0.74 to 2.24; p = 0.37). In conclusion, radiation was significantly reduced in the zero or near-zero fluoroscopy ablation groups without compromising efficacy and safety.
Owing to the often long duration of catheter ablation procedures, there is much concern about the radiation hazard to both patients and medical staff in the electrophysiology laboratory. Prolonged radiation exposure is associated with a higher incidence of dermatitis, cataracts, malignancies, and congenital defects. Since there is no definite level of exposure that is known to be completely safe, the utilization of ionizing radiation during medical diagnostic or interventional procedures should be as low as reasonably achievable (ALARA principle). Various measures, including the use of new 3-dimensional electroanatomical mapping software, intracardiac echocardiography (ICE), miniaturized transesophageal echocardiography, and contact force–sensing catheters, have led to a significant reduction or complete elimination of fluoroscopy in most patients, particularly in children, pregnant women, and patients with immune dysfunction. The data obtained from randomized clinical trials, in which zero or near-zero fluoroscopy ablation was compared with routine fluoroscopically guided procedures for cardiac arrhythmias, are relatively limited and inconsistent, and most trials are small and underpowered. We therefore performed a meta-analysis of clinical studies that compared outcomes for procedures using zero or near-zero fluoroscopy or conventional ablation in terms of fluoroscopic time, ablation time, procedure duration, immediate success, long-term success, complication rate, and recurrence rate in the treatment of cardiac arrhythmias.
Methods
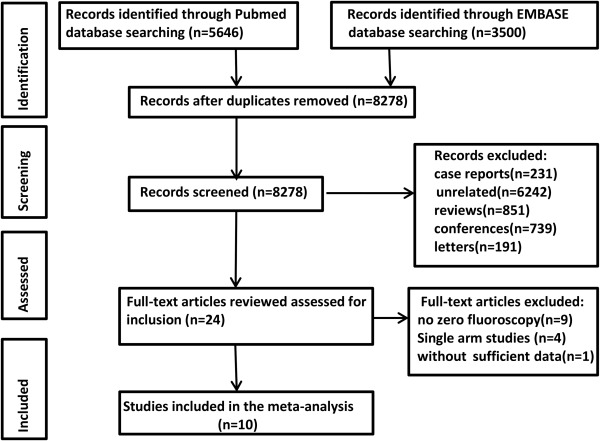
PubMed and Embase databases were searched for studies relevant to zero or near-zero exposure radiofrequency ablation of cardiac arrhythmias, and studies from January 1974 to January 2016 were included. The search strategies were as follows: (radiation or x-ray or fluoroscopy or fluoroscopic or fluoroscopically) and (catheter ablation); only human studies and those published in English were included. Manual searches of reference lists supplemented from potentially relevant studies were also conducted for any additional studies that may have been missed in the initial search.
Only data from full, published studies were used. No meeting or conference abstracts, letters, or case reports were included. Studies included in this meta-analysis (1) involved patients with cardiac arrhythmias requiring catheter ablation and compared the differences in fluoroscopic time, radiation dose, ablation time, procedure duration, acute success, long-term success, complications, or recurrence for procedures using zero or near-zero fluoroscopy and conventional ablation; (2) included patients treated with zero or near-zero fluoroscopy; and (3) were written in English. Review articles and duplicate publications were excluded. Each study was examined for inclusion and exclusion criteria by 2 independent investigators (Yang and Chen), and a consensus was reached on all items. All manuscripts were reviewed to ensure the most complete information possible.
Zero fluoroscopy was defined as the achievement of ablation entirely without the use of any fluoroscopy. Near-zero fluoroscopy was interpreted as planning for a procedure with no fluoroscopy, but very limited radiation use if considered necessary by the operator. Quantitative outcomes were summarized and compared by the standard mean difference (SMD) and 95% CI for zero or near-zero fluoroscopy ablation and conventional ablation. Categorical variables were evaluated for the 2 groups by the weighted odds ratio and corresponding 95% CI. For each study, weight was calculated as the reciprocal of the variance of the estimated intervention effect. The random-effects model using the DerSimonian and Laird method was adopted regardless of the existence of heterogeneity. Heterogeneity across studies was examined with the inconsistency index (I 2 ) test. Predefined subgroup analysis was conducted a priori according to study design (randomized and nonrandomized clinical studies). Publication bias was evaluated using the Begg’s and Egger’s tests. The trim-and-fill method was used to further assess the potential effect of publication bias. Statistical analyses were completed with Review Manager software (version 5.3, http://ims.cochrane.org/revman/download ) and Stata software (version 12.0 for Windows; StataCorp, College Station, Texas).
Results
Ten studies involving 2,261 patients met our selection criteria and originated from different countries between 2007 and 2015. The process of the literature search is summarized in Figure 1 . Of the 10 included clinical studies, 4 were randomized and 6 were nonrandomized. All studies used 3-dimensional localization systems for invasive electrophysiology. Baseline characteristics of all patients included are summarized in Table 1 .