Class 1
Nonsignificant
Small < 10 mm thick on decubitus CXR
No thoracentesis needed
Class 2
Typical parapneumonic
> 10 mm thick
Glucose > 40 mg/dl, pH > 7.20
LDH < 3 x upper limit normal for serum
Gram stain and culture negative
Class 3
Borderline complicated
7.0 < pH < 7.20 and/or
LDH > 3 x upper limit normal and glucose > 40 mg/dl
Gram stain and culture negative
Class 4
Simple complicated
pH < 7.0 or glucose < 40 mg/dl or
Gram stain or culture positive
Not loculated, not frank pus
Class 5
Complex complicated
pH < 7.0 and/or glucose < 40 mg/dl or
Gram stain or culture positive
Multiloculated
Class 6
Simple empyema
Frank pus
Single locule or free flowing
Class 7
Complex empyema
Frank pus
Multiple loculations
In 2000, the American College of Chest Physicians (ACCP) published an evidence-based guideline on the medical and surgical treatment of parapneumonic effusions. The panel categorized patients with a parapneumonic effusion according to their risk for a poor outcome, and management recommendations were made accordingly. The risk for a poor outcome was established based on three criteria: pleural space anatomy, pleural fluid bacteriology, and pleural fluid chemistry. In all but minimal pleural effusions (<10 mm thickness), pleural fluid analysis is necessary to adequately categorize the effusion. Four categories of risk were defined, as shown in Table 63.2, and thoracic drainage was recommended for category 3 and 4 parapneumonic effusions.
Table 63.2
Categorization of the risk of poor outcome in patients with parapneumonic effusion
Pleural space anatomy | Pleural fluid bacteriology | Pleural fluid chemistry | Category | Risk of poor outcome | Drainage | |||||
|---|---|---|---|---|---|---|---|---|---|---|
A0 | Minimal, free-flowing effusion (< 10 mm on lateral decubitus) | AND | Bx | Culture and Gram stain results unknown | AND | Cx | pH unknown | 1 | Very low | No |
A1 | Small to moderate free-flowing effusion (> 10 mm and < ½ hemithorax) | AND | B0 | Negative culture and Gram stain | AND | C0 | pH ≥ 7.20 | 2 | Low | No |
A2 | Large, free-flowing effusion (≥ ½ hemithorax), loculated effusion, or effusion with thickened parietal pleura | OR | B1 | Positive culture or Gram stain | OR | C1 | pH < 7.20 | 3 | Moderate | Yes |
B2 | Pus | 4 | High | Yes |
Antimicrobial Therapy
Prompt and appropriate antibiotic therapy is an essential component of the management of parapneumonic effusions and empyema. Antibiotic selection should be guided by blood and pleural fluid culture and sensitivity results, when positive. The inoculation of pleural fluid samples into blood culture bottles has been shown to increase the yield of pleural fluid cultures. Nevertheless, pleural fluid cultures remain negative in approximately 40% of complicated parapneumonic effusions.
The bacteriology of pleural infection differs from that of isolated pneumonia, and antibiotics should be selected accordingly. The microbiological data from the First Multicenter Intrapleural Sepsis Trial (MIST1) was recently published. This constitutes the largest single cohort of well-defined bacteriology in complicated parapneumonic effusions and empyema. The authors used amplification and sequencing of bacterial ribosomal RNA in addition to standard cultures. Streptococcal species, including S pneumonia and the S milleri group, were the most frequent isolates in community-acquired pleural infection, accounting for over 50% of the culture positive cases. Anaerobes were identified in 20% of community-acquired infections, and coinfection with aerobes was frequently observed. In contrast, hospital-acquired pleural infection was dominated by Staphylococcus, Gram-negative organisms (Enterobacteriaceae, Pseudomonas) and Enterococcus species. A quarter of the hospital-acquired isolates were methicillin-resistant Staphylococcus aureus (MRSA).
The MIST1 microbiological data has important implications for the empiric antibiotic selection in patients with complicated parapneumonic effusions and empyema. Antibiotic regimens for the management of community versus hospital-acquired pleural infection are proposed in Table 63.3. Anaerobic coverage is recommended for all patients with parapneumonic effusions. Adding a macrolide is unnecessary given the low prevalence of “atypical” pathogens in pleural infection. Aminoglycosides demonstrate reduced pleural space penetration and should be avoided. Evidence is lacking to guide the duration of treatment for pleural infection. Antibiotics should be continued for at least 3 weeks, and a prolonged course may be necessary.
