The aim of the present study was to evaluate the prevalence and correlates of right ventricular (RV) noncompaction (RVNC), RV systolic dysfunction, and RV myocardial fibrosis in patients with isolated left ventricular (LV) noncompaction (LVNC). For this purpose, cine and contrast-enhanced cardiac magnetic resonance imaging (MRI) was used. A total of 56 consecutive patients with isolated LVNC were included in the study. The diagnosis of isolated LVNC was based on the presence of standard cardiac MRI and clinical criteria. For each patient, cine and contrast-enhanced cardiac MR images were analyzed to evaluate the prevalence and correlates of RVNC, RV dysfunction, and late gadolinium enhancement (a surrogate of myocardial fibrosis) involving the RV. Mean age of the patient population was 45 ± 19 years; 35 patients (63%) were men. RVNC was observed in 5 patients (9%). Impaired RV systolic function was observed in 9 patients (16%). Late gadolinium enhancement was not observed in any RV segment. No association was found between wall motion abnormalities and noncompaction at RV segmental level (φ coefficient 0.041, p = 0.26). At multivariate analysis, LV ejection fraction was the only variable independently related to RV ejection fraction (β = 0.62, p <0.001). In conclusion, RV systolic dysfunction is present in a non-negligible proportion of patients with isolated LVNC; LV systolic function is the only variable independently related to RV systolic function.
Prominent trabeculations and deep intertrabecular recesses within the left ventricular (LV) wall in the absence of other associated congenital or acquired heart disease are the main characteristics of isolated left ventricular noncompaction (LVNC) ; these features are believed to be related to an arrest in the normal embryogenesis of the endocardium and myocardium. The use of cardiac magnetic resonance imaging (MRI) is of potential clinical value in patients with isolated LVNC. Its high spatial resolution allows precise evaluation of the thickness of compacted and noncompacted myocardial layers and provides the opportunity to quantify biventricular function parameters with high accuracy and reproducibility. Moreover, contrast-enhanced cardiac magnetic resonance with late gadolinium enhancement (LGE) imaging may detect the area of myocardial fibrosis. Recent cardiac MRI studies have investigated the relation among LV systolic function, the extent of LVNC, and the presence and/or extent of LV myocardial fibrosis in this group of patients. Scarce data are conversely available about the associated involvement of the right ventricle (RV) and the clinical meaning of RV systolic dysfunction in this group of patients. Accordingly, the aim of the present study was to evaluate the prevalence and correlates of RV noncompaction (RVNC), RV systolic dysfunction, and RV myocardial fibrosis in patients with isolated LVNC. For this purpose, cine and contrast-enhanced cardiac MRI was used.
Methods
A total of 56 consecutive patients with isolated LVNC were included in the study. The diagnosis of isolated LVNC was based on the presence of the following cardiac MRI and clinical criteria : (1) visual appearance of 2 distinct myocardial layers (a compacted epicardial layer and a noncompacted endocardial layer); (2) marked trabeculation and deep intertrabecular recesses within the noncompacted layer; (3) noncompacted/compacted end-diastolic myocardial ratio >2.3; and (4) the absence of other associated congenital or acquired heart disease.
The cardiac MRI examinations of these patients were analyzed to evaluate the prevalence and independent correlates of RVNC, RV dysfunction, and RV myocardial fibrosis. Because of the lack of MRI criteria for RVNC, this was considered present when the following criterion derived from previous histopathologic studies was satisfied : the presence of recesses within the inflow area of the RV subjacent to the tricuspid valve involving at least 75% of the RV thickness.
All cardiac MRI studies were performed using a 1.5 T scanner (Signa Hdx, GE Healthcare, Milwaukee, Wisconsin). An 8-element cardiac phased-array receiver surface coil with breath holding in expiration and electrocardiographic gating was used for signal reception. Three standard cine long-axis slices and a stack of contiguous cine short-axis slices from the atrioventricular ring to the apex were acquired using a steady-state free-precession pulse sequence with the following parameters: 30 phases, a slice thickness of 8 mm, no gap, 8 views per segment, number of excitation: 1, field of view of 40 cm, 224 × 224 matrix, 256 × 256 reconstruction matrix, a repetition time of 3.5 ms, an echo time of 1.5 ms, a flip angle of 45°, and a bandwidth of 125 KHz. The LGE images were acquired in end-systole in the same view as that used for cine images 10 minutes after intravenous injection of 0.2 mmol/kg gadolinium-diethyltriaminepentaacetic acid (Magnevist, Bayer Schering Pharma, Germany). A segmented inversion-recovery gradient-echo pulse sequence was used with the following parameters: a slice thickness of 8 mm, no gap, number of excitation: 1, field of view of 40 mm, 224 × 192 matrix, 256 × 256 reconstruction matrix, a repetition time of 4.6 ms, an echo time of 1.3 ms, and a flip angle of 20°. The appropriate inversion time was set to null normal myocardium (range, 250 to 350 ms).
