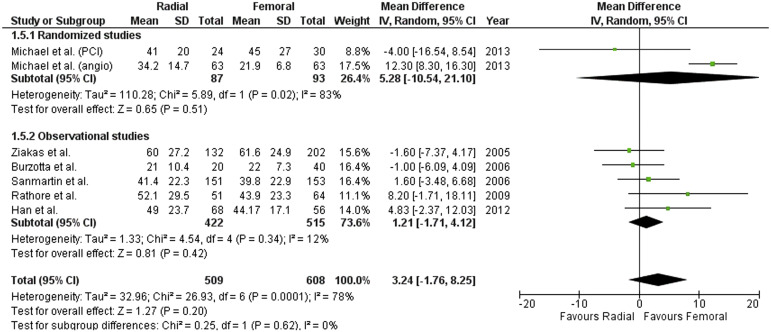
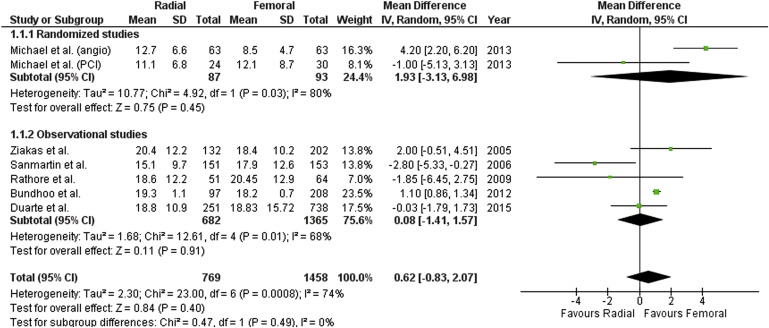
Cardiac catheterization through the radial artery approach (RA) has been shown to significantly reduce access-site complications compared with the femoral artery approach (FA) in many clinical settings. However, in the subset of patients with previous coronary artery bypass grafting (CABG), optimal vascular access site for coronary angiography and intervention is still a matter of debate. We aimed to perform a systematic review and meta-analysis of available studies comparing RA with FA in patients with previous CABG. Data were extracted by two independent reviewers; weighted mean differences and 95% confidence interval (CI) were calculated for continuous outcomes, whereas odds ratio (OR) and 95% CI were calculated for dichotomous outcomes. Summary statistics were calculated by random-effects model using Review Manager 5.3 software. The meta-analysis included 1 randomized and 8 nonrandomized studies, with a total of 2,763 patients. Compared with FA, RA required similar procedural time (mean difference 3.24 minutes, 95% CI −1.76 to 8.25, p = 0.20), fluoroscopy time (mean difference 0.62 minutes, 95% CI −0.83 to 2.07, p = 0.40), and contrast volume (mean difference −2.58 ml, 95% CI −18.36 to 13.20, p = 0.75) and was associated with similar rate of procedural failure (OR 1.32, 95% CI 0.63 to 2.80, p = 0.46), higher rate of crossover to another vascular access (OR 7.0, 95% CI 2.74 to 17.87, p <0.0001), and lower risk of access-site complications (OR 0.46, 95%CI 0.26 to 0.80, p = 0.006). In conclusion, the present meta-analysis suggests that in patients with previous CABG undergoing coronary procedures, RA, compared with FA, is associated with increased crossover rate but may reduce access-site complications.
The radial artery approach (RA) has been shown to consistently reduce access-site complications and bleeding compared with the femoral artery approach (FA) across a wide spectrum of patients undergoing percutaneous coronary procedures, such as patients with acute coronary syndromes, obesity, women, and the elderly. However, limited evidence is available in the setting of patients with previous coronary artery bypass grafting (CABG). Patients with previous CABG often have multivessel coronary artery disease and present diffuse atherosclerosis involving different vascular territories, such as the iliac and femoral arteries ; therefore, RA could be an effective strategy to reduce access-site complications in this setting. Conversely, RA can be technically more demanding and may be associated with increased radiation exposure, especially when attempting to cannulate bypass conduits. Despite several observational studies suggesting that RA can be safely and effectively performed in patients with previous CABG, RA was inferior to FA in terms of contrast volume, procedural time, and radiation exposure in the only randomized trial performed to date. The goal of the present study was to perform a systematic review and meta-analysis of available studies comparing RA with FA in patients with previous CABG undergoing coronary procedures.
