Atrial fibrillation (AF) is a common arrhythmia encountered after coronary artery bypass graft surgery (CABG) and is associated with poor outcomes. The purpose of this study was to examine whether initiation of statins before CABG reduces the risk of postoperative AF. We searched for clinical trials that randomized patients who underwent CABG to preoperative statin therapy versus placebo. We required that the trial reported the incidence of postoperative AF. Random-effects summary odds ratio (OR) were constructed. Sensitivity analysis for the trials that reported AF as a primary outcome along with subgroup analyses according to the different statins used was also conducted. Twelve trials with 2,980 patients met our inclusion criteria. Atorvastatin was tested in 8 trials, whereas rosuvastatin was studied in 2 studies. Statins were associated with a lower risk of postoperative AF (OR 0.42, 95% confidence interval [CI] 0.27 to 0.66, p <0.0001). There was benefit with atorvastatin (OR 0.35, 95% CI 0.25 to 0.50, p <0.0001) but not rosuvastatin (OR 0.69, 95% CI 0.28 to 1.71, p = 0.42). On sensitivity analysis limited to trials that reported AF as a primary outcome, the risk of postoperative AF was still reduced with statins (OR 0.40, 95% CI 0.25 to 0.90, p = 0.02). The mean duration of the hospital stay was significantly lower in the statin group: 8.5 ± 1.8 days versus 9.1 ± 2.2 days (p <0.0001). Statin therapy, particularly atorvastatin, before CABG was associated with a reduction in the risk of postoperative AF.
Atrial fibrillation (AF) is a common arrhythmia encountered after coronary artery bypass graft surgery (CABG) with an estimated frequency of about 10% to 65%. Postoperative AF is associated with increased mortality, morbidity, and longer hospital stay. The increased levels of systemic inflammatory markers perioperatively have been postulated as one of the underlying mechanisms for postoperative AF. Statins or hydroxymethylglutaryl-CoA reductase inhibitors are important long-term medications in the management of patients with coronary artery disease who are awaiting CABG. Despite that, many eligible patients are not on statins. Beyond their lipid-lowering action, statins exert pleiotropic and anti-inflammatory effects, in which some studies and meta-analyses have shown a reduction in the risk of postoperative AF. More recently, a large, multicenter randomized trial demonstrated that initiation of statins before CABG did not prevent the risk of postoperative AF. Because of the uncertainty of the current available data, we conducted this comprehensive meta-analysis to evaluate whether statins initiated before CABG would reduce the risk of postoperative AF.
Methods
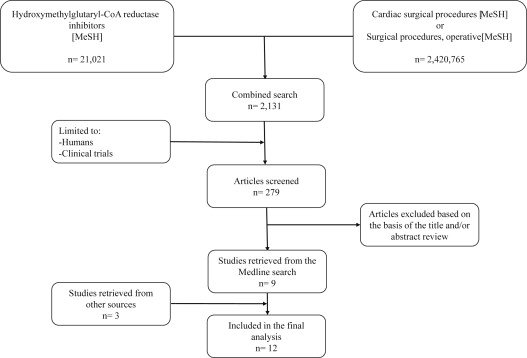
We performed a computerized literature search of the Medline database without language restriction from inception until January 2015 using the search strategy shown in Figure 1 . We also searched both the Web of Science database and the Cochrane Register of Controlled Trials using the key words “statins” and “coronary artery bypass graft.” Additionally, we searched for abstracts of the major scientific sessions until January 2015 using the same key words. To ensure that no potentially important studies were missed, the reference lists from the retrieved articles and previous meta-analyses were also checked.
We selected studies that randomized patients to receive statin therapy versus placebo before CABG. We required that the study reported the incidence of AF in both arms. We excluded studies in which statins were initiated after the surgery. If the study reported that the patients were on long-term statin therapy, we required that statin therapy be discontinued before randomization.
Two authors (IYE and AM) independently extracted data on study design, sample characteristics, sample size, intervention strategies, outcome measures, and other study characteristics from the included studies. Any discrepancies were resolved by consensus of the authors. For all clinical outcomes, we tabulated the number of events that occurred in each arm of each trial. When necessary for article clarification, we communicated with the corresponding author. For non-English articles, we used Google Translator (Google, Inc., Mountain View, California).
The primary outcome was postoperative AF. Secondary outcomes were all-cause mortality, myocardial infarction (MI), stroke, renal failure, the length of intensive care unit stay, and the total duration of the hospital stay.
For continuous variables, we calculated the mean and SD using 2-sided 2-sample t test. All outcomes were analyzed by the intention-to-treat analysis. Random-effects summary odds ratio (OR) were constructed using a DerSimonian-Laird model. We also performed fixed-effects summary OR using a Peto model for the rare outcomes. We assessed statistical heterogeneity for each outcome using the I 2 statistic. I 2 statistic values <25%, 25% to 50%, and >50% were considered as low, moderate, and high degree of heterogeneity, respectively. We examined the risk for publication bias using Harbord’s method. We conducted this meta-analysis based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Furthermore, the quality of the trials was evaluated based on the adequate description of treatment allocation, blinded outcome assessment, and description of losses to follow-up. All p values were 2 tailed, with statistical significance set at 0.05, and confidence intervals (CIs) were calculated at the 95% level for the overall estimates effect. All analyses were performed using STATA software, version 11 (STATA Corporation, College Station, Texas).
In our primary analysis, all statins were combined regardless of dose, type, or duration of therapy. To enhance the quality of the analysis, we conducted a sensitivity analysis for the trials that reported AF as the primary outcome. We also conducted subgroup analyses according to the type of statin used. Additionally, we performed a random-effects meta-regression analysis to explore the effect of the number of days that statins were initiated before CABG on the logarithm of the OR for AF.
Results
A total of 12 studies met our inclusion criteria with a total of 2,980 patients. Nine of the trials were retrieved from the Medline search, whereas the Web of Science database and the Cochrane Register of Controlled Trials search added 2 studies and 1 study was presented at the European Society of Cardiology 2014 meeting.
Atorvastatin 20 mg was tested in 6 studies, atorvastatin 40 mg in 2 studies, rosuvastatin 20 mg in 2 trials, pravastatin 40 mg in 1 study, and simvastatin 20 mg in 1 study. History of AF was an exclusion criteria in 5 studies, 1 study enrolled a small proportion patients (7% to 11%) with AF, whereas the remainder of the studies did not specify. All the included studies were conducted in a single center except for 1 trial that was multicenter. In 9 studies, patients underwent on-pump CABG. In 2 studies, patients underwent off-pump CABG, whereas another study allowed both on- and off-pump CABG. In 8 studies, patients who underwent emergency CABG were excluded, whereas the remainder of the studies did not report the indication for CABG. Patients with a recent history (<4 weeks) of MI were excluded in all studies except for 2 studies, in which 47% and 13% of the patients in the statin arm and 38% and 8% in the placebo arm had a history of MI, respectively. The concomitant use of ß blockers, amiodarone, and inotropes was comparable between the statin and placebo arms. In Table 1 , we report the baseline characteristics of the included studies, follow-up duration, and the treatment strategy of statin therapy. In Supplementary Table 1 , we list the perioperative medications, whereas the measures of study quality are listed in the Supplementary Table 2 .
| Study (ref#) | Year | Patients, S/P | Age (years) mean (SD) S/P | Male, % S/P | DM, % S/P | Statin arm | Initiation of statins prior to surgery (days) | Follow-up duration (days) |
|---|---|---|---|---|---|---|---|---|
| STICS | 2014 | 960/962 | NR/NR | NR/NR | NR/NR | Rosuvastatin 20 mg | 8 | 5 |
| Baran | 2012 | 30/30 | 61(9)/62(8) | 63/60 | 23/33 | Atorvastatin 40 mg | 14 | 30 |
| Sun | 2011 | 49/51 | 64(7)/65(8) | 65/69 | 37/39 | Atorvastatin 20 mg | 7 | 7 |
| Vukovic | 2011 | 29/28 | 61(8)/62(7) | 86/82 | 35/29 | Atorvastatin 20 mg | 21 | Hospitalization |
| Spadaccio | 2010 | 25/25 | 66(8)/65(7) | 52/56 | NR/NR | Atorvastatin 20 mg | 21 | Hospitalization |
| Ji | 2009 | 71/69 | 65(6)/66(9) | 68/71 | 38/38 | Atorvastatin 20 mg | 7 | Hospitalization |
| Mannacio | 2008 | 100/100 | 61(9)/59(8) | 75/70 | NR/NR | Rosuvastatin 20 mg | 7 | Hospitalization |
| Song | 2008 | 62/62 | 62(10)/64(9) | 63/68 | 47/52 | Atorvastatin 20 mg | 3 | 30 |
| Caorsi | 2008 | 21/22 | 68(7)/68(7) | 81/86 | 38/41 | Pravastatin 40 mg | 2 | 7 |
| Tamayo | 2007 | 22/22 | 68(7)/68(7) | 77/82 | 27/41 | Simvastatin 20 mg | 21 | Hospitalization |
| ARMYDA-3 | 2006 | 101/99 | 66(9)/67(8) | 79/68 | 32/42 | Atorvastatin 40 mg | 7 | Hospitalization |
| Chello | 2006 | 20/20 | 66(8)/64(7) | 80/75 | NR/NR | Atorvastatin 20 mg | 21 | Hospitalization |
Postoperative AF was the primary outcome in 5 studies. Four studies defined postoperative AF as an episode of AF lasting for >5 minutes observed on either a telemetry monitor or electrocardiogram, whereas 1 study used a Holter monitor for 5 days to detect any episodes of AF. The remainder of the studies did not specifically define AF.
The risk of postoperative AF was 19.9% in the statin group versus 25.8% in the placebo group (OR 0.42, 95% CI 0.27 to 0.66, p <0.0001, I 2 = 66%; Figure 2 ). There was an evidence of publication bias with Harbord’s test (p = 0.001). On the sensitivity analysis limited to the trials reporting AF as the primary outcome, the risk of postoperative AF was OR 0.48 (95% CI 0.25 to 0.90, p = 0.02, I 2 = 81%).
When each statin was tested separately, atorvastatin was associated with a reduction in the risk of postoperative AF (OR 0.35, 95% CI 0.25 to 0.50, p <0.0001, I 2 <0.1%) with no evidence of publication bias (p = 0.22). The risk of postoperative AF was not reduced with rosuvastatin (OR 0.69, 95% CI 0.28 to 1.71, p = 0.42, I 2 = 86%; Figure 3 ). We could not perform a separate analysis for either pravastatin or simvastatin because of the limited number of studies in these subgroups. On meta-regression analysis, the log OR of postoperative AF was nonsignificantly reduced when the duration of preoperative statins was increased (p = 0.15; Supplementary Figure 1 ).