RVNC was determined on cine short-axis slices. First, the RV myocardial segments were visually screened for the presence of deep intertrabecular recesses within the inflow area of the RV subjacent to the tricuspid valve. For this purpose, the Isner classification, dividing the RV into 12 segments (4 basal, 4 midventricular, and 4 apical), was used. Thereafter, the ratio of noncompacted (if present) to compacted myocardium was measured for each RV myocardial segment; RVNC was defined as a ratio of noncompacted to compacted myocardium of ≥3 at end-diastole. Using the same 12-segment model, the dichotomous absence or presence of wall motion abnormalities (WMAs) was visually assessed for each RV myocardial segment. Using a dedicated software (MASS Analysis; Medis, Leiden, the Netherlands), the following functional parameters were obtained from the cine short-axis images: RV and LV end-diastolic volume indexes (LVEDVi), RV and LV end-systolic volume index, LV mass index, and RV and LV ejection fractions (RVEF and LVEF, respectively). The dichotomous presence or absence of RV dysfunction (i.e., reduced RVEF) was assessed; previously published cardiac MRI ranges for normal RVEF were used as reference values. The dichotomous presence or absence of LV LGE was qualitatively determined by reviewing all short- and long-axis contrast-enhanced images; regions of elevated signal intensity had to be confirmed in 2 spatial orientations. The quantitative extent of LV LGE was determined as previously described, using a dedicated software (MASS 6.1). A region of interest was selected in the background of the image; mean signal intensity and SD of the region of interest were measured. The LV myocardium was delimited by endocardial and epicardial contours manually traced. Enhanced myocardium was defined as myocardium with a signal intensity of ≥5 SDs more than the mean of the region of interest. The extent of LGE was expressed as percentage of the LV mass (percent LV LGE). For RV LGE, the signal intensity of LV LGE was taken as the reference; an RV segment was considered as having LGE when the enhanced myocardium involved ≥50% of its circumferential length, as previously suggested. Cine and LGE images were evaluated blindly by 2 independent skilled observers.
Continuous variables are expressed as median and interquartile range. Categorical data are presented as absolute numbers and percentages. Differences in continuous variables were assessed using the Student t test or the Mann-Whitney U test, if appropriate. Chi-square or Fisher’s exact test, if appropriate, were used to assess differences in categorical variables. The φ coefficient was computed to assess the association between the presence of noncompaction and WMA at the RV segmental level. Univariate and multivariate linear regression analyses (using the backward stepwise model selection procedure) were performed to evaluate the relation between RVEF and the following variables: age, gender, LVEDVi, LVEF, LV mass index, number of LV noncompacted segments, percent LV LGE, RV end-diastolic volume index, presence of RVNC, and presence of RV LGE. Only variables with a p value ≤0.1 at univariate analyses were entered as covariates in the multivariate model. Because of the small population size, the multivariate analysis had exploratory nature. A 2-tailed p value <0.05 was considered statistically significant. Statistical analysis was performed using the SPSS software package (SPSS 19.0; SPSS Inc., Chicago, Illinois).
Results
Mean age of the patient population was 45 ± 19 years; 35 patients (63%) were men. RVNC was observed in 5 patients (9%). Overall, 13 RV segments (2%) fulfilled the definition of noncompaction; the median number of RV noncompacted segments per patient having RVNC was 2 (interquartile range 1.5 to 4) and the maximal noncompacted/compacted myocardium ratio was 5.2 (interquartile range 3.3 to 5.4).
Overall, 51 RV segments (8%) showed WMAs; WMAs were similarly observed at the RV basal, mid, and apical levels (18 [35%], 19 [37%], and 14 [28%], respectively). Importantly, no association was found between WMAs and noncompaction at the RV segmental level (φ coefficient 0.041, p = 0.26; Figure 1 ). LGE was not observed in any RV segment.
