Mesenteric Ischaemia I Severe occlusive disease of at least two of the three mesenteric vessels, resulting in a reduction in blood flow to the gut. This is caused by mesenteric artery stenosis (usually at the vessel origin) leading to a chronic or intermittent decrease in mesenteric perfusion. Theoretically, two vessels need to be involved for symptoms to develop (controversial). Patients often complain of post-prandial abdominal pain (due to gut malperfusion during digestion) referred to as mesenteric angina. In addition, they may practise food avoidance (due to pain) with weight loss (malabsorption and food avoidance), but can compensate by eating smaller meals more frequently (‘small meal syndrome’). Malabsorption may lead to diarrhoea and steatorrhoea with a risk of vitamin deficiency (especially fat-soluble [A, D, E, K]). Other non-specific features include anorexia, nausea and vomiting.
Classification
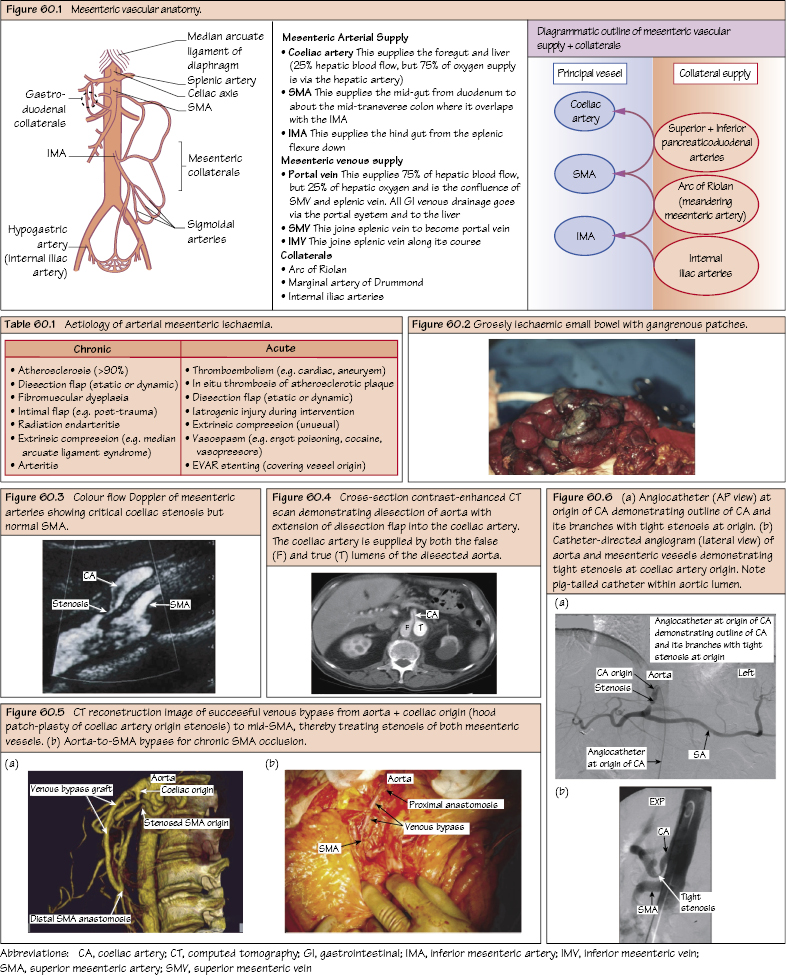
Mesenteric Arterial Ischaemia
Presentation
Chronic Mesenteric Ischaemia (CMI)
Clinical Features
Investigations and Diagnosis
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


