10 Masses and Devices
Key Points
• The knowledge of normal anatomic variants is critical. Incorrect identification of a mass as pathologic may lead to unnecessary diagnostic tests and treatments including surgery.
• The “coumadin ridge,” if not imaged correctly, may appear as a free-floating structure in the left atrium (LA).
• Lambl’s excrescences are degenerative strands on the aortic valve (AV) and are of no clinical significance.
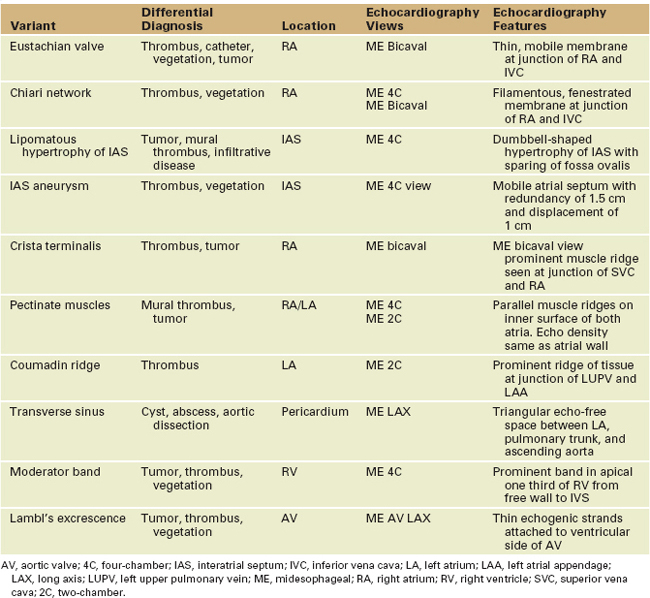
Several normal cardiac structures may mimic abnormal masses. In this section, we describe some of the structures (Table 10-1) that are frequently mistaken for pathologic entities.
Right Atrium
Crista Terminalis
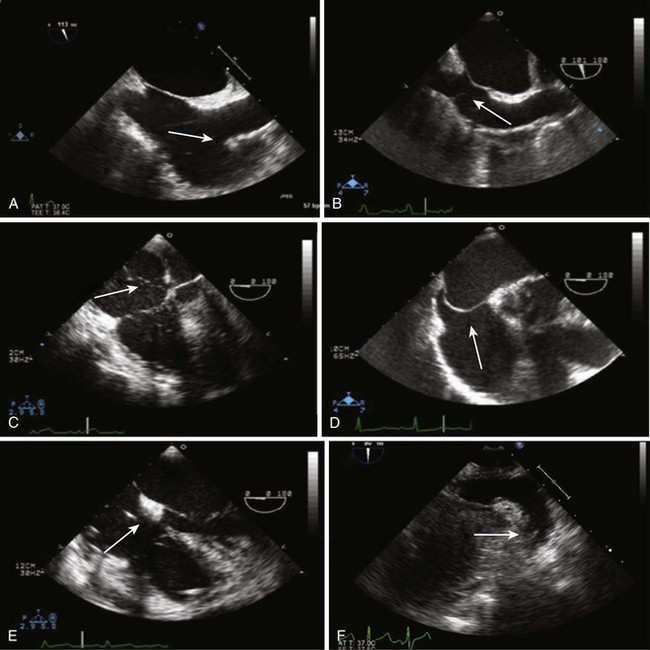
• Best seen in the midesophageal (ME) bicaval view, adjusting the probe depth to display the SVC-RA junction.
Eustachian Valve
• Can be differentiated from thrombus by its typical location, attachment to the RA, and filamentous appearance.
Left Atrium
Right Ventricle
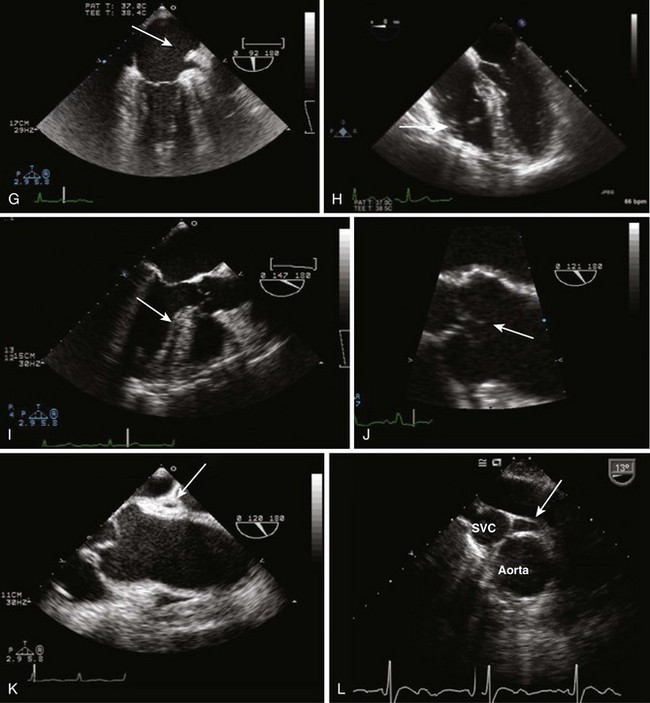
• Moderator band: prominent apical muscle band from septum to the anterior papillary muscle (PM; see Figure 10-1H).
• RV is heavily trabeculated, and with right ventricular hypertrophy (RVH) trabeculations, become very prominent.
• Catheters within the RV can appear as small mobile echo densities that resemble intracardiac masses.
Left Ventricle
• Aberrant chordae tendinae: abnormal extra MV chordae without structural function. Typically attached to the MV leaflets or to primary or secondary chordae. Homogeneous in structure, can be thickened compared with other chordae.
• Distal hypertrophy of the interventricular septum (IVS) with sigmoidal appearance: normal variant of aging and hypertension (see Figure 10-1I).
Aortic Valve
• Nodules of Arantius: points of coaptation of the AV. Seen at the tip of the AV as small globular thickening.
• Lambl’s excrescences: degenerative strands on either side of the AV (see Figure 10-1J). Commonly seen in older patients. They have no pathologic implications.
Pericardium
• There is good correlation between TEE and computed tomography (CT) measurements of pericardial thickness.
Transverse Sinus, Fat Pad, Cyst
Transverse Sinus
• It is seen as a triangular echo-free space between the ascending aorta, pulmonary trunk, and LA when filled with pericardial fluid.
• Best imaged in the ME long axis (LAX) view between the ascending aorta and the right pulmonary artery (PA; see Figure 10-1K).
Fat Pad
• A hypoechoic space anterior to the parietal pericardium. It is most often found adjacent to the RV and the LV apex.
Transesophageal Echocardiography Assessment of Intracardiac Masses
• TEE is the gold standard in the diagnosis of vegetations and intracardiac thrombi, although visualization of the ventricular apex may not always be accurate.
Systematic Transesophageal Echocardiography Assessment of Intracardiac Masses
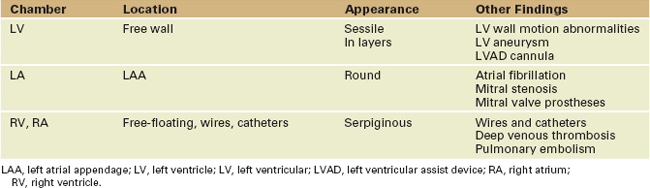
Intracardiac Thrombi
• Fresh thrombi are more mobile and friable, thus at higher risk of embolization (see Case 10-3 on the Expert Consult website).
• Older thrombi are more stable, are organized in layers, and may present initially with calcification.
Spontaneous Echocardiographic Contrast
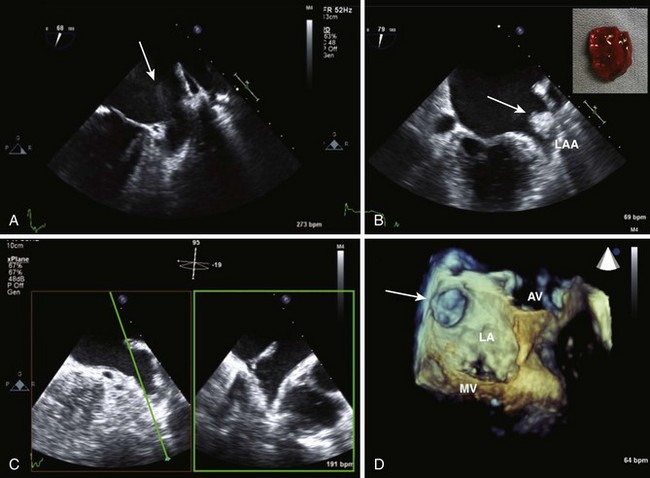
• Dense swirling pattern seen in situations of low-flow states resembling smoke (Figure 10-2A) (see Case 10-4 on the Expert Consult website).
