Fig. 35.1
Melody percutaneous pulmonary valve, in the close (left) and open (right) position, mounted on a platinum-iridium stent
35.3.2 The Delivery System
The delivery system, Ensemble, also manufactured by Medtronic, MN, includes a balloon-in-balloon (BiB) design onto which the valved stent is front-loaded and crimped (Fig. 35.2). The system is available with three outer balloon diameters: 18, 20, and 22 mm. The tip of the system is blue to correspond with the blue outflow suture on the device to help with correct orientation. The body of the Ensemble system consists of a one-piece Teflon sheath containing a braided wire-reinforced elastomer lumen. The design minimizes the risk of kinking while optimizing flexibility and retaining the pushability required for the procedure. There is a retractable sheath which covers the stented valve during delivery and is withdrawn just prior to deployment. Proximally, there are three ports, one for the guidewire (green), one to deploy the inner balloon (indigo), and one to deploy the outer balloon (orange).
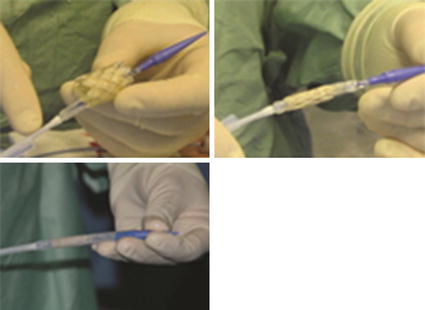
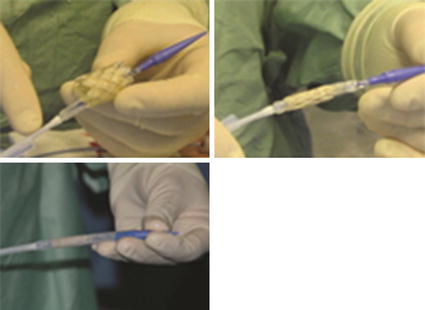
Fig. 35.2
Loading of the PPVI stent onto the delivery catheter
35.4 Procedure
Preparation
General anesthesia and orotracheal intubation.
Biplane catheterization laboratory preferred.
Patient position with arms lifted up, behind the patient’s neck (attention to brachial plexus overstretching).
Patient is fully monitored including an arterial line for continuous arterial pressure monitoring, two peripheral venous lines or a central venous line, and vesical catheter for diuresis evaluation.
Full anticoagulation is obrained by administering intravenously 100 UI/kg of heparin. Check hourly the activated clotting time >250 s. In case add heparin IV during the procedure. Usually it is not needed.
Antibiotics IV: usually a cephalosporin.
The procedure has to be considered as a surgical intervention. Therefore, special care has to be paid for strict asepsis. Special attention has to be given to operators’ scrubbing and patient’s preparation (including careful depilation). The personnel involved has to wear masks and hats.
35.5 Access Site
Usually a femoral access is used. Sometimes the internal jugular access can be used.
Both sides for vascular femoral access are prepared.
A 12 Fr femoral sheath is placed: this helps because the need for changing femoral sheath is avoided during diagnostic catheterization, balloon sizing, balloon testing, angiographies with 6 Fr multitrack catheter (NuMED Inc., Hopkinton, NY), or 9 Fr Mullins sheath (Cook Europe, Bjaeverskov, Denmark).
Arterial access is obtained by using a 5 Fr sheath.
35.6 Catheterization and Hemodynamic Evaluation
Right heart catheterization is performed using standard techniques to assess pressures and saturations with a right coronary catheter, JR 3.5, or any other catheter with a curved tip.
Routinely, pressure measurements are obtained in the right ventricle, pulmonary artery, and aorta with additional measurements, for example, in the branch pulmonary arteries.
A 0.035″ super-stiff guidewire is then positioned in a distal branch pulmonary artery to provide an anchor over which the delivery system can be advanced. It is important to avoid curves as much as possible, to place the tip of the wire as distal as possible (ideally in the pulmonary artery bed at the level of the diaphragm) and to be sure that the wire is not passing through the chordae of the tricuspid valve (check by using a multitrack catheter or a balloon-tipped catheter with the balloon inflated).
