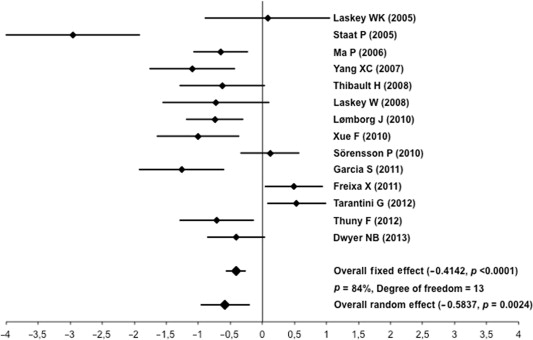
Clinical benefit of postconditioning in patients with ST-elevation myocardial infarction (STEMI) treated by primary percutaneous coronary intervention is still controversial. We performed a meta-analysis of available randomized clinical trials (RCTs) to define the role of postconditioning in STEMI. Fourteen RCTs evaluating postconditioning in a total of 778 patients with STEMI were identified in PubMed, EMBase, and Cochrane databases from January 1998 to February 2014. Overall, postconditioning was found to be cardioprotective in term of infarct size reduction (weighted standardized mean differences −0.5837, 95% confidence interval −0.9609 to −0.2066, p <0.05), but significant heterogeneity across the trials was detected (I 2 = 84%). Univariate meta-regression analysis did not identify clinical or procedural variables associated with a more pronounced effect of postconditioning effects on infarct size with the exception of using cardiac magnetic resonance (CMR) to evaluate infarct size (p <0.01). Restricting the analysis to 6 RCTs including a total of 448 patients and evaluating the postconditioning effect on infarct size by means of CMR led to the disappearance of benefit of postconditioning on infarct size. In conclusion, the results of this meta-analysis of RCTs suggested that postconditioning reduces infarct size, as expressed by weighted standardized mean differences. However, if the analysis was limited to trials with a more accurate quantification of infarct size reduction, namely by CMR, the benefit was lost. More data are required before adoption of postconditioning in clinical practice.
In 2003, Zhao et al first introduced the concept of ischemic postconditioning, showing that brief cycles of balloon-catheter occlusion after left anterior descending coronary artery reperfusion reduced infarct size by 44% compared with controls in the acute myocardial infarction canine model. Early observational experience of Laskey and Staat et al confirmed in humans the cardioprotective effect of postconditioning in terms of improved myocardial perfusion and infarct size reduction after primary percutaneous coronary interventions (PCIs). However, recent randomized clinical trials (RCTs) have brought controversial results and raised concerns about the safety of this maneuver. Moreover, the effects of postconditioning on infarct size using cardiac magnetic resonance (CMR) have not been fully evaluated in a meta-analysis. Accordingly, we conducted a meta-analysis of the available RCTs to better define the impact of postconditioning in patients with ST-elevation myocardial infarction (STEMI) treated by primary PCIs.
Methods
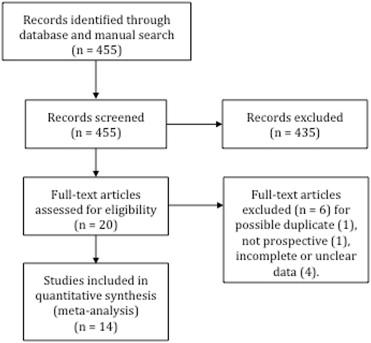
We searched PubMed, EMBase, and the Cochrane Central Register of Controlled Trials database for all published studies up to February 28, 2014, that evaluated postconditioning versus standard of care in patients with STEMI who underwent primary PCI. The following keywords were used: “ischemic postconditioning,” “postconditioning,” “angioplasty,” “myocardial infarction,” and “myocardial injury.” A manual search was also conducted, and reference lists of the retrieved articles were screened as well. Inclusion criteria were (1) prospective RCTs published in English, (2) primary PCI as the intervention, and (3) studies clearly reporting a measurement of infarct size in terms of cardiac biomarkers, single-photon emission computed tomography (SPECT) or CMR. Exclusion criteria were (1) studies not reporting clear and complete data on infarct size and (2) nonrandomized studies. Studies were selected and assessed for quality (according to the Jadad scoring method) by 2 investigators (EF and GT); a third investigator (ACF) independently assessed the studies in case of disagreement. Demographic data, baseline variables, number of patients in each intervention group, and infarct size measurements were extracted from each study. Following parameters were considered for infarct size assessment: creatine kinase (CK) peak or area under the curve (AUC); troponin I or T, peak or AUC; and percentage of left ventricle volume infarcted at SPECT or at CMR. When more than 1 method of assessment of infarct size were used, the more robust one was considered for the analysis (i.e., CMR > SPECT > CK or troponin AUC > CK or troponin peak).
For continuous variables (reported as mean and SD or median and interquartile range [IQR]), we calculated weighted standardized mean differences (WSMD) to obtain the pooled estimates with 95% confidence interval (CI) both with fixed and DerSimonian and Laird random effect model. The statistical significance was set at 5% level. In 1 study, median and IQR were reported instead of mean and SD; because the median was about in the middle of the IQR, we judged that the distribution was symmetric and we used the median value as mean value and SD was estimated considering that in the normal distribution width of the IQR is approximately 1.35 SD. In 1 study, peak of CK myocardial band instead of AUC of CK was used because this latter value was not consistent with the reported 95% CI. In 2 studies, we considered for the meta-analysis the opposite of the value of myocardial salvage index, expressed as percentage of area at risk, to maintain the sign of the effect concordant with that of the other studies. Heterogeneity was assessed using the Cochran Q and I 2 statistics. For the Q statistic, a p value of 0.10 was considered statistically significant for heterogeneity; for the I 2 statistic, heterogeneity was interpreted as absent (0% to 25%), low (25.1% to 50%), moderate (50.1% to 75%), or high (75.1% to 100%). Meta-regression and subgroup analysis were conducted to explore the potential sources of significant heterogeneity and a p value <0.1 was accepted as indicating statistical significance. For subgroup analysis, interaction between the intervention factor and the grouping factor was investigated with the method proposed by Altman and Bland, and a p <0.1 was considered as indicating interaction. Sensitivity analysis were used to assess the robustness of our results by removing each included study at 1 time to obtain and evaluate the remaining overall estimates of infarct size. Publications bias was assessed with funnel plot and Egger’s test followed in case of a p value <0.05 by the trim and fill method to estimate the number of null missing studies from the meta-analysis. All statistical analyses were conducted with “Metafor” package in R 3.0.2 on Windows environment.
Results
The search produced 455 hits. After exclusion by title or by abstract of all nonrelevant articles, a total of 20 potentially relevant studies of postconditioning in patients with STEMI who underwent primary PCI were selected for further evaluation. Out of them, 6 studies were excluded because of the following reasons: 1 was a duplicate, 1 was a retrospective study, and 4 lacked of clear and complete data on infarct size. Fourteen studies finally met the inclusion/exclusion criteria, for a total of 778 patients ( Figure 1 ). The main characteristics of the analyzed studies are listed in Table 1 . Seven studies enrolled patients with symptom-onset duration ≤6 hours at the time of presentation, whereas the remaining studies considered eligible patients with chest pain duration up to 12 hours. Five studies did not exclude patients with collaterals that was, indeed, an exclusion criterion in the others. The adopted postconditioning protocol (duration of ischemia/reperfusion interval × number of cycles) was 60 s/60 s × 4 in 7, 30 s/30 s × 4 in 3, 30 s/30 s × 2 in 2, and 90 s/180 s × 2 in 2. Eight of 14 studies had Jadad score of 2, whereas for the remaining the score was 3. In Table 2 are reported the infarct size assessment methods of each RCTs and the one adopted in the present meta-analysis. As surrogates of infarct size, myocardial biomarkers were used in 5 studies (CK peak value in 2 studies, AUC of CK in 1 study, and peak CK-myocardial band in 2 studies ), SPECT in 3 studies, and finally, delayed-enhancement CMR in 6 studies. The main clinical and procedural study characteristics are reported in Tables 1 and 3 . The direct stenting technique was used exclusively in 4 studies, partly in 2, and not used in the remaining 8. Out of 14 studies, glycoprotein IIb/IIIa (GP IIb/IIIa) inhibitors were used in 6 RCTs. Nevertheless, only one of them prespecified its use in the study protocol.
| Study (1st Author, Publication Year) | Nb. of Pts PC/C | Symptom Onset, hours | TIMI Grade | Collaterals to IRA | Ischemia Time, min PC/C | PC (Cycles × I/R) | Jadad Score |
|---|---|---|---|---|---|---|---|
| Laskey WK, 2005 | 10/7 | ≤12 | 0 | No | 341/286 | 2 × 90 s/180 s | 2 |
| Staat P, 2005 | 16/14 | ≤6 | 0 | No | 318/331 | 4 × 60 s/60 s | 2 |
| Ma X, 2006 | 47/47 | ≤12 | 0–1 (>89%) | Yes | 395/426 | 3 × 30 s/30 s | 3 |
| Yang XC, 2007 | 23/18 | ≤12 | 0 | No | 312/264 | 3 × 30 s/30 s | 2 |
| Thibault H, 2008 | 17/21 | ≤6 | 0 | No | 283/297 | 4 × 60 s/60 s | 2 |
| Laskey WK, 2008 | 12/12 | ≤6 | 0–1 | No | 228/222 | 2 × 90 s/180 s | 2 |
| Lømborg J, 2010 | 43/43 | ≤6 | 0–1 | Yes | 241/255 | 4 × 30 s/30 s | 3 |
| Xue F, 2010 | 23/20 | ≤12 | 0 | Yes | 246/324 | 4 × 60 s/60 s | 2 |
| Sörensson P, 2010 | 38/38 | ≤6 | 0 | Yes | 165/185 | 4 × 60 s/60 s | 2 |
| Garcia S, 2011 | 22/21 | ≤12 | 0 | No | 270/264 | 4 × 30 s/30 s | 2 |
| Freixa X, 2012 | 39/40 | ≤12 | 0–1 | No | 326/330 | 4 × 60 s/60 s | 3 |
| Tarantini G, 2012 | 39/39 | ≤6 | 0–1 | No | 212/194 | 4 × 60 s/60 s | 3 |
| Thuny F, 2012 | 25/25 | ≤12 | 0–1 | No | 289/215 | 4 × 60 s/60 s | 3 |
| Dwyer NB, 2013 | 39/40 | ≤6 | 0–1 | Yes | 151/167 | 4 × 30 s/30 s | 3 |
| Study (1st Author, Publication Year) | Peak CK | AUC CK | Peak CK-MB | AUC CK-MB | Peak Tn I | AUC Tn I | SPECT | DE-CMR |
|---|---|---|---|---|---|---|---|---|
| Laskey WK, 2005 | X | |||||||
| Staat P, 2005 | X | X | ||||||
| Ma X, 2006 | X | X | ||||||
| Yang XC, 2007 | X | X | ||||||
| Thibault H, 2008 | X | X | X | |||||
| Laskey WK, 2008 | X | |||||||
| Lønborg J, 2010 | X ∗ | X | ||||||
| Xue F, 2010 | X | X | X | |||||
| Sörensson P, 2010 | X | X ∗ | X | |||||
| Garcia S, 2011 | X | X | X | |||||
| Freixa X, 2012 | X | X | X | X | ||||
| Tarantini G, 2012 | X | X | X | |||||
| Thuny F, 2012 | X | X | ||||||
| Dwyer NB, 2013 | X | X | X |
∗ In this study, troponin T instead of troponin I was measured.
