Understand the pathogenesis and pathophysiology of normal and abnormal breath sounds.
Understand the pathogenesis and pathophysiology of normal and abnormal breath sounds.
 Recognize the implications of abnormal sounds in individuals with specific lung disease.
Recognize the implications of abnormal sounds in individuals with specific lung disease.
 Formulate a differential diagnoses for the causes of various abnormal lung sounds.
Formulate a differential diagnoses for the causes of various abnormal lung sounds.
ORIGIN OF NORMAL BREATH SOUNDS
Breath sounds result, in large part, from turbulent airflow. Turbulent airflow occurs when the orderly arrangement of particles in laminar flow becomes disrupted. During respiration, this can occur when airflow reaches a critical velocity such as during forced expiration or when airflow is physically disrupted as occurs at airway branch points.
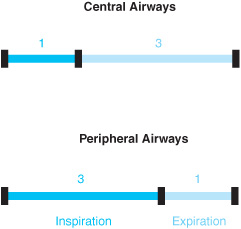
During auscultation, breath sounds are heard best over the trachea and central airways. These sounds, appropriately named tracheal or bronchial breath sounds, consist of high- and low-frequency sounds. In the periphery of the lung, higher pitched components are more attenuated than lower pitched ones, resulting in the muffled quality of normal alveolar breath sounds. Listening to alveolar breath sounds (also called vesicular sounds), the expiratory phase sounds shorter (a 3:1 inspiratory:expiratory ratio) because expiration is a passive process resulting in lower flow rates and less turbulence. The inspiratory:expiratory ratio (1:3) heard over the central airways better approximates the actual time spent in each phase of the respiratory cycle (Figure 5–1).
PATHOPHYSIOLOGY OF ABNORMAL LUNG SOUNDS
Abnormal breath sounds include sounds of differing intensity, duration, or quality when compared to those of the normal respiratory cycle. Qualitative differences in breath sounds are collectively called adventitious breath sounds. The three most common types of adventitious breath sounds are wheezes, rhonchi, and crackles. Other less frequent sounds heard on auscultation are squeaks and a pleural rub.
Figure 5–1. Inspiratory-expiratory ratio during auscultation.
Intensity of Breath Sounds
Care must be taken when assessing the significance of variations in the intensity of lung sounds. Bilateral and unilateral decreases in breath sounds can be of great clinical significance, but some asymmetry of sound intensity is common in normal lungs secondary to minor differences in regional airflow.
 Significant differences in the intensity of breath sounds provide valuable insights into the pathologic state of the lung. In general, sound travels better through liquid than it does through air; thus, pathologic states resulting in increased airway fluid (ie, consolidation by blood, water, or pus) facilitate the transmission of breath sounds (Table 5–1). This means that there is more transmission of sound through a pneumonic than through a normal lung, allowing one to identify areas of consolidation by using physical examination techniques such as egophony (nasal or bleating sound), bronchophony, and whispering pectoriloquy. Egophony, which means “goat sound,” refers to the high-pitched bleating sound “ay” heard over consolidated regions of lung as the patient repeats the sound “ee.” Compared to normal lung, in consolidated regions, a higher pitched sound will be better heard and allows for recognition of a spoken phrase such as “ninety-nine.” This is termed bronchophony. Whispering pectoriloquy involves having the patient whisper a word or phrase that contains several high-pitched components. A useful phrase such as “one, two, three” spoken as a whisper by the patient is heard more loudly by the examiner. Whispering pectoriloquy is also characteristic of a large cavity and may be heard above the level of a pleural effusion.
Significant differences in the intensity of breath sounds provide valuable insights into the pathologic state of the lung. In general, sound travels better through liquid than it does through air; thus, pathologic states resulting in increased airway fluid (ie, consolidation by blood, water, or pus) facilitate the transmission of breath sounds (Table 5–1). This means that there is more transmission of sound through a pneumonic than through a normal lung, allowing one to identify areas of consolidation by using physical examination techniques such as egophony (nasal or bleating sound), bronchophony, and whispering pectoriloquy. Egophony, which means “goat sound,” refers to the high-pitched bleating sound “ay” heard over consolidated regions of lung as the patient repeats the sound “ee.” Compared to normal lung, in consolidated regions, a higher pitched sound will be better heard and allows for recognition of a spoken phrase such as “ninety-nine.” This is termed bronchophony. Whispering pectoriloquy involves having the patient whisper a word or phrase that contains several high-pitched components. A useful phrase such as “one, two, three” spoken as a whisper by the patient is heard more loudly by the examiner. Whispering pectoriloquy is also characteristic of a large cavity and may be heard above the level of a pleural effusion.
Since sound travels less efficiently through air, it makes sense that decreases in the intensity of breath sounds will be detected in diseases characterized by hyper-inflation of the lung (eg, asthma, emphysema, or chronic bronchitis). Importantly, decreases in breath sounds can also result from various other mechanisms (Table 5–1), including failure of air to enter the lungs (airway obstruction) and processes that increase the distance between the lung and chest wall (effusion).
Table 5–1. Changes in the intensity of breath sounds
Increased | Decreased |
Increases in airway fluid | Increased lung volume |
Pneumonia | Hyperinflation |
Pulmonary hemorrhage | Asthma |
ARDS | Emphysema/bullous disease |
Congestive heart failure | Chronic Bronchitis |
Increased air entry/turbulence | Decreased air entry |
Hyperventilation | Hypoventilation |
Mouth breathing | Airway obstruction |
| Phrenic nerve injury |
| Muscle weakness |
| Lung collapse |
| Increased distance of lung from chest wall |
| Obesity |
| Pleural thickening |
| Pneumothorax |
| Empyema |
| Hemothorax |
| Transudative effusion |
Note: ARDS, acute respiratory distress syndrome.
Duration of Breath Sounds
As mentioned in the section on normal breath sounds, the typical inspiratory:expiratory (I:E) ratio heard during auscultation of the peripheral lung is 3:1. Decreases in this ratio can occur in various diseases of the airway (asthma, chronic obstructive pulmonary disease [COPD], or tracheal stenosis) in which the passage of air is obstructed, prolonging expiratory time. This finding is especially pronounced in emphysema, where the loss of alveolar attachments produces much greater expiratory versus inspiratory obstruction (see the flow volume loops in Chapter 1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree