Percutaneous mitral valve repair with the MitraClip has been shown to decrease mitral regurgitation (MR) severity, left ventricular volumes, and functional class in patients with severe (3+ or 4+) MR. Determination of which patients are optimal candidates for MitraClip therapy versus surgery has not been rigorously evaluated. Transesophageal echocardiography was prospectively performed in 113 consecutive patients referred for potential MitraClip therapy under the REALISM continued access registry. MR severity was assessed quantitatively in all patients. Mitral valve anatomy and feasibility of MitraClip placement were assessed by transesophageal echocardiography and clinical parameters. MR was degenerative (mitral valve prolapse) in 60 patients (53%), functional (anatomically normal) in 44 (39%), and thickened with restricted motion (Carpentier IIIB classification) in 9 (8%). MR was mild in 19 patients (17%), moderate in 27 (24%), and severe (3 to 4+) in 67 (59%) by Transesophageal echocardiography. MitraClip placement was performed in only 17 of 113 patients (15%); all were successful. Surgical mitral valve repair was performed in 25 patients (22%), mitral valve replacement in 12 (11%). Most patients (59 of 113, 52%) were treated medically, usually because MR was not severe enough to warrant intervention. In conclusion, most patients referred for MitraClip therapy do not have severe enough MR to warrant intervention. Of those with clinical need for intervention, surgery is more often recommended for anatomic or clinical reasons. Three-dimensional transesophageal echocardiography with quantitative assessment of MR severity is helpful in evaluating these patients.
Severe mitral regurgitation (MR) is associated with left ventricular (LV) dysfunction, heart failure, atrial fibrillation, and death. This is true regardless of whether MR is caused by a primary lesion of the mitral apparatus or is secondary to global or regional LV dysfunction (functional MR). In functional MR, medical therapy, cardiac resynchronization, or revascularization may decrease MR severity if reverse remodeling of the left ventricle occurs. There is no evidence that medical therapy directly decreases MR severity or improves clinical outcomes in primary MR. Thus, severe MR is considered a surgical disease. Surgical repair is superior to valve replacement and is recommended even in asymptomatic patients if the likelihood of repair is ≥90%. Recently a percutaneous Alfieri-type repair (MitraClip, Abbott Vascular Structural Heart, Menlo Park, California) has been shown to decrease MR severity, LV volumes, and New York Heart Association functional class in patients with moderately severe (3+) or severe (4+) MR. In the randomized Endovascular Valve Edge-to-Edge Repair Study (EVEREST) II, surgery was more effective than the MitraClip at decreasing MR severity but was not as safe, primarily because of an increased need for transfusion. Determination of which patients are optimal candidates for MitraClip therapy versus surgery has not been rigorously evaluated. This report presents the results of transesophageal echocardiography (TEE) in screening potential candidates for MitraClip therapy in a single institution participating in the on-going Continued Access Registry of the Evalve MitraClip System (REALISM), a prospective multicenter continued access registry of EVEREST II.
Methods
From November 2008, when EVEREST II enrollment ended, through March 2011, we performed TEE studies in 113 consecutive patients referred for potential MitraClip therapy for severe MR. All patients were judged by the referring cardiologist or cardiovascular surgeon to have moderately severe or severe MR based on transthoracic echocardiogram and in some cases TEE obtained at the referring medical center. Because all patients were referred after EVEREST II trial enrollment ended, the decision to perform MitraClip repair, surgical repair or replacement, or not to intervene was based on clinical judgment and not on the randomization process.
TEE was performed by a single operator (P.A.G.) under conscious sedation and topical pharyngeal anesthesia. TEE studies were performed using a Philips iE33 and Matrix array X7-2 3-dimensional TEE probe (Philips Ultrasound, Andover, Massachusetts). A standard protocol was used to obtain 2-dimensional TEE images according to American Society of Echocardiography guidelines. Vena contracta imaging of the MR jet in a long-axis view was obtained. Proximal isovelocity surface area (PISA) imaging was performed with the baseline shifted in the direction of the jet to optimize the hemispheric shape and maximize the PISA radius with angle correction, if necessary. Continuous-wave Doppler was performed in the best view that aligned with the MR jet. For markedly eccentric jets, transthoracic imaging with a Pedof transducer was performed after withdrawal of the TEE probe. Pulse-wave Doppler was used to measure mitral inflow velocities and pulmonary vein velocities. Live 3-dimensional and full-volume (with and without color Doppler) image acquisitions were then obtained.
MR severity was judged using a hierarchical algorithm based on American Society of Echocardiography guidelines. The primary determinant of MR severity was effective regurgitant orifice area (EROA) by the PISA technique when a clearly defined and measurable proximal flow convergence region was identified. EROA <0.2 cm 2 was considered mild, 0.2 to 0.3 cm 2 moderate, and ≥0.3 cm 2 severe (3+ or 4+) MR. In 1 case MR was graded as severe because EROA of 0.28 cm 2 was accompanied by systolic flow reversal in the 2 superior pulmonary veins and vena contracta width was 0.7 cm. If EROA by PISA was not measurable, vena contracta width was used. Inability to calculate EROA was invariably due to markedly eccentric jets with inability to properly align the continuous-wave Doppler beam with the MR jet. A vena contracta width ≤0.3 cm was considered mild MR and ≥0.6 cm was considered severe MR. If the vena contracta was intermediate, MR grade was increased to severe if there was 2 of the following: a flail leaflet, PISA radius >0.9 cm, pulmonary vein systolic flow reversal, or mitral early (E) velocity ≥1.2 m/s. In all patients the EROA or vena contracta was measurable.
Results
Demographics of patients are listed in Table 1 . Mean age was 69 years; 57% were women. Known coronary artery disease, defined as angiographic stenosis >50% or previous percutaneous coronary intervention or coronary artery bypass grafting, was present in 39%. Hypertension, heart failure, or atrial fibrillation was present in >1/2. LV ejection fraction was 48.5 ± 14.8%.
| Age (years) | 68.6 ± 13.3 |
| Men/women | 48 (42%)/65 (57%) |
| Hypertension | 65 (58%) |
| Diabetes mellitus | 24 (21%) |
| Coronary artery disease ⁎ | 44 (39%) |
| Previous coronary bypass surgery | 29 (26%) |
| Heart failure | 66 (58%) |
| Atrial fibrillation | 57 (50%) |
| Left ventricular ejection fraction (%) | 48.5 ± 14.8 |
⁎ Defined as >50% stenosis on angiogram or previous percutaneous coronary intervention or coronary bypass surgery.
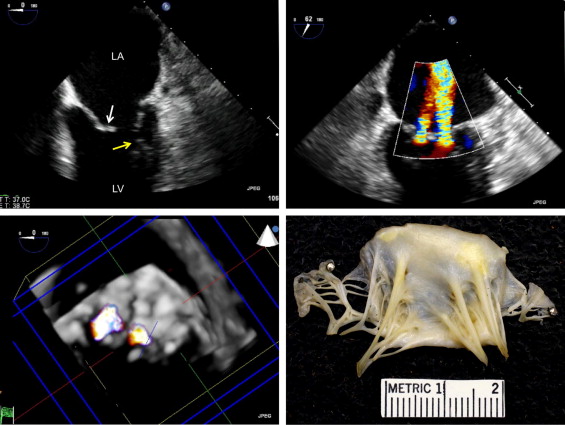
As presented in Table 2 the mechanism of MR was degenerative in 60 patients (53%), functional in 44 (39%), and combined leaflet thickening and restricted systolic and diastolic motion (Carpentier IIIB classification) in 9 (8%). Figure 1 shows an example of a patient with Carpentier IIIB MR in whom surgical pathology found nonspecific inflammation and scarring of the 2 leaflets. In patients with degenerative MR, a flail leaflet with torn chords was seen in 26 of 60 patients (43%). Barlow valve with marked thickening, redundancy, and prolapse of the 2 leaflets was present in 10 (17%) and fibroelastic deficiency (prolapse with thin leaflets) in 50 (83%). Isolated posterior leaflet prolapse or flail was present in 36 (60%), bileaflet involvement in 20 (33%), and anterior leaflet involvement in 4 (7%). In patients with degenerative MR, LV ejection fraction was 54.8 ± 9.2%.
| Mechanism of mitral regurgitation (n = 113) | |
| Degenerative | 60 (53%) |
| Functional | 44 (39%) |
| Other (Carpentier class IIIB) | 9 (8%) |
| Severity of mitral regurgitation (n = 113) | |
| Mild (1+) | 19 (17%) |
| Moderate (2+) | 27 (24%) |
| Severe (3 or 4+) | 67 (59%) |
| Outcome (n = 113) | |
| MitraClip | 17 (15%) |
| Mitral valve repair | 25 (22%) |
| Mitral valve replacement | 12 (11%) |
| Medical therapy only | 59 (52%) |
| MitraClip not implanted (n = 95) | |
| Mitral regurgitation less than severe (3–4+) | 46 (48%) |
| No A2–P2 coaptation | 11 (12%) |
| Flail width >1.5 cm | 6 (6%) |
| Elected surgical repair | 6 (6%) |
| Carpentier IIIA restriction | 6 (6%) |
| Needed other heart surgery | 4 (4%) |
| Previous mitral valve repair | 4 (4%) |
| Too ill/limited life expectancy | 3 (3%) |
| Severe annular calcification | 3 (3%) |
| Large cleft in posterior leaflet | 3 (3%) |
| Leaflets deemed not graspable | 2 (2%) |
| Died at home awaiting MitraClip | 1 (1%) |
| Transesophageal echocardiogram not suitable for guidance | 1 (1%) |
In the 44 patients with functional MR, 8 (18%) had an isolated inferior/posterior wall motion abnormality and 36 (82%) had multiple regional wall motion abnormalities or global hypokinesia. LV ejection fraction was 38.5 ± 16.4%.
MR was mild in 19 patients (17%), moderate in 27 (24%), and severe (3 to 4+) in 67 (59%) by quantitative TEE parameters. EROA by PISA ranged from 0.05 to 1.4 cm 2 ; vena contracta width was 0.2 to 1.1 cm. There was a statistically significant difference in the distribution of MR severity between patients with degenerative MR and those with functional MR (p = 0.0018). In the 60 patients with degenerative MR, 44 (73%) had severe MR by quantitative TEE measurements, 10 (17%) had moderate MR, and 6 (10%) had mild MR. In the 44 patients with functional MR, 17 (39%) had severe MR, 16 (36%) had moderate MR, and 11 (25%) had mild MR.
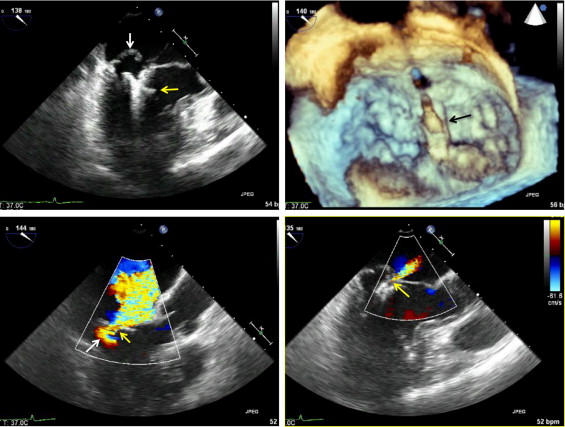
Based on TEE results and clinical data, 17 of 113 patients (15%) underwent MitraClip placement under the REALISM protocol. The procedure was successful in all 17 in decreasing MR severity ( Figure 2 ); there were no partial clip detachments or embolization. Surgical mitral valve repair was performed in 25 patients (22%) and mitral valve replacement in 12 (11%). Most patients (59 of 113, 52%) were treated medically, usually because MR was not severe enough to warrant intervention.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


