Fig. 11.1
Left intrathoracic carotid artery secondary to gunshot wound
The majority of carotid artery injuries are confined to the common carotid artery. According to the literature, the carotid artery segment that most frequently is involved is the common carotid (73 %), followed by the internal carotid (22 %), and finally the external carotid (5 %) [16].
For the operative management of carotid artery injury, the patient should be placed in supine position on the operating table with the head facing the contralateral side of the injury. The face, neck, supraclavicular area, and thoracic area must be included in the operating field. The contralateral groin should be also prepared in case a saphenous vein graft is needed to repair the carotid injury. The neck should be explored by a standard incision in the anterior border of the sternocleidomastoid (SCM) muscle, from the angle of the mandible up to the sternoclavicular junction (Fig. 11.2). Below the SCM muscle the internal jugular vein can be found. Medially deeper to it, the carotid artery can be found. The facial vein is usually transected in order to expose the common carotid bifurcation. Once exposed it is essential to obtain proximal and distal control of the common, internal, and external sections of the carotid artery.
If the injury is possible for primary repair, lateral arteriorrhaphy should be attempted. However, in injuries that produced extensive destruction of the carotid artery, resection of the involved segment should be done followed by reconstruction of the artery. End-to-end primary anastomosis can be done (Fig. 11.3) if there is no sign of tension. If this occurs, the interposition of a saphenous vein graft should be performed (Fig. 11.4). As an option, instead of a saphenous vein graft, a PTFE graft can be used in order to restore blood flow. Doppler signal analysis should be performed after the repair is complete (Fig. 11.5). The use of 5,000 units of heparin systematically is recommended in this type of injuries [16].
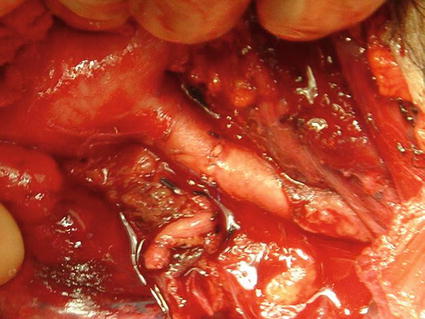
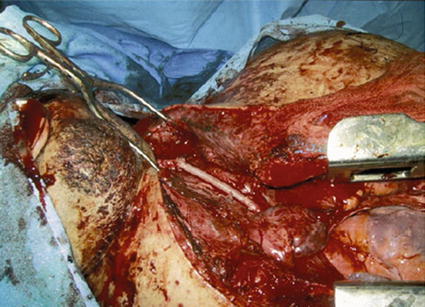
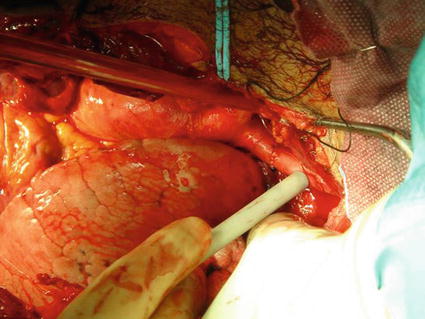
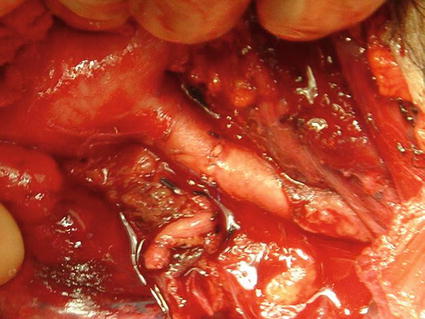
Fig. 11.3
Primary repair performing end-to-end anastomosis
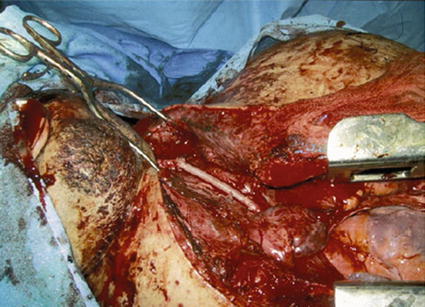
Fig. 11.4
Carotid repair with autogenous saphenous vein
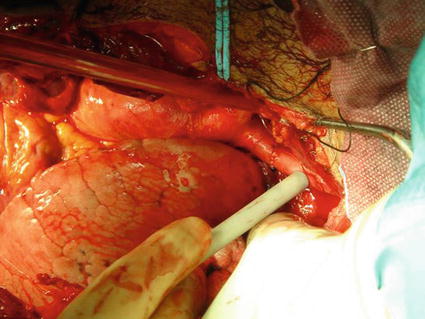
Fig. 11.5
Pulse checked by a handheld Doppler probe
11.6.2 Vertebral Artery Injuries
Vertebral artery injuries are uncommon and usually they are not life-threatening. The incidence of these injuries varies from 1 % up to 7.4 % [17]. The most common mechanisms of injuries are gunshot wounds, followed by stab wounds. These injuries are often associated to other injuries such as aerodigestive injuries, cervical spine, nerve injuries, and other vascular injuries. According to Rowe et al., associated vascular injuries occur in a range from 13 to 19 % [17].
The vast majority of vertebral artery injuries does not require any treatment or are treated with angiography. The operative management of these injuries is reserved for patients with active bleeding or those that angiographic treatment had failed. Proximal vascular control of the vertebral artery can be achieved at the base of the neck where it comes off the subclavian artery. This approach requires a supraclavicular incision followed by transection of the SCM muscle off the clavicle. By retracting the subclavian vein caudally and the anterior scalene muscle laterally, the vertebral artery can be found in the superior and posterior aspect of the ascending subclavian artery. The interosseous portion of the vertebral artery is achieved by a standard cervical incision like in carotid artery injuries. The longus colli muscle is found deep in the neck and should be removed from the bony structures. The anterior rim of the vertebral foramen must be removed in order to expose the vertebral artery. The vertebral artery can be safely ligated without major complications. Special care must be taken in order to avoid injury to the nerves. It is important to remark that the preferred approach of these injuries is angiographically.
11.6.3 Laryngotracheal Injuries
Laryngotracheal injuries are uncommon injuries. They are present in 1/30,000 emergency room visits. In penetrating neck injuries the incidence of laryngotracheal injury varies between 2 and 4 % [17]. The management of these injuries varies from nonoperative management up to operative management, but most of these injuries are beneficiated with early operative intervention. Besides hemodynamic support, oxygenation and ventilation of these patients are important.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree