Megacode Review
 Just the facts
Just the factsIn this chapter, you’ll learn:
♦ the role of the team leader during the Megacode
♦ the role of the team members performing airway management, cardiopulmonary resuscitation, and emergency medication administration
♦ appropriate actions to take during emergency situations.
A look at the Megacode
The Megacode station in an advanced cardiac life support (ACLS) class provides a rehearsal to help team members organize their roles when involved in a real code situation. A case study approach is used to present a realistic picture of what occurs during a code. Each student takes a turn at each of the four roles:
team leader
team member in charge of airway management
team member in charge of cardiopulmonary resuscitation (CPR)
team member in charge of I.V. access and drug administration.
|
Team member roles
During the Megacode, the team leader serves as the director of care activities and delegates responsibilities to the other team members accordingly. The team leader assesses and manages circulation, airway, breathing, and defibrillation. Other components of the team leader role include:
monitoring the quality of CPR being performed
long-term objectives such as controlling rescuers and bystanders on the scene
investigating the existence of advance directives
deciding when to stop resuscitation
incorporating family needs and concerns during and after the resuscitation process
providing opportunities to conduct an objective critique of the resuscitation event.
There’s no “I” in team
Remember, the team leader needs to be open to suggestions from other team members because many different activities occur simultaneously during a Megacode. For example, the team member administering drugs may notice that 3 minutes have passed since the last dose of epinephrine was given or the team member who intubated the patient may realize that breath sounds haven’t been checked. Team members who respond to code situations frequently can quickly and smoothly work through algorithms because they need infrequent prompting from the team leader to perform appropriately to achieve a positive outcome.
Algorithms
Within the Megacode, algorithms serve as guides to patient care, pointing the team in a unified direction. However, don’t use an algorithm as a replacement for your team’s assessment skills. Remember that research findings may alter the current recommendations, so team members must keep up-to-date and be aware of changes in standards of practice.
|
Megacode testing
At Megacode testing stations, the ACLS instructor will give you a brief patient scenario. These stations typically include any equipment the situation demands. Before testing day, you’ll be given the opportunity to practice with the equipment.
Some instructors try to set up scenarios that apply to the student’s likely work situation. For example, if the student is a critical care nurse, the patient situation may take place in an intensive care setting. If the student is employed in a free-standing surgical center, the situation may occur there.
Raise your hand
When presented with the patient situation, you may find that you need additional information to take an action or make a
sound decision. Don’t be afraid to ask for that information. If you ordered an arterial blood gas analysis, you might need to ask if the results have arrived. This information is helpful if you need to make adjustments in oxygenation.
sound decision. Don’t be afraid to ask for that information. If you ordered an arterial blood gas analysis, you might need to ask if the results have arrived. This information is helpful if you need to make adjustments in oxygenation.
|
In turn, the instructor may ask you for information that’s appropriate to the situation. For example, she may ask you if an alternative medication could be given or remind you that an I.V. line hasn’t been started (or that the team is trying to insert a line). The instructor won’t be trying to trick you, but she will be trying to determine if you’re thinking along the correct route or simply guessing. A seasoned instructor can differentiate an unprepared student from a nervous one and will provide guidance to redirect you back to the algorithm.
Line up!
It may be helpful to line up the equipment as you intend to use it or in an order you find most comfortable. You may also use the equipment to remind yourself about what has occurred during the testing scenario. For example, you might place epinephrine nearer to the patient’s I.V. site as a reminder that one dose has been given.
Sample Megacode scenarios
Here are three simulations to help you prepare for the Megacode section of the ACLS examination. Remember to only look at each scenario from the perspective of one team member at a time because trying to think about every single responsibility may prove overwhelming.
Scenario #1
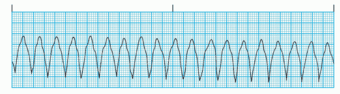
INSTRUCTOR: A patient arrives in your emergency department (ED) complaining of palpitations and mild dizziness. She’s visibly anxious and crying. Her vital signs are: blood pressure, 98/50 mm Hg; heart rate, 210 beats/minute; and respiratory rate, 24 breaths/minute. You attach a pulse oximeter and her oxygen saturation is 90%. You attach her to the monitor, which shows this rhythm:
|
|
TEAM LEADER: The rhythm on the monitor appears to be ventricular tachycardia (VT). I would perform a CABD assessment and administer oxygen 4L/minute by nasal cannula.