| Study (1st Author, Publ. Year) | Age, years PC/C | Male, % PC/C | Diabetes, % PC/C | Dyslipidemia, % PC/C | Baseline LVEF, % PC/C | Direct Stent Technique, % PC/C | GP IIb/IIIa Rec Inh, % PC/C |
|---|---|---|---|---|---|---|---|
| Laskey WK, 2005 | 58/58 | 50/71 | NA | NA | NA | 0/0 | NA |
| Staat P, 2005 | 58/56 | 75/93 | 20/13 | 80/50 | 52/49 | 100/100 | NA |
| Ma X, 2006 | 64/64 | 66/70 | 38/45 | NA | NA | 0/0 | NA |
| Yang XC, 2007 | 59/63 | 87/61 | 26/28 | 61/56 | NA | 0/0 | 0/0 |
| Thibault H, 2008 | 56/56 | 76/78 | 12/10 | 52/49 | 44/46 | 100/100 | NA |
| Laskey WK, 2008 | 60/58 | 58/58 | 42/42 | 46/75 | NA (≥40) | 0/0 | 58/67 |
| Lønborg J, 2010 | 61/62 | 69/74 | 7/7 | 46/41 | NA | 0/0 | 49/49 |
| Xue F, 2010 | 54/62 | 95/94 | 21/29 | 16/24 | NA | 0/0 | NA |
| Sörensson P, 2010 | 63/62 | 82/89 | 71/68 | 77/62 | NA | 0/5 | 79/79 |
| Garcia S, 2011 | 61/55 | 86/76 | 5/19 | 73/71 | NA | 0/0 | NA |
| Freixa X, 2012 | 59/60 | 84/72 | 23/17 | 44/35 | NA | 61/55 | NA |
| Tarantini G, 2012 | 60/60 | 85/85 | 18/3 | 51/49 | 59/59 | 100/100 | 100/100 |
| Thuny F, 2012 | 57/57 | 72/76 | 20/14 | 36/48 | 52/50 | 100/100 | 76/72 |
| Dwyer NB, 2013 | 56/57 | 90/93 | 10/3 | 36/28 | 56/52 | 0/0 | 90/85 |
Considered collectively, the 14 RCTs investigating postconditioning had a cardioprotective effect in term of infarct size reduction (WSMD −0.5837, 95% CI −0.9609 to −0.2066, p <0.05), with significant heterogeneity (I 2 = 84%, p <0.0001), as shown in Figure 2 and Table 4 . Sensitivity analysis showed qualitative and quantitative consistency of the main result (all p <0.05) ( Figure 3 ). Evidence of significant publication bias was observed (Egger’s test Z = −2.6322, p = 0.0085), but no additional studies with null effect were identified, probably for the high heterogeneity of the analyzed RCTs. At the random-effect univariable meta-regression analysis, most of the investigated variables (age, men [%], diabetes [%], dyslipidemia [%], country [Asia vs non-Asia], maximum symptom onset duration [≤6 hours = 0; ≤12 hours = 1], Thrombolysis in Myocardial Infarction flow grade and collaterals to area at risk at presentation, direct stenting technique, GP IIb/IIIa inhibitors use, mean ischemic time, and postconditioning ischemia duration [≥60 seconds; <60 seconds]) were not significant source of heterogeneity (all p ≥0.1), with the exception of the use of CMR to evaluate infarct size (intercept = −0.9858, p <0.0001; slope = 0.8729, p = 0.0074). A subgroup analysis, by analysis restriction to those RCTs using CMR to investigate infarct size (6 studies for a total of 448 patients enrolled) showed that postconditioning had no impact on infarct size (CMR WSMD −0.1129, 95% CI −0.575 to 0.3492, p = 0.6319, and no CMR WSMD −0.9853, 95% CI −1.426 to −0.5466, p <0.0001) ( Figure 4 ).