Chapter 75 Lung Transplantation
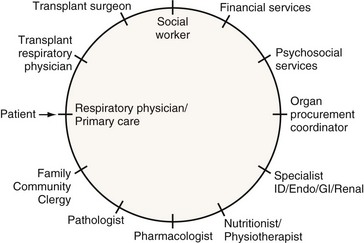
Pulmonary transplantation has become an effective and reliable means to improve survival and quality of life in carefully selected patients with end-stage pulmonary disease. The current success in transplantation is attributed to appropriate referral, early selection, careful evaluation, and improving management of lung allograft donors and recipients. The multidisciplinary approach (Figure 75-1), together with meticulous clinical care of each transplant candidate (including understanding of the underlying disease state and optimization of psychosocial status), is of the utmost importance. The concurrent advances in surgical techniques, combined immunosuppressive regimens, surveillance for rejection and institution of prophylaxis, and early treatment of infection have resulted in the excellent survival rates and quality of life witnessed today.
Current Trends in Lung Transplantation
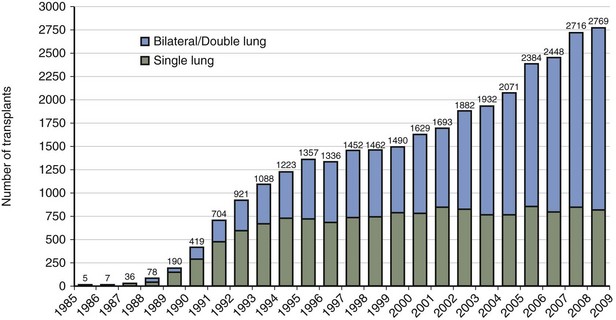
In the United States, the United Network for Organ Sharing (UNOS) has been operating the Organ Procurement and Transplantation Network (OPTN) since 1984. The International Society for Heart and Lung Transplantation (ISHLT), in collaboration with UNOS, created a worldwide registry of all heart and heart-lung transplant procedures in 1982. The Twenty-seventh Report documents that more than 32,000 lung transplant procedures have been performed since that time, with 2769 lung transplant procedures done in 2008 by 158 transplant centers worldwide. Most current transplant procedures involve bilateral sequential or double-lung transplants (Figure 75-2). Seventy-three heart-lung transplant procedures were done during that same year.
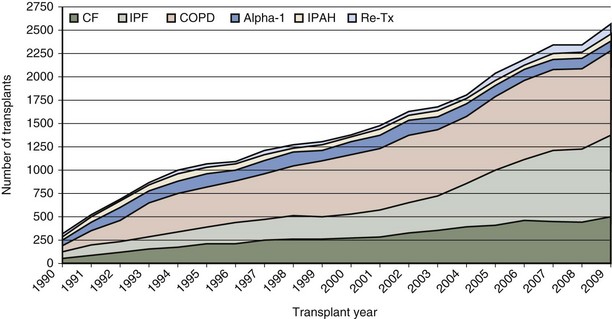
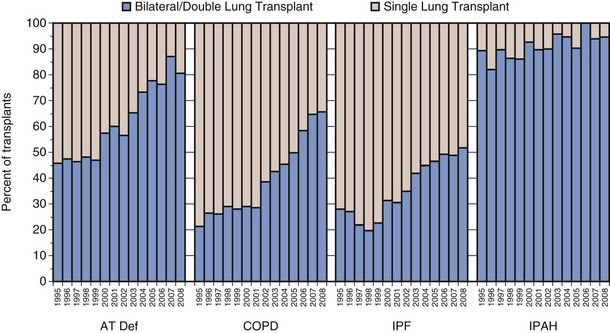
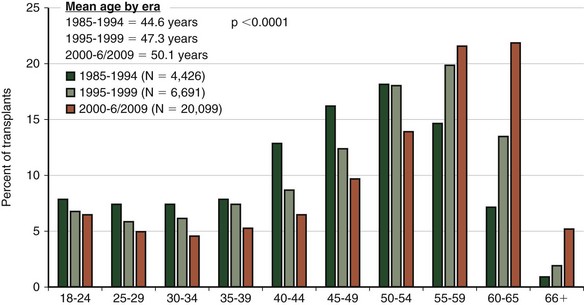
Although the number of lung transplant procedures has increased substantially in the past 2 decades, the leading indications for lung transplantation remain relatively unchanged: chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), cystic fibrosis (CF), α1-antitrypsin (A1A) deficiency with emphysema, and pulmonary arterial hypertension (PAH) (Figure 75-3). The type of transplant a patient receives is dictated in part by the recipient’s underlying disease: Recipients with COPD and IPF tend to receive single-lung as often as double-lung transplants, whereas those with CF and PAH almost always receive bilateral lung transplants (Figure 75-4). Over the past several years, a trend toward performing double-lung transplants and transplanting older people in the 55 to 65 age range has emerged (Figure 75-5).