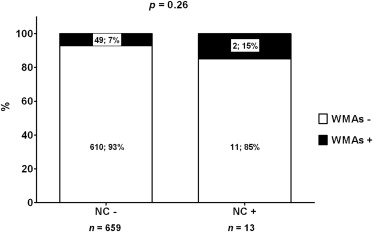
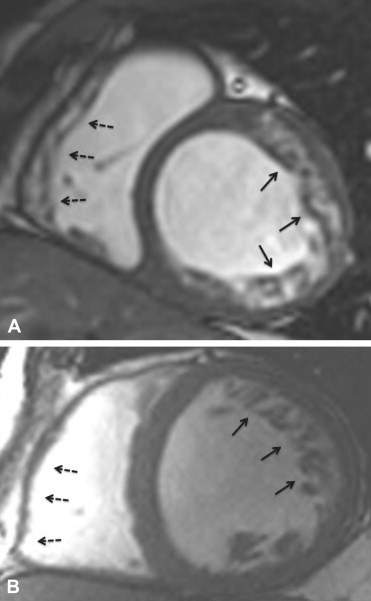
Figure 2 shows cine cardiac MRI of a patient having multiple areas of noncompaction of both LV and RV myocardium and of a patient without RVNC.
Impaired RV systolic function (defined accordingly to previously published cardiac MRI ranges for normal RVEF) was observed in 9 patients (16%). Table 1 lists the main differences between patients with and without reduced RVEF. Patients with impaired RV systolic function had higher LVEDVi, LV end-systolic volume index, and LV mass index (p = 0.076, 0.004, and 0.026, respectively). In addition, they showed lower LVEF, higher prevalence of LV LGE, and larger percent LV LGE (p <0.001, p = 0.026, and p = 0.017, respectively). Of note, no significant difference was observed between the 2 groups regarding the number of LV noncompacted segments and the presence of RVNC.
| Variable | RV Systolic Dysfunction | p | |
|---|---|---|---|
| No (n = 47) | Yes (n = 9) | ||
| Age (yrs) | 43 (25–59) | 57 (43–68) | 0.066 |
| Men | 29 (62) | 6 (67) | 1.00 |
| LVEDVi (ml/m 2 ) | 94 (75–121) | 122 (93–134) | 0.076 |
| LV end-systolic volume index (ml/m 2 ) | 44 (30–66) | 80 (54–93) | 0.004 |
| LVEF (%) | 55 (44–63) | 32 (30–37) | <0.001 |
| LV mass index | 71 (62–86) | 102 (72–104) | 0.026 |
| Number of LV noncompacted segments | 4 (3–5) | 4 (2–5.5) | 0.81 |
| Presence of LV LGE | 21 (45) | 8 (89) | 0.026 |
| Extent of LGE expressed as % of LV mass | 0 (0–5) | 6 (3–15) | 0.017 |
| RV end-diastolic volume index (ml/m 2 ) | 76 (62–91) | 81 (69–96) | 0.40 |
| RV end-systolic volume index (ml/m 2 ) | 25 (20–31) | 47 (37–52) | <0.001 |
| RVEF (%) | 67 (60–73) | 45 (41–51) | <0.001 |
| RVNC | 3 (6) | 2 (22) | 0.18 |
Table 2 lists the results of the univariate and multivariate linear regression analyses performed to determine the independent correlates of RV systolic function. At the univariate analysis, the following variables were significantly related to RVEF: age, LVEDVi, LVEF, LV mass index, and percent LV LGE. At multivariate analysis, only LVEF was independently related to RVEF (β = 0.62, p <0.001). Figure 3 shows the relation between RVEF and LVEF in patients with isolated LVNC.
| Independent Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
| β | p | β | p | |
| Age (yrs) | −0.29 | 0.031 | — | — |
| Men | −0.19 | 0.17 | ||
| LVEDVi | −0.32 | 0.018 | — | — |
| LVEF | 0.62 | <0.001 | 0.62 | <0.001 |
| LV mass index | −0.28 | 0.035 | — | — |
| Number of LV noncompacted segments | 0.11 | 0.42 | ||
| Extent of LGE expressed as % of LV mass | −0.34 | 0.011 | — | — |
| RV end-diastolic volume index | −0.20 | 0.15 | ||
| RVNC | −0.17 | 0.21 | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


