Management of Sleep-Disordered Breathing
Puja Kohli
Richard Schwab
Atul Malhotra
Obstructive sleep apnea is a common disorder with major neurocognitive and cardiovascular sequelae (1). Despite advances in the treatment of sleep apnea, further work is clearly required in this area (2). The existing therapies have efficacy, but can be poorly tolerated and in some cases work in only a subgroup of patients. In this chapter, we will review the evidence underlying various therapies and highlight the potential avenues for future advances.
POSITIVE AIRWAY PRESSURE THERAPY
For many years, the only treatment available to patients with obstructive sleep apnea (OSA) was surgical bypass of the obstructed airway (i.e., tracheostomy) (3,4). This situation changed with the development of positive airway pressure (PAP) therapy (5), which quickly gained acceptance due to its noninvasive nature (6). Although nasal continuous positive airway pressure (CPAP) is not tolerated by all afflicted individuals (7), it remains the treatment of choice for OSA as of today (8).
Mechanism of Action
In OSA, the upper airway collapses due to an imbalance in the forces that usually keep the airway open (9,10). The airway lumen in OSA patients is often smaller and more collapsible than in matched controls due to structural abnormalities and/or soft tissue properties in the airway walls (11, 12, 13 and 14). Also, end-expiratory lung volume can have a tethering effect on the human upper airway (15, 16 and 17), and this force may be reduced in OSA patients particularly in those with abdominal obesity (18,19). While normally during wakefulness the airway dilator muscles keep the airway open against these collapsing influences (20), during sleep neural drive to the muscles decreases causing relaxation and subsequent airway closure among those anatomically predisposed (21,22). The pharyngeal airway closes when the transmural pressure (i.e., pressure inside the airway minus pressure outside the airway) is negative, that is tissue pressure surrounding the airway exceeds the pressure within the airway itself (23,24). Thus, PAP is used to increase the airway pressure (and the pharyngeal transmural pressure) to prevent pharyngeal collapse (Figure 8.1).
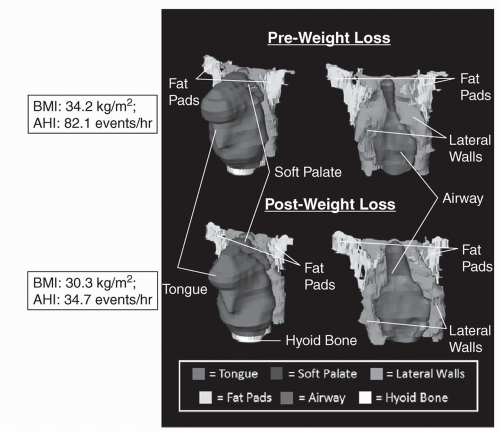
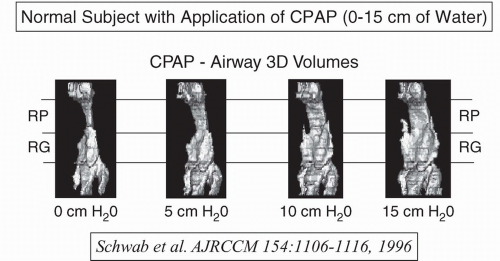
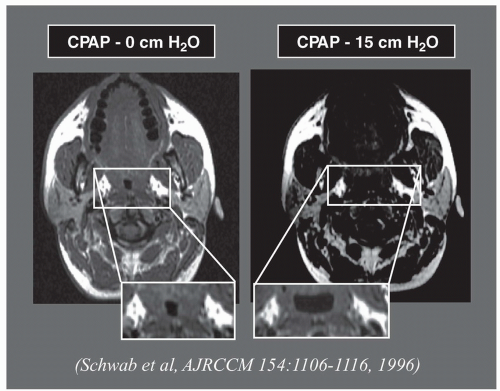
There are multiple mechanisms that may explain how PAP maintains airway patency. Magnetic resonance imaging (MRI) studies show increases in the entire airway volume and area with applied pressure, confirming the use of PAP as a “pneumatic splint” (12) (Figure 8.2). Other imaging studies reveal that PAP reduces lateral pharyngeal wall thickness and may decrease airway edema (25) (Figures 8.3 and 8.4). Furthermore, studies also show that PAP increases endexpiratory lung volume (26, 27 and 28), likely through direct mechanical influences. In humans genioglossal activity is reduced with increases in lung volume, suggesting that the airway is being stabilized through mechanical effects rather than through neuromuscular reflexes (29).
