The effects of radiofrequency catheter ablation (RFCA) on left atrial (LA) size, volumes, and function in patients with atrial fibrillation (AF) are not well understood. The aim of this study was to systematically review the effects of RFCA on LA size, volumes, and function in patients with AF. Medline, the Web of Science, the Cochrane Central Register of Controlled Trials, and the reference lists of retrieved reports were searched for relevant studies through April 2009. Studies conducted in patients with AF were included if their primary outcomes were changes in LA size or volumes and/or function before and after RFCA. Weighted mean differences for changes in LA diameter, LA maximum volume, LA minimum volume, LA ejection fraction, and LA active emptying fraction were estimated using fixed- and random-effects meta-analyses. Seventeen relevant studies (enrolling 869 patients) among 192 identified studies were included in the final analysis. Compared to preablation values, there were significant decreases in LA diameter and LA volumes at postablation follow-up. However, compared to preablation values, there were no significant differences in LA ejection fraction and LA active emptying fraction at postablation follow-up. Decreases in LA diameter and LA volumes remained significant in those without AF recurrence but not in those with AF recurrence. LA ejection fraction and LA active emptying fraction did not decrease in patients without AF recurrence, whereas they decreased in patients with AF recurrence. In conclusion, successful RFCA in patients with AF significantly decreases LA size and volumes and does not seem to adversely affect LA function.
Despite the wealth of data on the diagnostic and prognostic implications of left atrial (LA) size and volumes, the effects of radiofrequency catheter ablation (RFCA) on LA size, volumes, and function in patients who undergo RFCA are not well understood. We aimed to systematically review the effects of RFCA on LA size, volumes, and function in patients with atrial fibrillation (AF).
Methods
We searched Medline, the Web of Science, the Cochrane Central Register of Controlled Trials, and the reference lists of retrieved reports in April 2009 for studies of RFCA in patients with AF using the appropriate terms: “catheter ablation,” “atrial fibrillation,” “atrial size,” “atrial volume,” and “atrial function.”
Two investigators (VJ and ACJ) independently screened all titles and abstracts to identify studies that examined the effects of RFCA in patients with AF on LA size, volumes, and function. Only reports in English were included in this study. Two reviewers (VJ and SS) extracted relevant data from the included studies using a standardized data extraction form. Randomized and nonrandomized studies with follow-up imaging done ≥1 month after RFCA were considered for inclusion. Primary outcome measures were changes in LA diameter (LAD); LA maximum volume (LAVmax), defined as the maximal LA volume before the opening of the mitral valve; changes in LA minimum volume (LAVmin), defined as the minimal LA volume at the closure of mitral valve; changes in the LA ejection fraction (LAEF; defined as [LAVmax − LAVmin]/LAVmax), and the LA active emptying fraction (LAAEF; defined as [LA mid-diastolic volume at onset of p wave on surface electrocardiogram − LAVmin]/LA mid-diastolic volume at onset of p wave on surface electrocardiogram). Studies were excluded if the effects of RFCA on LA size, volumes, or ejection fraction were not reported before and after RFCA.
Studies reporting changes in LAD, LA volumes, and function on the basis of AF recurrence were analyzed separately to assess effects of RFCA in patients with AF recurrence compared to those without AF recurrence. Studies that did not separate the results on the basis of the recurrence of AF were analyzed together as combined studies. The total changes in LA size, volumes, and function for all studies (recurrent, no recurrence, and combined) were also analyzed.
The quality of included studies was assessed by exploring (1) study design, (2) the representativeness of the study participants with regard to patients who undergo RFCA for AF, (3) reporting of loss to follow-up, and (4) limitations and biases.
Statistical analyses were performed using Cochrane RevMan version 5, and the results are expressed as weighted mean differences (WMDs) for continuous outcomes, with 95% confidence intervals (CIs). Data were pooled using the DerSimonian-Laird random-effects model, but a fixed-effects model was also analyzed to ensure the robustness of the model chosen and susceptibility to outliers. Heterogeneity was analyzed using Cochran’s Q (heterogeneity chi-square, with n − 1 degrees of freedom) and the I 2 statistic, with a p value of 0.05 used for statistical significance. We planned to conduct sensitivity analyses if significant heterogeneity was found (I 2 > 50%) for any 1 of the outcomes. Sensitivity analyses included (1) fixed- versus random-effects model, (2) exclusion of studies with shorter durations of follow-up (<3 months), (3) exclusion of studies with lower left ventricular ejection fractions (<50%), (4) exclusion of studies with sample sizes <30 patients, and (5) analyses based on AF recurrence.
Results
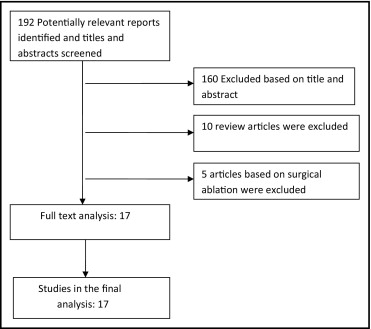
We identified 17 studies (enrolling 869 patients) that reported changes in LA size, volumes, or function in patients with AF who underwent RFCA ( Figure 1 ). Baseline characteristics of the studies included in the meta-analysis are listed in Table 1 . The primary outcomes of the studies included are listed in Table 2 .
| Study | Number of Patients | Follow-Up (mo) | Paroxysmal AF Persistent AF Permanent AF | Age (yrs) | Men | Co-Morbidities | Duration of AF in Hears | LVEF | Success Rate |
|---|---|---|---|---|---|---|---|---|---|
| Reant et al | 48 | 11 | 37 (77%) | 53 ± 9 ⁎ | 30 (75%) ⁎ | NA | 6 ± 5 ⁎ | 62 ± 5 ⁎ | 29/37 (78%) ⁎ |
| NA | NA | NA | NA | NA | NA | ||||
| 11 (23%) | 55 ± 11 † | 10 (91%) † | 12 ± 9 † | 53 ± 8 † | 6/11 (54%) † | ||||
| Wylie et al | 33 | 1.5 | 24 (73%) | 55 ± 12 | 25 (76%) | Mild MR (39%) | 5 | 64 ± 7 | 27/33 (82%) |
| 9 (27%) | Moderate MR (3%) | ||||||||
| NA | |||||||||
| Delgado et al | 34 | 6 | 23 (68%) | 53 ± 13 | 24 (70%) | HTN (24%) | 7 ± 6 | NA | 21/34 (62%) |
| 6 (18%) | ICM (excluded) | ||||||||
| 5 (15%) | Valvular (excluded) | ||||||||
| Lemola et al | 27 | 5 | 27 (75%) | 55 ± 11 | 18 (66%) | CAD (9%) | 5 ± 4 | 56 ± 5 | NA |
| NA | |||||||||
| 9 (25%) | |||||||||
| Verma et al | 26 | 6 | 40 (60%) | 56 ± 10 | 19 (73%) | HTN (31%) | 5.8 ± 5 | 50 ± 13 | NA |
