Mental stress–induced myocardial ischemia (MSIMI) has been associated with adverse prognosis in patients with coronary artery disease (CAD), but whether this is a uniform finding across different studies has not been described. We conducted a systematic review and meta-analysis of prospective studies examining the association between MSIMI and adverse outcome events in patients with stable CAD. We searched PubMed, EMBASE, Web of Science, and PsycINFO databases for English language prospective studies of patients with CAD who underwent standardized mental stress testing to determine presence of MSIMI and were followed up for subsequent cardiac events or total mortality. Our outcomes of interest were CAD recurrence, CAD mortality, or total mortality. A summary effect estimate was derived using a fixed-effects meta-analysis model. Only 5 studies, each with a sample size of <200 patients and fewer than 50 outcome events, met the inclusion criteria. The pooled samples comprised 555 patients with CAD (85% male) and 117 events with a range of follow-up from 35 days to 8.8 years. Pooled analysis showed that MSIMI was associated with a twofold increased risk of a combined end point of cardiac events or total mortality (relative risk 2.24, 95% confidence interval 1.59 to 3.15). No heterogeneity was detected among the studies (Q = 0.39, I 2 = 0.0%, p = 0.98). In conclusion, although few selected studies have examined the association between MSIMI and adverse events in patients with CAD, all existing investigations point to approximately a doubling of risk. Whether this increased risk is generalizable to the CAD population at large and varies in patient subgroups warrant further investigation.
One-third to 1/2 of patients with coronary artery disease (CAD) develop myocardial ischemia in response to laboratory mental stress. Mental stress–induced myocardial ischemia (MSIMI) is a distinct phenomenon from physical (exercise or pharmacologic) stress–induced myocardial ischemia. Unlike physical stress–induced myocardial ischemia, MSIMI is less likely to result in chest pain and electrocardiographic changes, indicators of ischemia, and is not related to severity of coronary atherosclerosis. Although the exact mechanisms are unknown, MSIMI may in part result from abnormal vasomotion secondary to sympathetic nervous system activation. A number of observational studies have reported an association between MSIMI and adverse cardiac events or total mortality. Nonetheless, these studies were small and used a variety of stressor types and diagnostic criteria for MSIMI. Whether these variations affect the prevalence of MSIMI and its relation with adverse outcomes is not known. Clarification of the prognostic importance of MSIMI is fundamental, because, if its role is established, mental stress testing could transition from the research domain to clinical care. This is particularly true given that effective treatment modalities to reduce MSIMI are emerging. Therefore, we undertook a systematic review and meta-analysis with the primary objective of summarizing the existing evidence of the association between MSIMI and adverse outcomes in patients with CAD.
Methods
We systematically searched PubMed, EMBASE, Web of Science, and PsycINFO to identify prospective studies examining the association between MSIMI and subsequent outcomes in patients with CAD. Search terms, described in detail in the Supplementary Appendix , included “myocardial ischemia,” “ischemic heart disease,” “mental stress,” “psychological stress,” “mental* stress*,” “psychologic* stress*,” and “ischemi*.” The search was limited to studies published in English. To identify potential studies not captured by our database search strategy, we also searched studies listed in the bibliography of relevant publications and reviews.
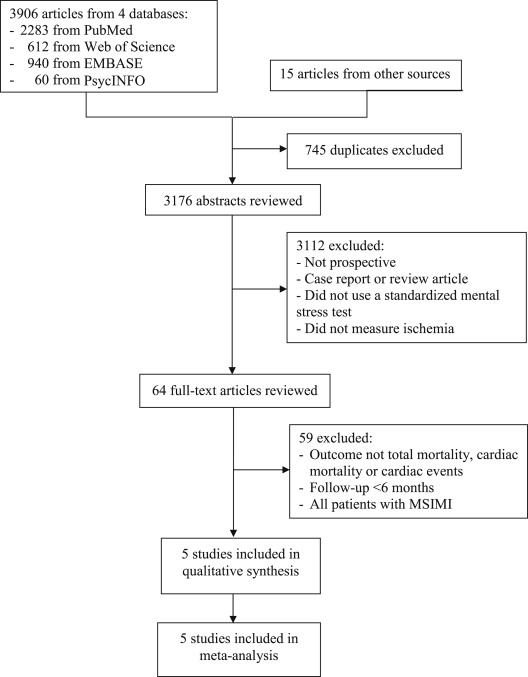
We included studies that (1) were prospective with a follow-up of at least 6 months; (2) were published in English in peer-reviewed journals from 1966 through March 2013; (3) included participants with documented stable CAD; (4) assessed presence of MSIMI using standardized mental stress tests and accepted techniques to assess ischemia; and (5) assessed recurrence of CAD events, cardiac mortality, or total mortality at follow-up. We further excluded studies in which all participants had MSIMI at baseline ( Figure 1 ).
Study selection was conducted in 2 steps. First, the titles of studies identified in our literature search were independently reviewed by 4 reviewers (JW, RR, CR, and VV). Second, the abstracts of studies that remained after the first-level screening were reviewed by 2 reviewers (RR and CR) and disagreements were reconciled.
Data from studies that met inclusion criteria were independently extracted by 2 reviewers (JW and CR). The data extracted included descriptive information about each study sample size, study design, follow-up length, type of mental stressor, method of assessing myocardial ischemia, and outcome variables. Disagreement was resolved by consensus or, when necessary, adjudicated by a third reviewer (RR). The definition of MSIMI was based on the criteria of each individual study.
Quality assessment was conducted using the Newcastle-Ottawa Scale for observational studies, which recognizes quality indicators in 3 general domains: selection of exposed and nonexposed cohorts (representativeness of the exposed cohort, selection of the nonexposed cohort, ascertainment of exposure, and demonstration of absence of outcome at the beginning of studies), comparability of exposed and nonexposed cohorts (analysis appropriately adjusted for potential confounding factors, such as medications, history of other chronic diseases, and lifestyle factors), and outcome ascertainment (adequacy of outcome assessment, length of follow-up, and adequacy of follow-up, i.e., losses are not related to either the exposure or the outcome). A study could be awarded a maximum of 1 point for each variable within each assessment domain (selection, comparability, and outcome) for a possible maximum total score of 8. The quality assessment was conducted independently by 3 reviewers (CR, RR, and AJS), and the results were reconciled until a consensus was reached.
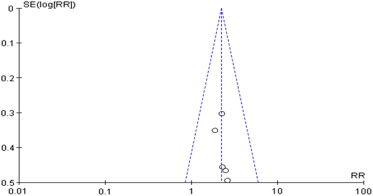
Relative risks and 95% confidence intervals were initially calculated from each study. Data were pooled across studies using fixed-effects meta-analysis models and weighted by the inverse of the estimated variance. A forest plot was created to illustrate individual and pooled risk estimates. Heterogeneity among studies was assessed with the I 2 statistic. A funnel plot was derived to assess publication bias; with this method, lack of bias is assumed if individual-level data are symmetrically distributed around the true mean, whereas publication bias is suggested if the funnel shape is asymmetrical. Subgroup analyses according to sample or protocol characteristics, such as patient demographics, type of stressor, method of MSIMI diagnosis, and length of follow-up, were planned but ultimately not carried out because of the limited number of included studies. All analyses were conducted using Review Manager 5.2 (The Cochrane Collaboration, Oxford, United Kingdom).
Results
The database search yielded a total of 3,906 citations ( Figure 1 ). An additional 15 studies were identified from the bibliography of relevant reports and reviews. After eliminating duplicates, 3,176 remained. Of these, 3,112 studies were not prospective and were therefore excluded. The 64 remaining reports were retrieved in full-text to be examined in more detail. Of these, 59 were ultimately excluded for not meeting other inclusion criteria. Five studies met the inclusion criteria and were included in the systematic review and meta-analysis.
The 5 cohort studies were all from the United States, and the pooled sample included 555 participants with 117 outcome events. Table 1 summarizes main study characteristics. The number of participants ranged from 30 in the study by Jain et al to 182 in the study by Sheps et al. The mean age ranged from 58 to 64 years. The proportion of women was small, and the pooled sample was 85% male. Three of the 5 studies did not provide information on the racial composition of the sample; in the remaining 2 studies the sample was predominantly white (96% and 77%, respectively). The follow-up period ranged from 35 days to 8.8 years.
| Study | n | % Women | Mean Age, y | Mean/Median Follow-Up (Range) | Stressor/Length | Criteria for MSIMI | Outcome | No. of Events | MSIMI Prevalence | Lost to Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|
| Jain (1995) | 30 | 0 | 64.0 | 2 y | Arithmetic/5–6 min | Reduction in LVEF ≥5% for ≥2 min by RNV | Non-fatal MI or unstable angina | 14 | 50% | 0 |
| Jiang (1996) | 126 | 11% | 59.0 | 44 m (2–5 y) | Arithmetic/3 min; PS/3 min; MT/3 min SI/20 min | WMA or reduction in LVEF >5% by RNV | Non-fatal MI, revasc, or cardiac death | 28 | 67% | 7% |
| Krantz (1999) | 79 | 4% | 58.0 | 3.5 y (2.7–7.3 y) | PS/5 min; Arithmetic/5 min; | WMA by echocardiography or RNV | Non-fatal MI, revasc, or cardiac death | 28 | 57% | 18% |
| Sheps (2002) | 182 | 14% | 63.0 | 5.2 ± 0.4 y | PS/5 min; ST/5 min | WMA by RNV | All-cause mortality | 15 | 20% | 7% |
| Babyak (2010) | 138 | 30% | 62.0 | 5.9 y (35 d–8.8 y) | PS/5 min; MT/5 min | Reduction in LVEF ≥5% by RNV | Non-fatal MI or all-cause mortality | 32 | 19% | 4% |
Except for one, all the studies used multiple mental stress tasks in a single session. These included various combinations of mirror tracing, public speaking, cognitive testing, structured interviews, and stroop testing. The length of mental stress testing also varied. Myocardial ischemia was assessed using radionuclide ventriculography in all studies; in one, echocardiography was also used. Criteria for MSIMI were not consistent and included the occurrence of wall motion abnormalities during mental stress, a reduction in left ventricular ejection fraction, or both. MSIMI was common in all 5 studies, but, consistent with the different assessment criteria, it varied substantially, from 19% to 67% ( Table 1 ). Clinical outcomes also differed across studies ( Table 1 ) and included all-cause mortality alone or in combination with varying CAD event types, including nonfatal myocardial infarction, cardiac death, revascularization procedures, or unstable angina.
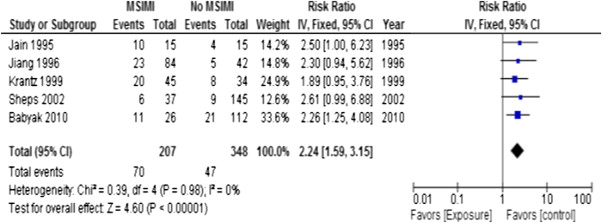
The meta-analysis of the 5 cohort studies indicated that there was a significantly higher risk of cardiac events or total mortality among CAD patients with MSIMI (pooled relative risk 2.24, 95% confidence interval 1.59 to 3.15; Figure 2 ). No significant heterogeneity of estimates was found among these 5 studies (Q = 0.39, I 2 = 0.0%, p = 0.98). The funnel plot ( Figure 3 ) showed good symmetry, which indicates that publication bias is not likely to exist in the analysis.
The methodologic quality of the 5 studies included in the meta-analysis, as scored with the Newcastle-Ottawa scale, is presented in Table 2 . The mean total score was 6.5 out of a maximum score of 7 (range 5.5 to 8) indicating that, overall, the methodologic quality was moderately good. The 5 studies generally received acceptable scores for the criteria of selection, comparability, and outcome, except for representativeness of the exposed group.



