Presence of left ventricular hypertrophy (LVH) has been reported to be associated with supraventricular and ventricular arrhythmias, but the association has not been systematically quantified and evaluated. A systematic search of studies in MEDLINE, EMBASE, CINAHL, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials databases was undertaken through April 2014. Studies reporting on LVH and sustained arrhythmias such as atrial fibrillation and supraventricular tachycardias (SVTs) and ventricular arrhythmias (tachycardia and fibrillation) were identified. Pooled effect estimates were calculated with random-effects models (DerSimonian and Laird). A total of 10 eligible studies with 27,141 patients were included in the analysis. The incidence of SVT in patients with LVH was 11.1% compared with 1.1% among patients without LVH (p <0.001). Patients with LVH had 3.4-fold greater odds of developing SVT (odds ratio 3.39, 95% confidence interval 1.57 to 7.31) than those without LVH, although significant heterogeneity was present (I 2 = 98%). Meta-regression analyses revealed the heterogeneity to have originated from differences in the baseline covariates such as age, male gender, hypertension, and diabetes of the individual studies. The incidence of ventricular arrhythmias was 5.5% compared with 1.2% in patients without LVH (p <0.001). The occurrence of ventricular tachycardia or fibrillation was 2.8-fold greater, in the presence of LVH (odds ratio 2.83, 95% confidence interval 1.78 to 4.51), and there was no significant heterogeneity (I 2 = 9%). Presence of LVH in hypertensive patients is associated with a greater risk of sustained supraventricular/atrial and ventricular arrhythmias, and there is an unmet need for identifying and refining risk stratification for this group.
Highlights
This systematic review and meta-analysis revealed that
- •
Patients with left ventricular hypertrophy (LVH) had 3.4-fold greater odds of supraventricular tachycardia.
- •
The patients with LVH had 2.8 times greater odds of ventricular tachycardia or fibrillation.
- •
Patients with LVH should therefore be risk stratified and followed up closely for earlier detection of these arrhythmias.
Ever since the first report from the Framingham cohort, a variety of studies have shown left ventricular hypertrophy (LVH) to be a blood pressure–independent powerful predictor of sudden cardiac death and other cardiovascular mortality and morbidity. Initially believed to be a benign adaptive process to compensate hemodynamic changes, LVH signifies response secondary to increased preload and afterload modulated by genetic, exogeneous, and neuroendocrine factors. Presence of LVH has often been implicated to be associated with clinically significant arrhythmias, but the association has not been systematically quantified and evaluated. Hence, we undertook a systematic review and meta-analysis to evaluate the association between LVH and sustained arrhythmias, particularly supraventricular arrhythmia (SVT) and ventricular arrhythmia (VT).
Methods
A comprehensive systematic search of studies published from January 1, 1966, to April 1, 2014, was conducted using MEDLINE, EMBASE, CINAHL, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials databases. Studies reporting on clinically significant sustained arrhythmias such as atrial fibrillation and SVT and ventricular arrhythmias (tachycardia and fibrillation) and LVH were identified. Studies were searched using the following text keywords and search strategy: “left ventricular hypertrophy” OR “hypertensive cardiomyopathy” OR “concentric cardiomyopathy,” “LVH” AND “arrhythmia,” OR “supraventricular arrhythmia” OR “ventricular arrhythmia” OR “ventricular tachycardia,” OR “ventricular fibrillation” OR “atrial fibrillation” OR “atrial flutter” OR “atrial tachycardia” OR “atrio-ventricular re-entrant tachycardia” OR “atrio-ventricular nodal re-entrant tachycardia” OR “supraventricular tachycardia.” A manual search of reference lists of appropriate review articles and original retrieved studies was also performed to identify studies potentially missed by the database searches. We did not impose any restrictions on language for the search.
Two physician-reviewers (SC and PS) independently reviewed originally identified titles and abstracts and selected studies for pooled analysis based on the study criteria. We selected studies that reported incidence and/or prevalence of SVT or VT in patients with and without LVH. Studies that reported data on presence of LVH and SVT, and LVH and VT both, were considered as 2 separate studies. Studies involving patients with hypertrophic cardiomyopathy were not included. We considered only high-grade arrhythmias, and studies reporting simple atrial or ventricular ectopy were not included. Only original articles were considered for this meta-analysis; reviews, letters to editors without original data, case reports, case series, and conference abstracts without peer-reviewed publication were excluded.
Two reviewers independently extracted data from all selected studies. The following data were extracted from each study: first author’s name, year of publication, mean age, gender distribution, prevalence of hypertension, LVH criteria, and incidence and/or prevalence of SVT or VT in patients with and without LVH. For studies that published data on LVH regression and arrhythmia, arrhythmia data after regression were collected to account for treatment changes when available. The quality of each study was assessed using the strengthening Meta-analysis of Observational Studies in Epidemiology (MOOSE) checklist and ratified with the Newcastle-Ottawa scale ( Supplementary Data ).
The meta-analysis was performed in accordance with the recommendations from the Cochrane Collaboration and the MOOSE statement. Pooled effect estimates were calculated with random-effects models (DerSimonian and Laird) because of known clinical and methodological heterogeneity of the studies. Heterogeneity was assessed using Higgins and Thompson I 2 statistic, with I 2 <25% considered low. In addition, in presence of heterogeneity, meta-regression was used to evaluate the modifying effect of common clinical and demographic variables, including age, gender, hypertension, and diabetes. Publication bias was estimated using funnel plots and the Egger regression test. A 2-tailed p <0.05 was considered statistically significant. All analyses were performed using Stata 11 (Stata Corp., College Station, Texas) and RevMan v5.02 (Nordic Cochrane Center, Copenhagen, Denmark).
Results
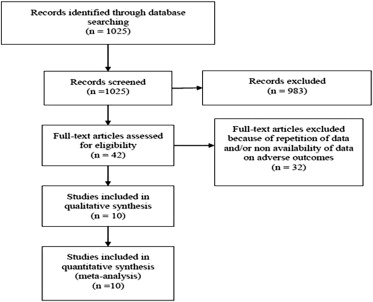
Our initial search identified 1,025 studies, of which based on our inclusion and exclusion criteria, 10 studies were selected for pooled analysis ( Figure 1 ). Characteristics of the 10 selected studies are listed in Table 1 . Two studies reported data on presence of LVH and SVT and also on LVH and VT and, hence, were considered as 2 separate studies herewith ( Table 1 ). The included studies comprised 27,141 patients, with 9,564 arrhythmia events in total. Of selected studies, 7 studies involving 21,606 patients reported data on SVT, of which 5 studies reported data on atrial fibrillation and LVH. Six studies with 5,535 patients reported data on LVH and VT. The incidence of SVT in patients with LVH was 11.1% compared with 1.1% among patients without LVH (p <0.001). There was a 3.4-fold greater odds of detecting supraventricular arrhythmias in association with presence of LVH (odds ratio 3.39, 95% confidence interval 1.57 to 7.31), although significant heterogeneity was present (I 2 = 98%; Figure 2 ). Meta-regression analyses revealed the heterogeneity to have originated from differences in the baseline covariates such as age, male gender, hypertension, and diabetes of the individual studies (residual I 2 = 0%). The incidence of ventricular arrhythmias was 5.5% compared with 1.2% in patients without LVH (p <0.001). There was a 2.8-fold greater odds of detecting clinically significant ventricular arrhythmias, in the form of ventricular tachycardia or fibrillation, in association with the presence of LVH (odds ratio 2.83, 95% confidence interval 1.78 to 4.51), no significant heterogeneity being present (I 2 = 9%; Figure 3 ).
| First Author (R) | Year | Patients | Age (Years) | Male (%) | Hypertension (%) | LVH Criteria | Arrhythmia | Number Patients With Arrhythmia in | |
|---|---|---|---|---|---|---|---|---|---|
| LVH | Non LVH | ||||||||
| Aronow | 1999 | 2,384 | 81 ± 9 | 35 | NR | ECHO | AF | 201/1,024 | 112/1,360 |
| Bender | 2012 | 317 | 67 ± 12 | 82 | NR | EKG | VT | 31/109 | 33/208 |
| Cea-Calvo | 2007 | 7,108 | 72 ± 7 | 46 | 73 | EKG | AF | 183/886 | 423/6,222 |
| Hennersdorf | 2007 | 104 | 63 ± 11 | 59 | 100 | ECHO | SVT | 12/47 | 5/56 |
| Hennersdorf | 2007 | 104 | 63 ± 11 | 59 | 100 | ECHO | VT | 2/47 | 1/56 |
| Levy | 1987 | 4,960 | 58 | 45 | NR | EKG/ECHO | VT | 6/843 | 12/3,994 |
| Martin-Rioboo | 2009 | 570 | 65 ± 11 | 46 | 60 | EKG | AF | 24/78 | 5/492 |
| McLenachan | 1987 | 150 | 58 ± 2 | 66 | 67 | EKG | VT | 14/50 | 5/100 |
| Novo | 1997 | 128 | 52 ± 9 | 68 | 100 | ECHO | SVT | 18/66 | 8/62 |
| Novo | 1997 | 128 | 52 ± 9 | 68 | 100 | ECHO | VT | 8/66 | 2/62 |
| Okin | 2006 | 8,861 | 67 ∗ | 45 | 100 | EKG | AF | 411/5,924 | 290/2,907 |
| Verdecchia | 2003 | 2,482 | 51 ± 12 | 53 | 100 | EKG | AF | 85/424 | 144/2,058 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