INSTRUCTOR: The CABD assessment indicates that the patient is conscious and breathing with a palpable pulse. The patient’s airway is natural and her breathing is adequate. Oxygen is in place by nasal cannula. An I.V. line has been started and a 12-lead electrocardiogram (ECG) is performed. A diagnosis of stable VT is made.
TEAM LEADER: I would direct a team member to administer adenosine 6 mg IV as quickly as possible, followed by a 20-mL saline flush.
INSTRUCTOR: There is no change in rhythm.
TEAM LEADER: I would direct a team member to give adenosine 12 mg as quickly as posssible followed by a 20-mL saline flush.
INSTRUCTOR: That’s correct. There is no change in rhythm. The patient’s blood pressure is 70/20 mm Hg and she has become more restless. She’s arousable but can’t answer questions.
TEAM LEADER: I would check the carotid pulse.
INSTRUCTOR: The patient’s carotid pulse is present with this rhythm.
TEAM LEADER: Does this defibrillator deliver monophasic or biphasic energy?
INSTRUCTOR: It’s a biphasic device.
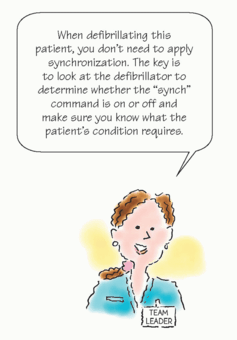
TEAM LEADER: I would direct a team member to place the defibrillator’s gel pads or “hands off” pads on the patient’s chest. I would announce “all clear” and “remove oxygen source from patient” and visually confirm that team members are clear of the patient and the oxygen is turned off. I would select the synchronize mode on the defibrillator and perform synchronized cardioversion at 100 joules.
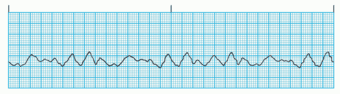
INSTRUCTOR: The patient converts to this rhythm after cardioversion:
|
|
TEAM LEADER: I would check the carotid pulse.
|
INSTRUCTOR: The patient’s carotid pulse is checked and is absent.
TEAM LEADER: I would then turn off the synchronize mode on the defibrillator, visually verify and announce “all clear” and “remove oxygen source from patient,” and defibrillate the patient at 200 joules.
INSTRUCTOR: The patient’s carotid pulse is absent with no change in rhythm.
TEAM LEADER: I would direct team members to perform CPR, beginning with chest compressions. I would monitor the quality of the compressions and the bag-mask ventilations. I would have the team intubate the patient in less than 10 seconds or insert a supraglottic advanced airway based on their skill level, and administer epinephrine 1 mg by I.V. push. CPR shouldn’t be interrupted to place a supraglottic advanced airway.
INSTRUCTOR: An endotracheal (ET) tube is placed and confirmed with five-point chest auscultation and secondary confirmation and monitoring using waveform capnography is begun. Epinephrine is administered and CPR is in progress.
TEAM LEADER: I would announce “all clear” and “remove oxygen source from patient,”and then defibrillate the patient at 200 joules after 2 minutes of CPR. I would then have to team immediately resume chest compressions, making sure team members switch performing compressions every 2 minutes. I would administer amiodarone 300 mg by rapid I.V. infusion diluted in 20 to 30 mL of dextrose 5% in water (D5W).
INSTRUCTOR: Amiodarone is administered.
TEAM LEADER: I would visually verify and announce “all clear” and “remove oxygen source from patient” and then defibrillate the patient again at 200 joules after 2 minutes of CPR.
INSTRUCTOR: The patient is defibrillated.
TEAM LEADER: I would resume CPR for 2 minutes and then check the carotid pulse and rhythm on the monitor.
INSTRUCTOR: There’s no change in the patient’s pulse or cardiac rhythm.
TEAM LEADER: I would direct team members to continue CPR and, if it has been 3 to 5 minutes since 1 mg of epinephrine was given, I would administer vasopressin 40 units by I.V. push.
INSTRUCTOR: Vasopressin is administered.