Various modes of PAP are available for treatment (Table 8.1). PAP therapy has been shown to improve sleepiness and blood pressure in OSA (6,30, 31 and 32), and is regarded as the treatment of choice for OSA. At present, there is minimal evidence supporting more expensive forms of PAP therapy (33). However, in certain patients, these newer modes may be beneficial and therefore treatment should be individualized in such cases.
Modes and Indications
Continuous positive airway pressure (CPAP): A CPAP machine delivers airflow that maintains a constant servo-controlled pressure during both inspiration and expiration. The level of pressure is generally set based on an in-laboratory titration to eliminate obstructive events and snoring in all stages of sleep and positions. However, autotitration devices are sometimes used to determine the optimal pressure. Nasal CPAP is generally considered first line-therapy for most patients with OSA.
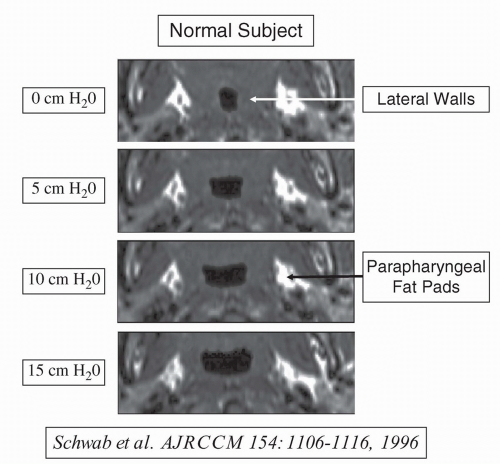
FIGURE 8.4 Axial retropalatal magnetic resonance imaging (MRI) in a normal subject (the same subject as in Figure 8.3) at baseline and with continuous positive airway pressure (CPAP) up to 15 cm H2O. Note the lateral airway enlargement with progressive increases in CPAP which results in thinning of the lateral pharyngeal walls but the parapharyngeal fat pads are not displaced. The increase in airway size with greater levels of CPAP is primarily in the lateral dimension; the anteriorposterior dimension of the airway does not change significantly with CPAP. (From Reference 25 with permission.)
TABLE 8.1 Mechanisms of PAP Therapies
Positive Airway Pressure Therapy
Mechanism
CPAP
Maintains the same pressure during inspiration and expiration
BiPAP
Independent adjustment of inspiratory and expiratory pressures
APAP
Maintains the same pressure during inspiration and expiration but the pressure level varies to the lowest pressure that keeps the airway open
Pressure relief systems
Lowers the applied pressure during early exhalation while maintaining the pressure at end-exhalation
ASV
Maintains low baseline pressure and then adds varying ventilatory support to maintain a preset level of ventilation for each breath
Combination device (i.e. auto level BiPAP)
Varies both the inspiratory and expiratory pressure levels to overcome the obstruction at the lowest possible pressure
Bilevel positive airway pressure (bilevel PAP): Bilevel PAP allows independent adjustment of inspiratory and expiratory pressures (34). Some patients, specifically those with expiratory pressure discomfort, feel more comfortable when breathing out against lower pressure and therefore prefer bilevel PAP over CPAP. Randomized trials, however, have not shown a difference in treatment adherence between the two modes (35). Bilevel PAP has a number of modes, including S (spontaneous), T (timed), and ST (spontaneous-timed). These modes can be used in patients with various disorders to support ventilation. For example, a back-up rate can be quite useful in treating patients with neuromuscular disease or in certain forms of central apnea (36). For most OSA patients, the S mode is generally adequate (if bilevel is being used rather than CPAP).
Pressure-relief systems: Industry has developed various techniques to attempt to make CPAP more comfortable. The concept underlying these methods is that collapse of the airway tends to occur at end-exhalation, whereas the discomfort experienced by patients is frequently during early exhalation. As a result, these devices attempt to lower the applied pressure during early exhalation while maintaining the pressure at end-exhalation. Data are still emerging regarding the efficacy of this approach, but some data do support this methodology (37, 38 and 39). While some laboratories are now preferentially using these devices rather than CPAP, further data and economic analyses will likely be required for their use to become standard of care.
Automatically titrating positive airway pressure (APAP): Autotitrating CPAP devices maintain the same pressure during inspiration and expiration. However, the applied pressure level varies throughout the night to maintain the lowest pressure that keeps the airway open. Various companies have used different approaches to define airway compromise (e.g., flow limitation, snoring, vibration). Automatic PAP can be used in two major ways. First, the device can be used to determine the therapeutic CPAP level for patients who will ultimately receive long-term CPAP therapy. For example, patients who undergo home sleep testing who are diagnosed with OSA might undergo an autotitration study to determine the appropriate CPAP settings. Second, some practitioners use autotitration devices for long-term therapy of OSA patients. The average airway pressure using APAP is lower than on CPAP because the machine decreases the delivered pressure in sleep stages or positions that do not require as much pressure (33). However, most randomized trials have not shown systematic benefit to automatic PAP over standard CPAP. This mode may be helpful in patients who need continual adjustment of their pressures (so-called moving targets), such as those experiencing weight loss following bariatric surgery. In addition, there may be subgroups of patients with highly variable pressure requirements (e.g., high pressure requirements primarily during REM sleep or during supine sleep) in whom these devices are more likely to be beneficial than in standard OSA patients. However, further data are required before definitive recommendations can be provided.
Adaptive seroventilation (ASV): Adaptive seroventilation provides a low baseline pressure and then adds varying ventilatory support to maintain a preset level of ventilation for each breath (40). Therefore, with this mode, if a patient’s effort decreases, the machine’s inspiratory support increases to maintain a steady level of ventilation. This mode has been proposed as a method for treating some patients with central sleep apnea or in certain patients who have OSA refractory to standard CPAP. Some authors have used the term complex sleep apnea to refer to patients with OSA who develop central sleep apnea on initiation of CPAP (41) These patients with
so-called treatment-emergent central apnea generally experience spontaneous resolution of their disease with ongoing therapy (42,43). Thus, the use of expensive newer devices for these patients will require outcome data before their use can be justified. The use of these newer devices for Cheyne-Stokes breathing is now being actively investigated, the results of which we eagerly await (36,44).
Combination device. The various modes listed above have been combined in various ways to optimize patient comfort. Automatically titrating bilevel positive airway pressure (auto bilevel PAP) devices vary both the inspiratory and expiratory pressure levels to overcome the obstruction at the lowest possible pressure while maximizing comfort. Bi-flex devices have been used to optimize comfort by employing the pressure relief strategies discussed above with bilevel devices. Bi-flex with auto uses a combined approach of bi-level PAP with “flex” to provide pressure relief along with autotitration to vary the pressure according to physiologic demands.
As definitive roles for each of these modes remains to be established, clinicians often start with CPAP and then change to an alternative mode in an attempt to improve adherence as required. However, further work is required to define the optimal rescue strategy.
Effectiveness
Obstructive Sleep Apnea
Positive airway pressure therapy improves adverse outcomes of sleep-disordered breathing. Randomized trials have found that treatment with therapeutic CPAP improves sleepiness and increases vigilance, productivity, and quality of life when compared to sham CPAP (45). PAP therapy confers sustainable long-term benefits as well, regardless of the severity of the OSA. For instance, Munoz and colleagues demonstrated that patients with OSA sustained an improvement in daytime alertness over an entire year of observation (46). In addition, studies with patients with only mild OSA show that treatment with CPAP improves symptoms such as breathing pauses, choking, morning headache, and concentration difficulties (7,47).
Automobile accidents are a significant contributor to the adverse outcomes in patients with OSA. Findley et al. (48,49) found that patients with OSA have worse driving performance and make more mistakes than controls without OSA. Treatment with CPAP has been found to improve performance (50), and improves steering control and reaction time (51). CPAP has also been found to reduce accident rates, which are three to seven times higher for patients with OSA (52).
PAP treatment for OSA likely also significantly improves cardiovascular outcomes in patients with hypertension, congestive heart failure, and stroke. Data from the Sleep Heart Health Study and the Wisconsin Sleep Cohort have shown that the risk of developing hypertension is not only related to the presence of OSA, but also increases with the severity of the OSA (53,54). A subsequent study performed by Becker et al. (30) found that after only 2 months of CPAP treatment, mean blood pressure was reduced in patients with OSA. Another study found that reductions in blood pressure were larger in patients with more severe OSA and in patients with hypertension (31). In addition, patients who are more adherent with CPAP are likely to have the greatest decrease in blood pressure (55). However, randomized trial data are currently lacking with regards to CPAP yielding improved cardiovascular outcomes. A number of studies are underway that are seeking to test the hypothesis that nasal CPAP therapy reduces the frequency of hard cardiovascular outcomes (such as myocardial infarction, congestive heart failure, and stroke). At present, the level of evidence is primarily from observational cohort studies in which nasal CPAP-treated patients have improved outcome as compared with
untreated controls (56). Such studies are encouraging, but leave open the question as to whether use of CPAP is simply a marker of a healthy participant (57). That is, considerable literature exists showing that adherent patients have an improved outcome as compared with nonadherent ones, even when examining individuals taking placebo. The implication of this finding is that adherent behavior is a marker of improved outcome, likely due to more educated patients, with greater motivation than nonadherent controls. Indeed, Platt et al. (57) have shown that the use of statins is markedly greater among CPAP-treated patients than among controls, suggesting that CPAP therapy may be a marker of a good prognosis. As a result, randomized trials will be required to draw any definitive conclusions. However, randomized trials have considerable ethical barriers, given the need to leave symptomatic patients untreated for years while waiting for cardiovascular events to occur (8). On the other hand, asymptomatic patients are unlikely to be adherent with therapy for extended periods of time. Thus, conclusive data regarding the utility of CPAP in preventing cardiovascular events may be difficult to obtain.
untreated controls (56). Such studies are encouraging, but leave open the question as to whether use of CPAP is simply a marker of a healthy participant (57). That is, considerable literature exists showing that adherent patients have an improved outcome as compared with nonadherent ones, even when examining individuals taking placebo. The implication of this finding is that adherent behavior is a marker of improved outcome, likely due to more educated patients, with greater motivation than nonadherent controls. Indeed, Platt et al. (57) have shown that the use of statins is markedly greater among CPAP-treated patients than among controls, suggesting that CPAP therapy may be a marker of a good prognosis. As a result, randomized trials will be required to draw any definitive conclusions. However, randomized trials have considerable ethical barriers, given the need to leave symptomatic patients untreated for years while waiting for cardiovascular events to occur (8). On the other hand, asymptomatic patients are unlikely to be adherent with therapy for extended periods of time. Thus, conclusive data regarding the utility of CPAP in preventing cardiovascular events may be difficult to obtain.
Finally, OSA has been found to increase the risk of stroke in patients with mild, moderate, and severe OSA in addition to elderly patients with OSA (58,59). A study by Marin and colleagues found that OSA patients treated with CPAP had fewer vascular events, including stroke and death, compared to those who were untreated (56). These data support the use of CPAP in high-risk patients to prevent stroke; however, more data are needed to provide definitive proof.
Congestive Heart Failure
Sleep-disordered breathing is common in patients with congestive heart failure. About one-third of these patients have predominantly central sleep apnea (CSA) and roughly one-third have predominantly OSA (60).
Treatment of OSA with CPAP in patients with congestive heart failure (CHF) has been shown to improve ejection fraction and New York Heart Association functional class (61, 62 and 63). In addition, Kaneko et al. (62) found that treatment in these patients reduces blood pressure and improves sleepiness and quality of life. The findings of the Kaneko paper were somewhat controversial due to a relatively small sample size and unexpected findings in the hemodynamic data (reduced left ventricular end-diastolic dimension despite increased left ventricular end-diastolic volume in CHF patients given CPAP). However, the findings of the Kaneko paper were corroborated by Mansfield et al. (63), who observed improvements in cardiac function with 3 months of CPAP therapy in people with OSA plus CHF. Th us, the existing data are from small studies, but would support the use of CPAP in people with OSA plus CHF, although hard outcome data are still lacking.
Patients with CHF and CSA suffer from a cycle of apneas alternating with arousals and hyperventilation that is seen in Cheyne-Stokes respirations (CSR). Optimization of medical therapy is the cornerstone of treatment in these patients, as studies have shown resolution of CSR with appropriate dosing of cardiac medications (64). The role of CPAP in these patients is less clear. Early studies suggested that treatment of CSA with CPAP in patients with heart failure was beneficial. Patients treated with CPAP had improvement of ejection fraction (65, 66, 67 and 68), decreased need for cardiac transplantation, and improved exercise tolerance (69,70)




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree