This meta-analysis was undertaken to assess the efficacy and safety of coronary artery bypass grafting (CABG) compared to drug-eluting stenting (DES) in patients with diabetes mellitus and multivessel coronary artery disease (CAD). CABG has been the preferred revascularization strategy in patients with diabetes compared to DES. Drug-eluting stents reduce the rate of target vessel revascularization compared to bare-metal stents. The ideal revascularization strategy for patients with diabetes with multivessel CAD in the DES era is unknown. A search of published reports was performed to identify clinical studies comparing CABG with DES in patients with diabetes with multivessel CAD with a minimum follow-up of 1 year. Five studies including 1,543 patients with diabetes (757 who underwent CABG and 786 who underwent DES) met the selection criteria. The mean follow-up period was 18 months (range 12 to 36). Compared to DES, CABG was associated with a lower risk for major adverse cardiac events (odds ratio [OR] 0.48, 95% confidence interval [CI] 0.36 to 0.65), driven mainly by a lower risk for repeat revascularization (OR 0.18, 95% CI 0.11 to 0.30), despite having a higher percentage of triple-vessel disease. There was no significant difference in death (OR 0.85, 95% CI 0.52 to 1.39) or myocardial infarction (OR 0.82, 95% CI 0.41 to 1.61). Patients in the CABG group had a higher risk for cerebrovascular events (OR 2.15, 95% CI 0.99 to 4.68). In conclusion, PCI with DES is safe and may represent a viable alternative to CABG for selected patients with diabetes with multivessel CAD.
Patients with diabetes are at increased risk for cardiovascular disease and also account for 1/4 of all patients who undergo coronary revascularization. Diabetes mellitus is associated with accelerated coronary artery disease (CAD) to account for a higher rate of myocardial infarction and cardiovascular mortality. Furthermore, patients with diabetes after revascularization procedures have increased mortality and morbidity. Clinical trials have reported lower mortality rates as well as lower rates of repeat revascularization in patients with diabetes treated with coronary artery bypass grafting (CABG) compared to percutaneous revascularization. However these studies preceded drug-eluting stenting (DES), which has been shown to decrease in-stent restenosis and repeat revascularization compared to bare-metal stenting in patients with diabetes. In the Synergy Between PCI With Taxus and Cardiac Surgery (SYNTAX) trial, patients with 3-vessel disease or left main CAD treated with CABG had lower rates of repeat revascularization but higher rates of stroke compared to those treated with paclitaxel-eluting stents (Taxus; Boston Scientific Corporation, Minneapolis, Minnesota). Therefore, we performed a meta-analysis to compare CABG to DES in patients with diabetes with multivessel disease.
Methods
We conducted a search of Medline, EMBASE, metaRegister of Controlled Trials, and Cochrane databases for clinical studies from January 2003 to July 2009 using the Medical Subject Heading terms “coronary artery bypass graft surgery,” “drug-eluting stent,” “sirolimus-eluting stent,” “paclitaxel-eluting stent,” “diabetes mellitus,” and “multivessel disease.” We used the Science Citation Index to cross-reference for studies that met our criteria.
We selected studies on the basis of predetermined criteria: clinical trials that (1) were published in peer-reviewed journals with full available text in English, (2) compared the use of percutaneous coronary intervention (PCI) to that of CABG in patients with multivessel CAD (≥2 arteries), (3) included only patients with diabetes in the study, (4) had lengths of follow-up ≥12 months, and (5) used DES in the PCI arm. Studies using bare-metal stenting were excluded in this study because DES has become the “gold standard” and to be more consistent among studies. Studies that did not include baseline patient demographics were excluded as well.
The end points of this meta-analysis were (1) major adverse cardiac events (death, myocardial infarction, and repeat revascularization); (2) death; (3) myocardial infarction; (4) repeat revascularization, defined as target vessel revascularization or any urgent revascularization on the basis of clinical condition, including surgical or percutaneous intervention; and (5) cerebrovascular events.
Prespecified data elements for each study were captured, including baseline characteristics and clinic outcomes. Two independent reviewers (MSL, TY) performed data extraction from text, tables, and figures, and a consensus was obtained for all data. Discrepancies were resolved through discussion.
The meta-analysis was completed using Comprehensive Meta-Analysis version 2 (Biostat, Englewood, New Jersey). A fixed-effects model of meta-analysis was used to aggregate the study-level data. Forest plots were generated for graphical presentations, and Q statistics were computed to assess heterogeneity across the different studies. All p values were 2 tailed, with statistical significance at 0.05, and confidence intervals (CIs) were calculated at 95%. Baseline characteristics were analyzed using weighted means and standard deviations for continuous variables and weighted proportions for binary variables. Odds ratios (ORs) and 95% CIs were calculated comparing outcomes between CABG and PCI for each of the predetermined end points. Microsoft Excel (Microsoft Corporation, Redmond, Washington) was used as ancillary software to calculate p values comparing the 2 groups’ baseline covariates using 2-sample Student’s t tests for continuous data and chi-square tests for categorical data.
Results
Five studies met our criteria for inclusion in the meta-analysis ( Table 1 ). A total of 1,543 patients were included in the analysis (757 who underwent CABG and 786 who underwent DES). Four of the studies were observational studies and 1 was a nonrandomized trial (Arterial Revascularization Therapies Study–Part II [ARTS II]) in which DES patients were selected in an attempt to match already known outcomes from the CABG cohort from ARTS I. The mean follow-up period was 18 months (range 12 to 36 months). The CABG group had higher percentages of men, triple-vessel disease, number of vessels treated, and histories of myocardial infarction, while the DES group had higher percentages of patients with hypertension and presentation with myocardial infarction.
| Study | No. of Patients | Follow-Up (months) | Age (years) | Male (%) | Smokers (%) | Hypertension (%) | Hyperlipidemia (%) | Previous MI (%) | 2-Vessel Disease (%) | 3-Vessel Disease (%) | EF | Stable Angina | UA | MI | No. of Vessels Treated | Inclusion/Exclusion Criteria |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tarantini et al | 127/93 | 24/24 | 67/65 | 81/82 | 40/37 | 87/90 | 64/47 | 60/43 | 17/55 | 84/45 | 75/73 | 60/42 | 20/33 | NR/NR | 2.4/1.5 | Excluded patients with ST elevation MIs, EFs <35%, cardiogenic shock, or valvular disease |
| Briguori et al | 149/69 | 12/12 | 66/63 | 72/70 | 40/31 | 80/74 | 66/55 | 37/42 | 14/51 | 87/50 | 53/54 | 82/80 | 10/9 | NR/NR | 2.7/1.6 | Included patients with proximal LAD lesions; excluded patients with previous revascularization and ESRD |
| Lee et al | 103/102 | 12/12 | 68/67 | 65/66 | 15/16 | 90/89 | 74/74 | 17/23 | NR/89 | NR/11 | 52/51 | 48/42 | 36/41 | 17/17 | 3.0/2.1 | Included patients with MIs, LV dysfunction, and renal or hepatic disease |
| Qiao et al | 282/363 | 12/12 | 62/61 | 78/69 | 29/32 | 61/74 | 26/30 | 25/21 | 18.1/2051 | 82/49 | 59/60 | 19/18 | 72/60 | 9/22 | 2.6/1.9 | Excluded patients with concomitant valve surgery |
| ARTS II | 96/159 | 36/36 | 63/65 | 69/67 | 17/12 | 56/80 | 49/74 | 49/30 | 64/49 | 35/50 | 60/60 | 63/54 | 33/32 | 4/15 | NR/NR | Excluded patients with previous revascularization, EFs <30%, and overt congestive heart failure |
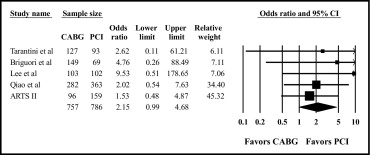
The OR and summary plot for major adverse cardiac events show that the overall analysis revealed a 52% significant reduction in patients who underwent CABG (OR 0.48, 95% CI 0.36 to 0.65; Figure 1 ). The chi-square test with 4 degrees of freedom for the Q statistic was 2.22 (p = 0.69), indicating no significant heterogeneity among the studies. Therefore, the overall analysis from the fixed-effects model was robust.
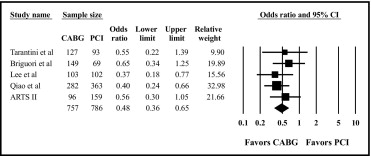
There was no significant difference in mortality between the 2 revascularization strategies (OR 0.85, 95% CI 0.52 to 1.39; Figure 2 ). The chi-square test with 4 degrees of freedom for the Q statistic was 0.67 (p = 0.95), indicating no significant heterogeneity among the studies.
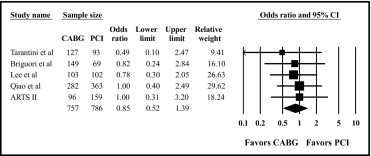
There was no significant difference in myocardial infarction between the 2 revascularization strategies (OR 0.82, 95% CI 0.41 to 1.61; Figure 3 ). The chi-square test with 3 degrees of freedom for the Q statistic was 4.25 (p = 0.24), indicating no significant heterogeneity among the studies.

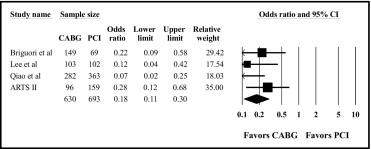
There was a significantly lower risk for repeat revascularization by 82% in patients treated with CABG compared with DES (OR 0.18, 95% CI 0.11 to 0.30; Figure 4 ). The chi-square test with 3 degrees of freedom for the Q statistic was 3.65 (p = 0.30), indicating no significant heterogeneity among the studies.
There was a higher risk for cerebrovascular events in patients treated with CABG compared to DES (OR 2.15, 95% CI 0.99 to 4.68; Figure 5 ). The chi-square test with 4 degrees of freedom for the Q statistic was 1.63 (p = 0.80), indicating no significant heterogeneity among the studies.