| 27 (40%) | DM (9%) | ||||||||
| NA | CAD (19%) | ||||||||
| Valvular (15%) | |||||||||
| Perea et al | 55 | 12 | 41 (74%) | 52 ± 11 | 44 (80%) | HTN (22%) | 8.4 ± 8 | 60 ± 9 | 38/55 (69%) |
| 14 (26%) | Structural heart disease (16%) | ||||||||
| NA | |||||||||
| Beukema et al | 105 | 15 | 52 (49%) | 53 ± 9 | 88 (84%) | HTN (26%) | 6 ± 5 ⁎ | 54 ± 4 | 39/52 (75%) ⁎ |
| 53 (51%) | DM (5%) | 7.6 ± 6 ‡ | 32/53 (60%) ‡ | ||||||
| NA | |||||||||
| Choi et al | 33 | 3 | 21 (64%) | 56 ± 10 | 27 (82%) | CAD (6%) | 5 ± 4 | 53 ± 6 | NA |
| 12 (36%) | HTN (21%) | ||||||||
| NA | DM (6%) | ||||||||
| Valvular (6%) | |||||||||
| Lemola et al | 41 | 4 | 25 (61%) ⁎ | 54 ± 12 | 33 (80%) | Structural heart disease (41%) | 5 ± 3 | 55 ± 8 | 33/41 (80%) |
| 16 (39%) † | HTN (21%) | ||||||||
| Tsao et al | 45 | 21 | 45 (100%) | 60 ± 13 | 36 (80%) | NA | NA | NA | 35/45 (77%) |
| NA | |||||||||
| NA | |||||||||
| Tops et al | 57 | 3 | 35 (61%) | 53 ± 8 | 45 (79%) | HTN (30%) | 6 ± 5 | 54.5 ± 7 | 39/57 (68%) |
| 18 (32%) | Valvular (10%) | ||||||||
| 4 (7%) | CAD (7%) | ||||||||
| Rodrigues et al | 33 | 8 | 33 (100%) | 53 ± 13 | 22 (79%) | HTN (39%) | 6 | NA | 17/28 (61%) |
| NA | |||||||||
| NA | |||||||||
| Muller et al | 91 | 6 | 72 (79%) | 59 ± 8 | 79 (87%) | HTN (33%) | 6.4 ± 6 | NA | 70/91 (77%) |
| 11 (12%) | CAD (7%) | ||||||||
| 8 (9%) | |||||||||
| Marsan et al | 57 | 8 | 45 (79%) | 56 ± 9 | 44 (77%) | DM (11%) | 4.6 ± 4.1 | 57 ± 9 | 38/57 (67%) |
| 12 (21%) | HTN (44%) | ||||||||
| CAD (5%) | |||||||||
| Liu et al | 120 | 12 | 60 (100%) | 59 ± 9 (CPVA) | 40 (66%) | NA | 2.6 ± 1 | 67 ± 3 | 32/60 (53%) |
| 60 (100%) | 60 ± 9 (SPVI) | 40 (66%) | 2.6 ± 1 | 66 ± 4 | 46/60 (76%) | ||||
| Jayam et al | 51 | 2 | 28 (55%) | 53 ± 16 | 37 (72.5%) | HTN (35%) | 8.5 ± 6.5 | 59 ± 6 | 24/51 (47%) |
| 11 (22%) | CAD (11%) | ||||||||
| 12 (33%) | |||||||||
| Efremidis et al | 13 | 9 | NA | 55 ± 23 | 11 (84.6%) | CAD (23%) | 3.2 ± 2.4 | 35 ± 5 | 8/13 (62%) |
| 10 (76.9%) | HTN (53%) | ||||||||
| 2 (23.1%) | DM (62%) |
| Study | LEAF a /LAAEF b Before Ablation | LEAF a /LAAEF b at Follow-Up | LAVmax Before Ablation | LAVmax at Follow-Up | LAVmin Before Ablation | LAVmin at Follow-Up | LAD Before Ablation | LAD After Ablation |
|---|---|---|---|---|---|---|---|---|
| Reant et al | 31 ± 13 b, ⁎ | 34 ± 11 b, ⁎ | NA | NA | NA | NA | NA | NA |
| 5.5 ± 4 b, † | 22 ± 11 b, † | |||||||
| Wylie et al | 31 ± 10 b | 27 ± 8 b | 120 ± 32 | 102 ± 25 | 62 ± 23 | 58 ± 19 | NA | NA |
| Delgado et al | 49 ± 16 a | 46 ± 13 a | 55 ± 16 | 48 ± 16 | 28 ± 13 | 26 ± 11 | NA | NA |
| 25 ± 20 b | 28 ± 18 b | |||||||
| Lemola et al | 32 ± 13 ⁎ | 21 ± 8 ⁎ | 121 ± 40 ∥ | 95 ± 30 ∥ | 87 ± 39 ∥ | 78 ± 27 ∥ | NA | NA |
| Verma et al | 17 ± 6 a | 22 ± 5 a | 94 ± 28 | 86 ± 18 | 78 ± 24 | 67 ± 14 | NA | NA |
| 17 ± 10 § | 19 ± 9 § | |||||||
| Perea et al | 40 ± 111 (NR) | 38 ± 101 (NR) | 98 ± 20 (NR) | 85 ± 17 (NR) | 58 ± 16 (NR) | 52 ± 12 (NR) | NA | NA |
| 37 ± 101 (R) | 27 ± 101 (R) | 126 ± 33 (R) | 103 ± 28 (R) | 78 ± 22 (R) | 76 ± 24 (R) | |||
| Beukema et al | NA | NA | NA | NA | NA | NA | 40 ± 4 (NR) ⁎ | 37 ± 3 |
| 44 ± 6 (NR) ‡ | 40 ± 4 | |||||||
| 45 ± 6 (R) ‡ | 49 ± 5 | |||||||
| Choi et al | 32 ± 12 | 31 ± 10 | 63 ± 20 | 50 ± 16 | 44 ± 18 | 35 ± 13 | NA | NA |
| Lemola et al | NA | NA | 115 ± 39 (NR) | 97 ± 35 (NR) | NA | NA | NA | NA |
| 128 ± 80 (R) | 135 ± 70 (R) | |||||||
| Tsao et al | NA | NA | 61 ± 19 (NR) | 56 ± 17 (NR) | NA | NA | 64 ± 8 (NR) | 61 ± 9 (NR) |
| 61 ± 17 (R) | 78 ± 25 (R) | 63 ± 8 (R) | 68 ± 11 (R) | |||||
| Tops et al | NA | NA | 59 ± 12 (NR) | 50 ± 11 (NR) | 37 ± 9 (NR) | 31 ± 7 (NR) | 45 ± 3 (NR) | 42 ± 2 (NR) |
| 63 ± 7 (R) | 68 ± 8 (R) | 43 ± 7 (R) | 47 ± 7 (R) | 45 ± 3 (R) | 48 ± 3 (R) | |||
| Rodrigues et al | 47 ± 81 | 43 ± 81 | 55 ± 18 (both) | 57 ± 19 (both) | 30 ± 15 | 34 ± 15 | 41 ± 7 | 40 ± 6 |
| 56 ± 21 (NR) | 58 ± 20 (NR) | |||||||
| 53 ± 14 (R) | 57 ± 20 (R) | |||||||
| Muller et al | NA | NA | 59 ± 12 (NR) | 50 ± 11 (NR) | 37 ± 9 (NR) | 31 ± 7 (NR) | 45 ± 3 (NR) | 42 ± 2 (NR) |
| 63 ± 7 (R) | 68 ± 8 (R) | 43 ± 7 (R) | 47 ± 7 (R) | 45 ± 3 (R) | 8 ± 3 (R) | |||
| Marsan et al | 52 ± 10 (NR) | 58 ± 10 (NR) | 26 ± 8 (NR) | 23 ± 7 (NR) | 13 ± 5 (NR) | 10 ± 4 (NR) | NA | NA |
| 47 ± 13 (R) | 42 ± 11 (R) | 31 ± 8 (R) | 32 ± 8 (R) | 16 ± 7 (R) | 18 ± 6 (R) | |||
| Liu et al | ||||||||
| CPVA | NA | NA | NA | NA | NA | NA | 33 ± 3 (NR) | 32 ± 2 (NR) |
| 35 ± 3 (R) | 34 ± 2 (R) | |||||||
| SPVI | NA | NA | NA | NA | NA | NA | 35 ± 3 (NR) | 35 ± 2 (NR) |
| 35 ± 2 (R) | 38 ± 3 (R) | |||||||
| Jayam et al | NA | NA | 102 ± 42 | 84 ± 30 | NA | NA | 36 ± 6 | 34 ± 8 |
| Efremidis et al | NA | NA | NA | NA | NA | NA | 49 ± 5 (NR) | 44 ± 4 (NR) |
| 49 ± 10 (R) | 48 ± 9 (R) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