Methods
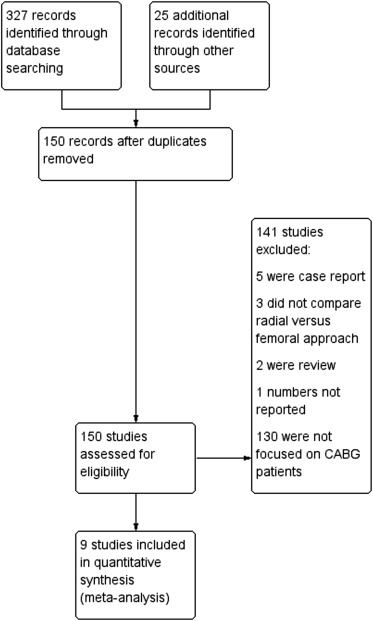
This meta-analysis was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist. Major electronic databases (PubMed, Scopus, the Cochrane Library) were searched through October 2015 using the following terms: “radial,” “vascular access,” “femoral,” “coronary artery bypass graft,” “coronary angiography,” and “percutaneous coronary interventions.” We limited our search to articles in English; the “Similar articles” section of PubMed and references from selected papers were also checked. Moreover, we searched abstracts presented at major Interventional Cardiology meetings (Transcatheter Cardiovascular Therapeutics and Euro Paris Course on Revascularization) in the last 5 years. We included both randomized and observational studies comparing RA with FA for coronary angiography (CA) and/or percutaneous coronary intervention (PCI) in patients with previous CABG, in which at least 1 of the following outcome was reported: (1) procedural time; (2) fluoroscopy time; (3) procedural failure rate; (4) contrast volume; (5) crossover rate to a different vascular access; and (6) access-site complications. Procedural failure was defined in the following way: (1) the inability to complete the diagnostic examination from the selected access route in CA procedures and (2) Thrombolysis in Myocardial Infarction (TIMI) flow <3 and/or residual stenosis >30% in PCI procedures. The 2 outcomes were analyzed separately for studies allowing both diagnostic CA and PCI procedures. Access-site complications were adjudicated according to the definitions used by each study; when not clearly defined in the Methods section, the following events were adjudicated: access-site hematoma, access-site–related bleeding, any vascular complications requiring surgery or prolonging hospital stay (e.g., pseudoaneurysm, arteriovenous fistula), retroperitoneal bleeding, arterial dissection or occlusion, and limb ischemia. Two authors (S.Rig. and A.S.) evaluated each study for inclusion and extracted outcome data in duplicate using a standardized Excel sheet. Differences were resolved by consensus. Summary statistics were calculated by the Mantel-Haenszel method. Weighted mean differences and 95% confidence interval (CI) were calculated for continuous outcomes, whereas odds ratio (OR) and 95% CI were calculated for dichotomous outcomes. The heterogeneity of the studies was analyzed using a chi-square test for which a p value <0.2 was considered potentially heterogeneous. An I 2 test of heterogeneity, which describes the percentage of total variation across studies that is due to heterogeneity, was also performed for every comparison. Heterogeneity is described as low, moderate, and high, based on I 2 values of 25%, 50%, and 75%, respectively. A 2-sided p value was considered statistically significant. We used a random effect model for all our analyses. All statistical calculations were performed using Review Manager Version 5.3 (Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014).
Results
Of the 352 records initially screened, 9 studies met the inclusion criteria ( Figure 1 , Table 1 ). Only 1 study was a randomized trial, whereas the others were nonrandomized studies. One study was only presented as an abstract but was included in the analysis. The included studies contained a total of 2,763 patients; 947 were in the RA arm, whereas 1,816 were in the FA arm. The enrollment criteria were heterogeneous across studies; 3 studies included patients with CABG undergoing CA and/or PCI, 3 studies included patients undergoing saphenous vein graft PCI, 1 study included patients with left internal mammary artery (IMA) graft undergoing CA, 1 study included patients with CABG undergoing PCI and, finally, 1 study included patients with CABG undergoing CA. Patients with bilateral IMA grafts were excluded in most studies. In most studies the operators were expert in RA; in 1 study procedures performed during the learning curve were also considered, whereas in the RADIAL-CABG (RADIAL versus Femoral Access for Coronary Artery Bypass Graft Angiography and Intervention) trial a “fellow first” strategy, in which a physician in training performed the procedure under the supervision of an expert operator, was adopted. The mean age was 66.0 years in the RA arm and 65.7 years in the FA arm; most patients were men in both groups (86.1% in RA vs 83.3% in FA); the mean number of grafts was 2.2 in both arms. Although 53.3% of patients in the FA group presented with an acute coronary syndrome compared with 45.6% in the RA group, in the latter the rate of glycoprotein IIb/IIIa blocker use during the procedure was slightly higher (28.2% vs 25.3%). In the 3 studies reporting data about the side of RA, left RA was more prevalent, ranging from 88.7% to 100%. In the 3 studies focusing on vein graft PCI the rate of ≥7Fr sheath use was significantly higher in FA than in RA; in the remaining studies this rate was either not significantly different or not reported. RA was associated with a nonsignificant increase of 3.24 minutes (95% CI −1.76 to 8.25; p = 0.2) in procedural time and of 0.62 minutes (95% CI −0.83 to 2.07; p = 0.4) in fluoroscopy time compared with FA ( Figures 2 and 3 ). The procedural failure rate was similar between RA and FA (OR 1.32, 95% CI 0.63 to 2.80; p = 0.46; Figure 4 ), and the volume of contrast given was also similar between the 2 approaches (mean difference −2.58 ml, 95% CI −18.36 to 13.20; p = 0.75; Figure 5 ). Differently, the rate of crossover to another vascular access was significantly higher in RA (32 of 676 patients; 4.7%) than in FA (3 of 1,038 patients; 0.29%), with an odds ratio of 7.0 (95% CI 2.74 to 17.87; p <0.0001; Figure 6 ). Reasons for crossover from RA included radial artery spasm (n = 4), puncture failure (n = 6), anatomic variants and/or tortuosity of the radial artery (n = 7), issues with subclavian arteries/ascending aorta (n = 5), and failed selective engagement of grafts (n = 10). RA was associated with a significantly reduced risk of access-site complications (16 of 696 patients; 2.3%) compared with FA (62 of 1,078 patients; 5.8%), with an odds ratio of 0.46 (95% CI 0.26 to 0.80; p = 0.006; Figure 7 ). A detailed description of access-site complications was reported by all studies except one Most complications were represented by local hematomas, which were more frequent and severe in FA patients than in RA patients, such as the need for transfusion ( Table 2 ). Five studies also reported data about periprocedural cerebrovascular accident; in the RA group there were no events (0.0%), whereas in the FA group there were 4 events of 515 patients (OR 0.39, 95% CI 0.08 to 1.96; p = 0.25).