Table 63.3
Proposed empirical antibiotic regimens for pleural infection
Primary regimen | Alternative regimen | |
|---|---|---|
Community-acquired infection | ||
Intravenous | Third-generation cephalosporin (cefotaxime or ceftriaxone) + clindamycin or antipseudomonal penicillin/β-lactamase inhibitor | Imipenem or meropenem |
Oral | Amoxicillin/clavulanate | Clindamycin/ciprofloxacin |
Hospital-acquired infection | ||
Intravenous | Antipseudomonal penicillin/β-lactamase inhibitor + vancomycin | Imipenem or meropenem + vancomycin |
Pleural Fluid Drainage
Pleural fluid analysis is central to the evaluation of parapneumonic effusions. Clinical characteristics cannot be used to predict which patients will require invasive procedures for resolution of the pleural infection. The estimated 10% of patients with parapneumonic effusions who require chest tube drainage must be identified and treated promptly, as a free-flowing effusion may become loculated and difficult to drain over a period of 12–24 h. The importance of timing is reflected in the adage “the sun should never set on a parapneumonic effusion.”
Chest tube drainage is required in all patients with empyema, defined as purulent pleural fluid. The presence of organisms on pleural fluid Gram stain or culture also warrants prompt drainage of the infected fluid. A pleural fluid pH < 7.2 is an indication for chest tube drainage in patients with suspected pleural infection. This threshold identifies a non-purulent parapneumonic effusion as “complicated.” An unfavorable clinical evolution during treatment with antibiotics alone (following an initial aspiration suggestive of a simple parapneumonic effusion) should prompt patient review, repeat pleural fluid sampling, and probably chest tube drainage.
The pleural fluid pH should be measured using a blood gas analyzer and not a pH meter or pH indicator strips, which are unreliable. The pH value should be interpreted within the clinical context and if discordant repeat aspiration should be considered. In a small series of patients, variation in the pleural fluid pH was noted when separate fluid locules were sampled using ultrasound guidance.
The ACCP panel recommended thoracic drainage in all patients with parapneumonic effusions at moderate or high risk of poor outcome, based on their proposed classification. The drainage method was not specified, with therapeutic thoracentesis or tube thoracostomy being proposed as initial interventions. Beyond pleural fluid bacteriology and pH, the following features suggest thoracic drainage is necessary: large effusions, the presence of loculations, and thickened parietal pleura on contrast-enhanced CT scan. Drainage of large collections may be indicated simply for symptomatic relief, but is frequently limited by the presence of loculations. The British Thoracic Society (BTS) guidelines on the management of pleural infection in adults were recently updated, and similar indications for chest tube drainage were proposed.
An algorithm for the management of patients with parapneumonic effusions and empyema is proposed in Fig. 63.1. Pleural fluid aspiration identifies the subset of patients with parapneumonic effusions who require chest tube drainage. This initial thoracentesis may be performed with diagnostic and therapeutic intents. If all pleural fluid is removed with the initial aspiration and no fluid re-accumulates, then no further intervention may be required regardless of the fluid characteristics. Successful treatment of complicated parapneumonic effusions and empyema with serial therapeutic thoracentesis has been reported by various authors, although this approach has received relatively little consideration. No randomized controlled trial has compared serial therapeutic thoracentesis with tube thoracostomy.
Fig. 63.1
Algorithm for the management of patients with parapneumonic effusions and empyema (adapted from RLight chapter and BTS 2010 guideline)
No consensus exists on the chest tube size that should be used for drainage of complicated parapneumonic effusions and empyema. Large-bore chest tubes (28–36 Fr) were traditionally recommended, due to concerns that thick pleural fluid would obstruct smaller drains. However, recent data suggests that smaller pleural catheters (10–14 Fr) may be adequate in most cases of pleural infection and are better tolerated by patients. No randomized trial has compared small versus large-bore chest tubes for the management of pleural infection. A subgroup analysis of the MIST1 trial showed no difference in efficacy between large-bore and small-bore drains. The smaller chest tubes should be managed with regular saline irrigation to maintain catheter patency. The application of suction (−20 cm H2O) may improve drainage and is frequently employed.
Accurate catheter placement may be more important to successful pleural fluid drainage than chest tube size. The BTS guidelines recommend that chest tube insertion be performed under image guidance whenever possible. The PA and lateral chest radiographs may be the first investigation to suggest the presence of a pleural effusion, but thoracic ultrasound allows exact localization of the fluid. Ultrasound can detect small amounts of pleural fluid and identify fluid septations (Fig. 63.2). Ultrasound guidance for pleural procedures is expected to become standard of care, as it improves the safety and accuracy of the initial thoracentesis, and can guide chest tube placement.


Fig. 63.2
Ultrasound appearance of a multiloculated empyema. Multiple septations and thickening of the visceral pleura are visualized
Clinical and radiographic improvement should be observed within 24 h of successful chest tube drainage. Poor clinical progress may be due to incomplete fluid drainage or inadequate antibiotic coverage. In this context, culture results should be reviewed, and a CT scan of the chest obtained to delineate the infected pleural space. Contrast-enhanced CT scan (performed in the tissue phase) will identify visceral pleural thickening, pleural fluid loculations, and the chest tube position (Fig. 63.3). Significant residual fluid collections may be amenable to drainage with additional chest tubes, inserted under image guidance. In contrast, proceeding directly to VATS with lysis of adhesions should be considered in the presence of multiple fluid locules.
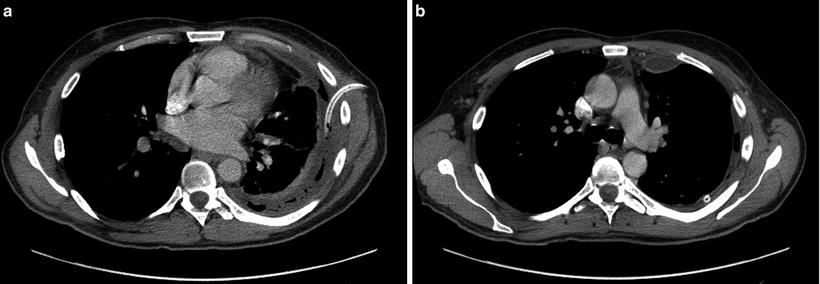
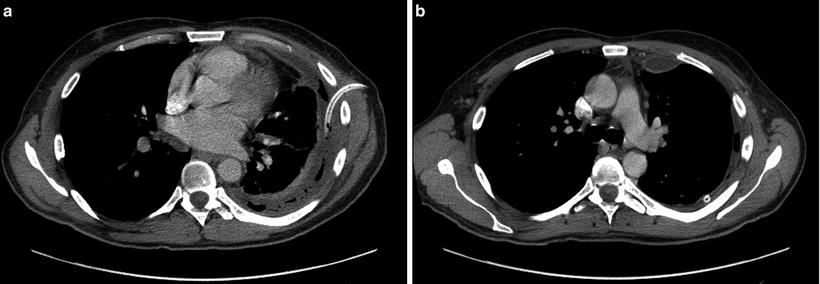
Fig. 63.3
Contrast-enhanced CT scan images of an empyema, following initial insertion of a 16-Fr chest tube by Seldinger technique (a). There is thickening and enhancement of both the visceral and parietal pleural surfaces (split-pleura sign, b)
Chest tube removal is appropriate once imaging confirms successful pleural fluid drainage, and the clinical evolution is consistent with resolution of pleural sepsis. Chest tubes are generally left in place until the volume of drainage decreases to less than 50 ml per 24 h. A chest tube that ceases to function should be promptly removed, as it then simply becomes a conduit for infection.
Specialist Referral and General Medical Care
A respiratory physician should be involved in the care of any patient who requires chest tube drainage. Involvement of thoracic surgery when the patient does not respond to initial drainage is recommended. Delayed specialist referral of patients with pleural infection has been identified as a factor that is associated with increased morbidity.
Adequate nutritional support was advocated by the Empyema Commission of 1918. This aspect of patient care should not be neglected. Hypoalbuminemia has been found to correlate with mortality in patients hospitalized for empyema.
Finally, thrombosis prophylaxis should proceed according to current recommendations. The most recent ACCP guidelines on the prevention of venous thromboembolism (8th edition) recommend prophylaxis with low molecular weight heparin or low-dose unfractionated heparin in the absence of any contraindications.
Predictors of Clinical Outcome
Patients with complicated parapneumonic effusions may require invasive surgical procedures for resolution of the pleural infection. Though early identification of the subset of patients who will fail initial management with antibiotics and tube thoracostomy would be very helpful, attempts at finding predictors of outcome in patients with complicated parapneumonic effusions and empyema have been disappointing.
A retrospective review of patients with complicated parapneumonic effusion or empyema identified loculation and (counterintuitively) low pleural fluid leukocyte count as independent predictors of failure of tube thoracostomy. CT and ultrasound have established roles in the investigation of parapneumonic effusions and facilitate pleural fluid drainage. Kearney et al. questioned whether ultrasound (fluid hyperechogenicity, septations) or CT features (pleural thickening, thickening of extrapleural fat) would predict the effusion stage or need for surgical treatment. Unfortunately, neither technique reliably identified the patients who subsequently required surgical intervention.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