The preferred guidewire is usually a 0.035″ exchange wire (Amplatz Ultra Stiff wire 260 cm long (Boston Scientific Corp., Natick, MA), Lunderquist 260 cm long (Cook Europe, Denmark), Back-up Meier 300 cm long (Boston Scientific Corp., Natick, MA).
Special care has to be paid to wire stability and position. This should not move during the procedure. If, in any phase of the procedure, the wire moves and the position is not satisfactory, replace in the ideal position with the use of a catheter. Never push forward the stiff wire because of the risk for pulmonary vascular bed injuries.
Angiography is performed using a 6 Fr multitrack catheter (NuMED Inc., Hopkinton, NY) or through a 9 Fr Mullins long sheath with the tip placed just beyond the pulmonary valve. In the latter case, a pigtail with radiopaque markers is placed across the wire inside the Mullins sheath in order to allow for precise measurements (Fig. 35.3).
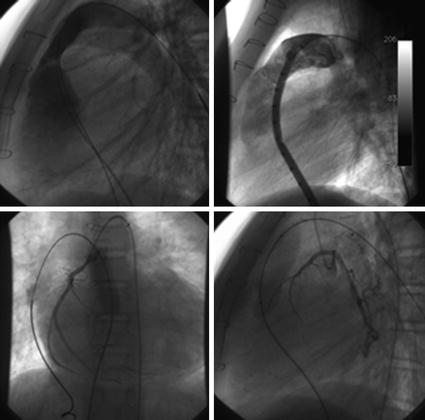
Fig. 35.3
Left upper: Angiography in lateral view showing severe stenosis and regurgitation at the level of the RVOT; right upper: Angiography in lateral view of the RVOT through the lateral port of the Mullins sheath after pre-dilatation of the RVOT; left and right bottom: balloon RVOT testing during simultaneous coronary angiography
Angiographies are performed in the pulmonary artery trunk, right ventricle, and ascending aorta (Fig. 35.3).
Usually the following imaging planes are used:
Lateral View
To visualize the anterior chest, landing zone, and proximal end of pre-stent
Useful to check coronary arteries involvement during balloon testing
Anteroposterior View with Cranial Angulation Usually Associated to Left Anterior Oblique Angulation
To visualize relation to bifurcation and distal end of stent.
Useful to check coronary artery involvement during balloon testing.
If needed, selective coronary artery angiography is performed.
Delineate landing zone and decide about final target diameter to be achieved with Melody valve.
In case of doubt on the characteristics of the landing zone, it can be useful to do as follows:
Get Clinical Tree app for offline access
Use a sizing balloon (34 mm Amplatzer ASD sizing balloon(NuMED Inc., Hopkinton,NY). This gives a precise negative image of the RVOT and landing zone.
Then use a low-pressure angioplasty balloon (e.g., a Z-Med II balloon, NuMED Inc., Hopkinton, NY) or Crystal balloons (Balt, Montmorency, France) in order to check for tissue distensibility
As a further step, if the tissue looks poorly distensible with low-pressure balloons, use a high-pressure balloon (Mullins X Ultra high-pressure balloon catheter, NuMED Inc., Hopkinton, NY), Atlas PTA balloon dilatation catheter (Bard, Tempe, AZ, USA)
In this latter case, two situations should be considered:
Presence of a lesion with high risk of tear. This can be anticipated in case of a heavily calcified lesion.
Potential for coronary compression.
If there is a possibility that a coronary artery is at risk of compression from valve implantation, coronary angiography is performed with an angioplasty balloon inflated simultaneously in the right ventricle to pulmonary artery conduit. If there is a high risk of coronary arterial compression, valve implantation should not be attempted, and the patient should be referred for surgery.
Selective coronary angiography is preferred in multiple projections (Fig. 35.3).
If coronary arteries are distant, low pressure will be enough.< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