| Study | RCT | Year | Group | Patients (n) | Enrollment criteria | Age (years) | Male (n,%) | BMI (kg/m2) | Sheath size ≥ 7 French (n,%) | Acute coronary syndrome (n,%) | GPI (n,%) | Heparin (IU) | Number of grafts |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ziakas et al. | 0 | 2005 | RA | 132 | Saphenous vein graft PCI | 71±8 | 116 (87.9) | – | 22 (16.6) | 78 (59.1) | 36 (27.2) | 8685±6300 | – |
| FA | 202 | 69±10 ∗ | 167 (82.7) | 71 (35.1) ∗ | 146 (72.2) | 67 (33.2) | 8288±3048 | ||||||
| Sanmartin et al. | 0 | 2006 | RA | 151 | CA in CABG patients | 68±8 | 131 (86.8) | – | 0 (0.0) | 42 (27.8) | 6 (4.0) | 5000 | 2.2±0.9 |
| FA | 153 | 68±8 | 127 (82.9) | 0 (0.0) | 55 (35.9) | 7 (4.6) | – | 2.4±0.9 ∗ | |||||
| Burzotta et al. | 0. | 2008 | RA | 20 | CA in LIMA graft recipients | 65±5 | 18 (90.0) | – | 0 (0.0) | 4 (20) | – | 5000 | 2.3±0.7 |
| FA | 40 | 65±9 | 36 (90.0) | 0 (0.0) | 12 (30) | 2500 | 2.3±0.6 | ||||||
| Rathore et al. | 0 | 2009 | RA | 51 | Saphenous vein graft PCI | 65±10 | 46 (90.1) | – | 3 (6.0) | 12 (23.5) | 40 (78.4) | – | – |
| FA | 64 | 63±11 | 56 (87.5) | 25 (40.0) ∗ | 27 (42.2) ∗ | 34 (53.1) ∗ | |||||||
| Bundhoo et al. | 0 | 2012 | RA | 97 | Saphenous vein graft PCI | 69±1 | 85 (87.6) | 29.0±0.4 | 0 (0.0) | 48 (49.5) | 33 (34.0) | 70 IU/Kg | – |
| FA | 208 | 69±1 | 175 (84.1) | 28.0±0.3 ∗ | 42 (20.0) ∗ | 138 (66.3) ∗ | 83 (39.9) | 70 IU/Kg | |||||
| Han et al. | 0 | 2012 | RA | 68 | CA/PCI in CABG patients | 65±9 | 53 (77.9) | 26±3 | – | 55 (80.9) | 14 (20.6) | – | 1.69 |
| FA | 56 | 64±8 | 43 (76.8) | 26±2 | 41 (73.2) | 10 (17.9) | 1.66 | ||||||
| Michael et al. | + | 2013 | RA | 64 | CA/PCI in CABG patients | 65±6 | 64 (100.0) | 31.9±5.5 | – | 20 (31.2) | – | – | 2.2±1.0 |
| FA | 64 | 67±6 | 64 (100.0) | 30.0±5.4 | 20 (31.2) | 2.3±0.9 | |||||||
| He et al. | 0 | 2015 | RA | 113 | PCI in CABG patients | 63±9 | 91 (80.5) | – | 6 (5.3) | 82 (72.6) | 6 (5.3) | – | 2.4±0.8 |
| FA | 291 | 63±9 | 232 (79.7) | 25 (8.6) | 191 (75.6) | 9 (3.1) | 2.5±0.8 | ||||||
| Duarte et al. | 0 | 2015 | RA | 251 | CA/PCI in CABG patients | 63±10 | 186 (74.1) | 31.8±7.2 | – | – | – | – | – |
| FA | 738 | 65±10 ∗ | 488 (66.2) ∗ | 30.1±6.3 ∗ |