Left Atrium
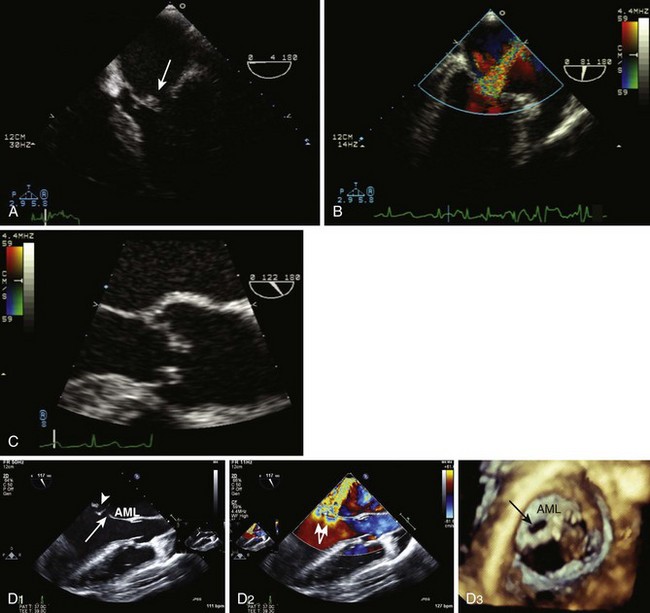
• Thrombi present as irregular masses of variable echogenicity that move with the underlying structure.
• LAA must be carefully assessed in the presence of mitral stenosis, LA enlargement, and stagnant flow with spontaneous echocontrast.
• LAA PW Doppler has a typical biphasic trace. A peak velocity less than 40 cm/s indicates a low-flow risk of thrombus formation.
Left Ventricle
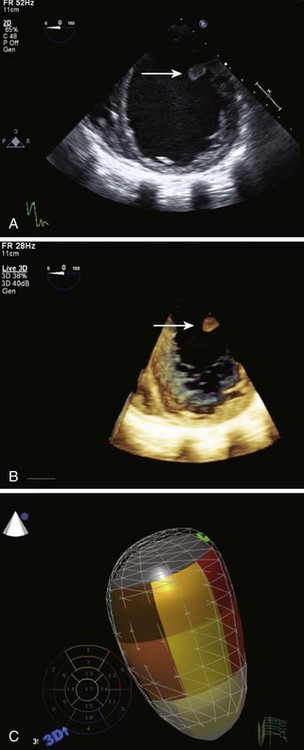
• LV thrombi coexist with left ventricular wall motion abnormalities, LV dilatation (Figure 10-3C), and aneurysm.
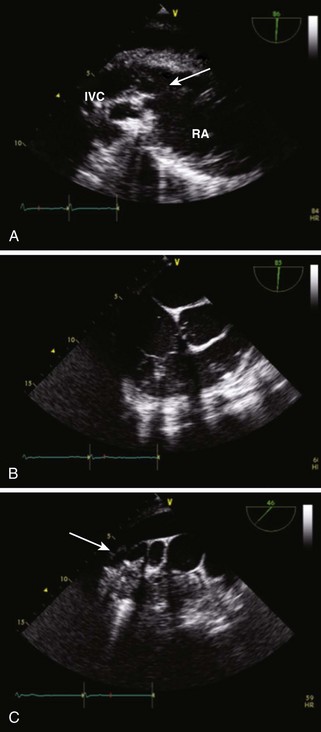
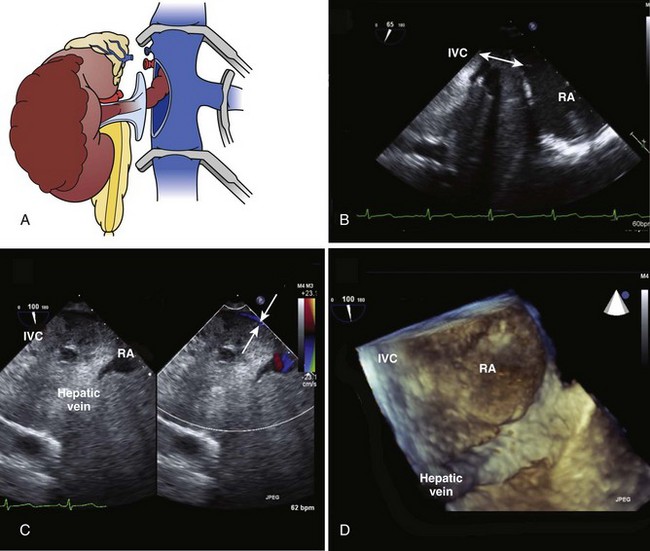
Inferior Vena Cava, Right Atrium, Right Ventricle
• Seen in the RA in the presence of venous thromboembolism and pulmonary embolism (Figure 10-4B) (see Case 10-3 on the Expert Consult website).