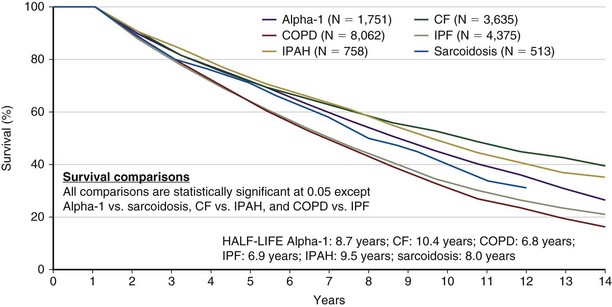
Survival
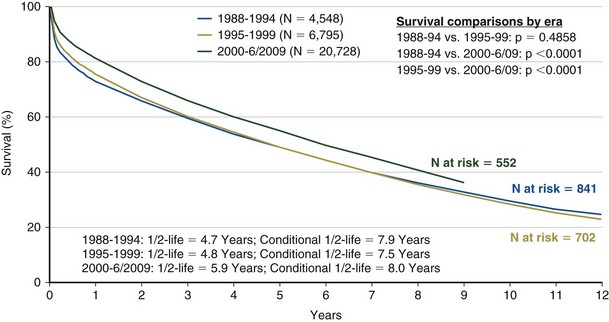
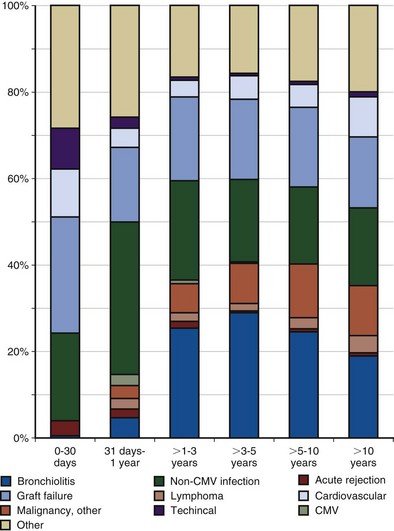
Achieving successful outcomes and maximal survival in the lung transplant population starts with the proper selection of transplant candidates. This entails an understanding of the natural history of the recipient’s lung disease and the projected survival with optimal medical and surgical therapy. Identifying potential candidates must be based on their current quality of life and the potential for improvement with and without transplantation. The median survival for lung transplant recipients has improved dramatically over the past several years. Transplant procedures performed from 2000 to 2004 were associated with a median survival of 5 years, significantly higher than for previous years (Figure 75-6). The survival curve is not linear, however, because approximately 20% of all recipients die in the first year after transplantation, with most occurring in the first 90 days. After this rapid decline, survival then stabilizes and follows a more linear trajectory, with an estimated 6% mortality rate per year. First-year mortality is attributable to postoperative graft complications, infection, cardiac failure, rejection, and early toxicity from immunosuppressive medications (Figure 75-7).
Several independent factors also seem to affect survival, including older age, higher body mass index (BMI), severe pulmonary hypertension, the type of transplant procedure performed, and the recipient’s native pulmonary disease. In recipients older than 65, the expected 5-year median survival is 3.4 years, considerably lower than the overall average 5-year median survival. This is one reason why age older than 65 is considered to be a relative contraindication (Table 75-1).
Table 75-1 General Contraindications to Lung Transplantation
| Absolute | Relative |
|---|---|
BCC, basal cell cancer; BMI, body mass index; HIV, human immunodeficiency virus; SCC, squamous cell cancer.
Modified from Orens JB, Estenne M, Arcasoy SM, et al: International guidelines for the selection of lung transplant candidates: 2006 update—a consensus report from the Pulmonary Scientific Council of the International Society of Heart and Lung Transplantation, J Heart Lung Transplant 25:745–755, 2006.
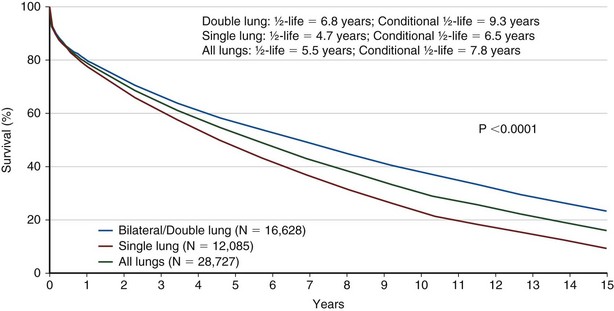
Bilateral lung transplantation (BLTx) is associated with a median survival of 5.6 years, compared with 4.3 years for single lung transplantation (SLTx) (Figure 75-8). Although heart-lung transplantation (HLTx) is associated with the lowest median survival rates of approximately 3 years, HLTx procedures also are the least commonly performed. Although it seems that bilateral lung transplant recipients have a better survival, specifically in the COPD group, this finding is controversial, because the observation is retrospective and uncontrolled. One contributing factor may be that older patients tend to receive single-lung transplants, whereas younger patients receive bilateral lung transplants. The highest survival rates are seen in patients with COPD and CF. The lowest survival rates are seen in patients with IPF and PAH, with a relative risk of death exceeding 2.0 in the first year after transplantation (Figure 75-9).
General Selection Criteria
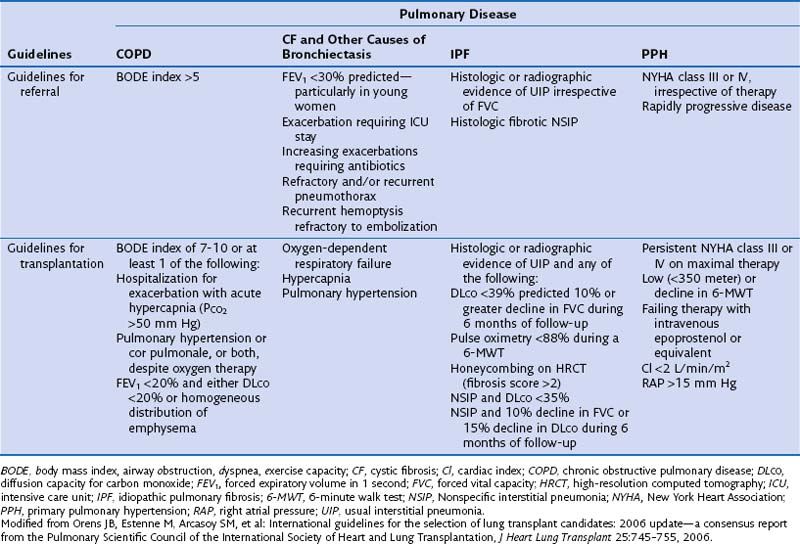
The International Consensus Guidelines for referral and selection of transplant candidates were published in 1998 as a joint effort from the American Society of Transplant Physicians, the American Thoracic Society, the European Respiratory Society, and the International Society for Heart and Lung Transplantation, to facilitate the appropriate timing of referral and proper selection of candidates most likely to benefit from transplantation while ensuring a fair allocation of limited organs. These guidelines were updated in 2006 (Table 75-2). In all instances, selected patients with end-stage pulmonary disease should have declining and irreversible lung function despite optimal medical and surgical management. To justify the risk of transplantation, patients should have an estimated survival of less than 2 years.
Disease-Specific Considerations for Referral and Selection
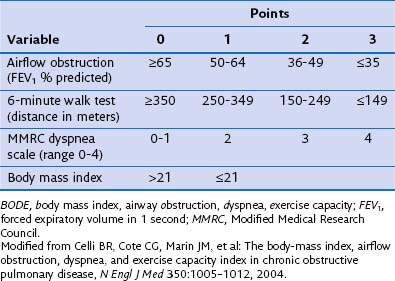
Chronic Obstructive Pulmonary Disease
Survival benefit has not been documented in patients with COPD, even though transplantation confers substantial improvement in functional capacity and quality of life. One potential explanation for this discrepancy is that the forced expiratory volume in 1 second (FEV1) may not be as reliable a referral parameter as, for example, the BODE index (determined by scoring for body mass index, airway obstruction, dyspnea, and exercise capacity) (Table 75-3). Patients with a BODE index between 7 and 10 should be selected for transplantation. Other criteria for selecting candidates with COPD include severe worsening of pulmonary function, shorter 6-minute walking distance capacity (less than 100 yards), weight loss (BMI less than 20 kg/m2), need for hospital admission (to the intensive care unit [ICU] in particular), and radiographically homogeneous emphysema. More severely affected patients will show chronic hypoventilation (i.e., PaCO2 greater than 55 mm Hg and evidence of pulmonary hypertension despite oxygen therapy). All patients with COPD should be referred for pulmonary rehabilitation and treated with oxygen therapy, and use of an alternative approach such as lung volume reduction surgery should be either documented as not a viable option or proved to be ineffective.