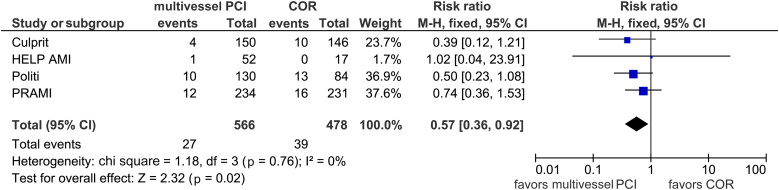
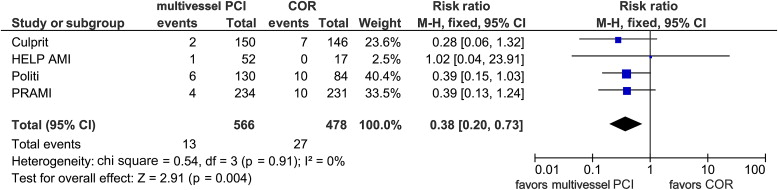
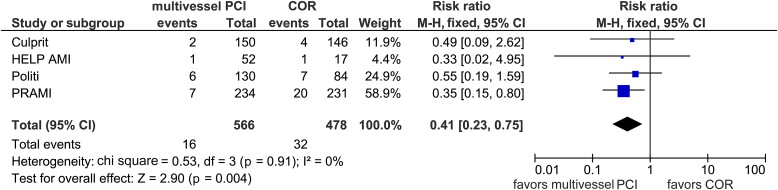
Current guidelines recommend against revascularization of the noninfarct artery during the index percutaneous coronary intervention (PCI) in hemodynamically stable patients with ST-segment elevation myocardial infarction (STEMI). This was based largely on observational studies with few data coming from randomized controlled trials (RCTs). Recently, several small-to-moderate sized RCTs have provided data, suggesting that a multivessel revascularization approach may be appropriate. We performed a meta-analysis of RCTs comparing multivessel percutaneous coronary intervention (MV PCI) versus culprit vessel–only revascularization (COR) during primary PCI in patients with STEMI and multivessel coronary disease (MVCD). We searched Medline, PubMed, and Scopus databases for RCTs comparing MV PCI versus COR in patients with STEMI and MVCD. The incidence of all-cause death, cardiac death, recurrent myocardial infarction, and revascularization during follow-up were extracted. Four RCTs fit our primary selection criteria. Among these, 566 patients underwent MV PCI (either at the time of the primary PCI or as a staged procedure) and 478 patients underwent COR. During long-term follow-up (range 1 to 2.5 years), combined data indicated a significant reduction in all-cause mortality (relative risk [RR] 0.57, 95% confidence interval [CI] 0.36 to 0.92, p = 0.02) and in cardiac death (RR 0.38, 95% CI 0.20 to 0.73, p = 0.004) with MV PCI. In addition, there was a significantly lower risk of recurrent myocardial infarction (RR 0.41, 95% CI 0.23 to 0.75; p = 0.004) and future revascularization (RR 0.37, 95% CI 0.27 to 0.52; p <0.00001). In conclusion, from the RCT data, MV PCI appears to improve outcomes in patients with STEMI and MVCD.
Multivessel coronary disease (MVCD) is commonly encountered in patients with ST-segment elevation myocardial infarction (STEMI) who underwent primary percutaneous coronary intervention (P-PCI), occurring in 40% to 60% of patients, and is associated with a worse prognosis compared with those patients with culprit-vessel disease only. The optimal management of patients with MVCD remains unresolved. Current American College of Cardiology/American Heart Association guidelines recommend against multivessel percutaneous coronary intervention (MV PCI) at the time of P-PCI. This is largely based on data from observational studies demonstrating a higher event rate for patients who underwent MV PCI at the time of P-PCI. Until recently, there were few randomized controlled trials (RCTs) examining outcomes of treating MVCD in STEMI. Since the publication of the most recent STEMI guidelines, 2 moderate-sized RCTs have reported favorable results after MV PCI. In view of the conflicting reports from randomized and observational studies, we performed a meta-analysis of RCTs only comparing the different strategies for the management of MVCD in STEMI.
Methods
Two authors (GE and JTH) independently and in duplicate searched Pubmed and Scopus databases until the end of December 2014 to identify prospective RCTs that compared MV PCI with culprit-only PCI (culprit vessel–only revascularization [COR]) in patients with STEMI. We also reviewed previous reports and the references of the selected studies. Finally, we searched conference proceedings of all major national and international cardiology conferences. We used the following key words: “multivessel,” “culprit,” “non-infarct-related artery” (non-IRA) “staged,” “revascularization,” “PCI,” “STEMI,” and “myocardial infarction” (MI). We included RCTs examining patients with STEMI and MVCD who underwent P-PCI that reported cardiovascular outcomes. We excluded prospective nonrandomized trials. We also excluded trials enrolling patients with cardiogenic shock or patients who underwent PCI for reasons other than P-PCI. We excluded trials that did not compare a strategy of MV PCI with COR. Disagreements were resolved by consensus.
For each of the selected studies, we identified the treatment strategy for each group. We defined MV PCI as either a single-setting PCI strategy in which lesions in the culprit vessel and the non-IRA were treated during the same procedure or a multisetting procedure with staged PCI of the non-IRA. COR was defined as intended PCI confined to the culprit vessel only. We examined the following clinical outcomes: all-cause mortality, cardiac mortality, recurrent myocardial infarction (re-MI), and repeat revascularization (PCI or coronary artery bypass graft). We also examined the incidence of major bleeding, contrast-induced nephropathy (CIN), and stroke. These outcomes were defined according to the definition used in each trial.
The statistical analysis was done in line with recommendations from the Cochrane Collaboration and the Preferred Reporting Items for Systematic reviews and Meta-analyses guidelines using Review Manager (RevMan), version 5.1.7 (Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark). Heterogeneity was assessed using the I 2 statistic, defined as the proportion of total variation observed between the trials attributable to differences in trials rather than sampling error (chance) with values <25% considered as low and >75% as high. Analysis was performed on an intention-to-treat basis. We performed fixed-effect analysis when I 2 was up to 25% and p at least 0.05, otherwise we used random-effect analysis. Publication bias was estimated visually by funnel plots and/or using Begg’s test and the weighted regression test of Egger.
Results
Our initial search strategy retrieved 582 articles. Among these, 7 fit our primary selection criteria. We excluded 3 of these trials: Two trials compared MV PCI at the time of P-PCI with staged PCI. Another trial performed FFR of the non-IRA to guide the decision for PCI. Four RCTs fit our final selection criteria and were included ( Supplementary Figure 1 ).
Table 1 lists the characteristics of the included studies. A total of 1,044 patients were included, of which 478 underwent COR and 566 were assigned to MV PCI. Exclusion criteria are depicted in Table 1 . Additional exclusion criteria included the following: recent (<1 week) use of fibrinolytic therapy, intention to treat >1 chronic total occlusion, severe tortuosity or calcification of the non-IRA, lesion in a graft or a vessel having received previous PCI, or significant side-branch disease ; unsuccessful P-PCI or significant valve disease ; and age <18 years, ventricular septal defect, mitral regurgitation, stage 4 or 5 chronic kidney disease, stent thrombosis, or previous Q-wave infarction. In 2 studies, MV PCI was performed at the time of the index procedure. In the study by Politi et al, 65 patients underwent PCI of the non-IRA at the time of P-PCI and 65 patients underwent MV PCI as a staged procedure 56.8 ± 12.9 days after the P-PCI. In the Multivessel Versus Lesion-Only Primary PCI Trial (CvLPRIT), 97 patients underwent MV PCI at the time of P-PCI and 42 patients underwent staged in hospital MV PCI. Table 2 depicts the baseline variables for the enrolled patients.
| Study | Year | Duration of F/U (Months) | COR (N) | Multi-vessel PCI (N) | Exclusion Criteria | ||||
|---|---|---|---|---|---|---|---|---|---|
| CS | LM | CTO | CAB | Other | |||||
| Help-AMI | 2004 | 12 | 17 | 52 | + | + | – | – | + |
| Politi et al | 2009 | 30 | 84 | 130 | + | + | – | + | + |
| PRAMI | 2013 | 23 | 231 | 234 | + | + | + | + | – |
| CvLPRIT | 2014 | 12 | 146 | 150 | + | – | + | + | + |
| Variable | Total (n=1044) | COR (n=478) | Multi-vessel PCI (=566) |
|---|---|---|---|
| Men | 829(79.4%) | 376(78.7%) | 453(80.0%) |
| Hypertension | 445(42.6%) | 204(42.7%) | 241(42.6%) |
| Diabetes Mellitus | 176(16.9%) | 95(19.9%) | 81(14.3%) |
| Smoker | 357(43.0%) | 154(39.1%) | 203(46.6%) |
| Anterior wall infarction | 393(37.6%) | 186(38.9%) | 207(36.6%) |
| Triple vessel disease | 327(31.3%) | 141(29.5%) | 186(32.3%) |
| Glycoprotein IIB/IIIA inhibitor use | 711(68.1%) | 318(66.5%) | 393(69.4%) |
During long-term follow-up, there were 27 deaths (4.8%) in the MV PCI group and 39 deaths (8.2%) in the COR. As shown in Figure 1 , we observed a significant decrease in all-cause mortality with MV PCI (relative risk [RR] 0.57, 95% confidence interval [CI] 0.36 to 0.92, I 2 = 0%, p = 0.02). Similarly, MV PCI was associated with a 62% reduction in the risk of cardiac death (RR 0.38, 95% CI 0.20 to 0.73, I 2 = 0%, p = 0.004; Figure 2 ). There was a 59% decrease in the risk of re-MI with MV PCI (RR 0.41, 95% CI 0.23 to 0.75, I 2 = 0%, p = 0.004; Figure 3 ). We observed a significant decrease in the risk of future revascularization in the MV PCI group (RR 0.37, 95% CI 0.27 to 0.52, I 2 = 0%, p <0.00001; Figure 4 ). Assessment of the included studies using funnel plots and also the Cochrane collaboration’s tool for assessing risk of bias demonstrated a low risk of bias among the 4 included studies ( Supplementary Figure 2 and Supplementary Table 1 ).
Only 2 studies reported the rates of major bleeding. There was no significant difference in the relative risk for major bleeding with MV PCI compared with COR (RR 0.83, 95% CI 0.38 to 1.83, p = 0.64). The rates of CIN were reported in 3 studies. Pooled analysis showed similar rates of CIN for MV PCI compared with COR (RR 0.53, 95% CI 0.16 to 1.77, p = 0.31). Stroke was reported in 2 studies. There was no significant difference in the relative risk for stroke with MV PCI compared with COR (1.76, 95% CI 0.38 to 8.19, p = 0.47; Supplementary Figure 3 ).
Results
Our initial search strategy retrieved 582 articles. Among these, 7 fit our primary selection criteria. We excluded 3 of these trials: Two trials compared MV PCI at the time of P-PCI with staged PCI. Another trial performed FFR of the non-IRA to guide the decision for PCI. Four RCTs fit our final selection criteria and were included ( Supplementary Figure 1 ).
Table 1 lists the characteristics of the included studies. A total of 1,044 patients were included, of which 478 underwent COR and 566 were assigned to MV PCI. Exclusion criteria are depicted in Table 1 . Additional exclusion criteria included the following: recent (<1 week) use of fibrinolytic therapy, intention to treat >1 chronic total occlusion, severe tortuosity or calcification of the non-IRA, lesion in a graft or a vessel having received previous PCI, or significant side-branch disease ; unsuccessful P-PCI or significant valve disease ; and age <18 years, ventricular septal defect, mitral regurgitation, stage 4 or 5 chronic kidney disease, stent thrombosis, or previous Q-wave infarction. In 2 studies, MV PCI was performed at the time of the index procedure. In the study by Politi et al, 65 patients underwent PCI of the non-IRA at the time of P-PCI and 65 patients underwent MV PCI as a staged procedure 56.8 ± 12.9 days after the P-PCI. In the Multivessel Versus Lesion-Only Primary PCI Trial (CvLPRIT), 97 patients underwent MV PCI at the time of P-PCI and 42 patients underwent staged in hospital MV PCI. Table 2 depicts the baseline variables for the enrolled patients.