• RA thrombi can cross a PFO and result in systemic embolism (see Case 10-3 on the Expert Consult website).
• TEE can visualize the right PA and the proximal left PA; the distal left PA is usually obscured by the left mainstem bronchus.
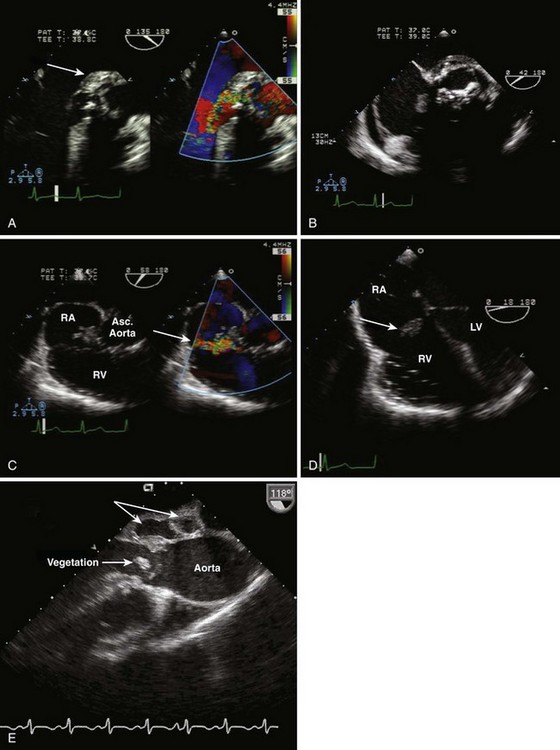
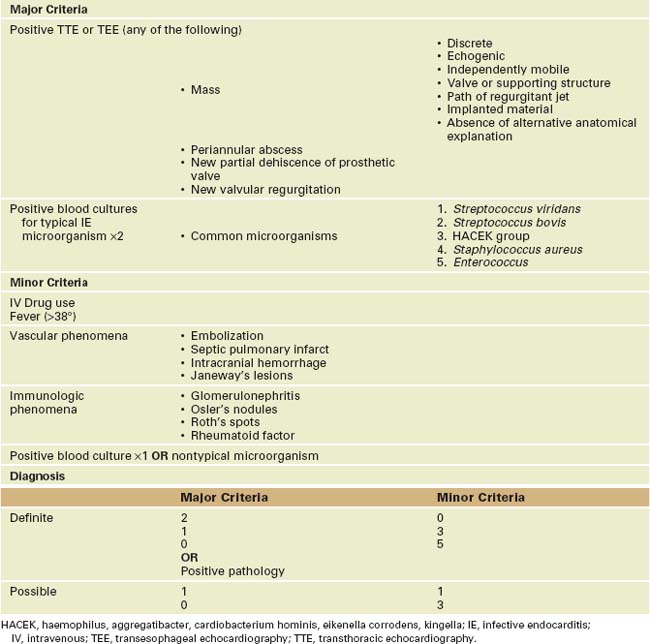
Infective Endocarditis
• The diagnosis is based on clinical and echocardiographic data according to the modified Duke Criteria (Table 10-3).
• TEE is also indicated in patients with prosthetic valves or elderly patients with valve abnormalities.
• Advanced forms of IE result in abscess and fistulae, especially when the aortic valve is involved.
• A form of noninfective endocarditis is marantic endocarditis. It may be observed in patients with adenocarcinoma and antiphospholipid syndrome. Lesions are very difficult to differentiate from IE.
TABLE 10-3 MODIFIED DUKE CRITERIA
Vegetations
Aortic Valve
• Common evolution is aortic root abscess (see Figure 10-6A and E) and invasion of the intervalvular fibrosa.
• In case of aortic regurgitation, vegetations may also be found on the chordae tendinae and the anterior MV leaflet.
• IE on the AV can result in leaflet perforation and aortic regurgitation and are at high risk of embolization.
• Assessment of the AV is performed on multiple views. Zoom is used to better assess the AV leaflets.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree