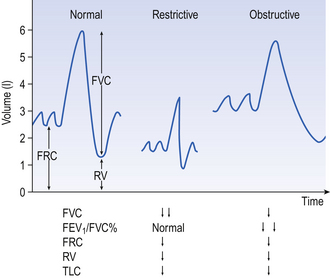
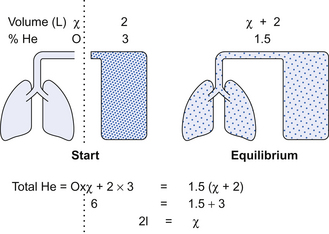
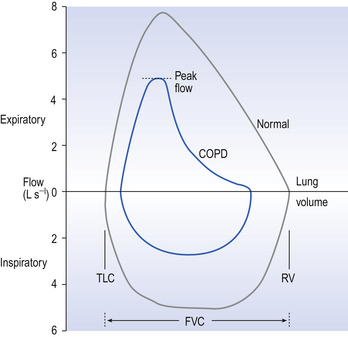
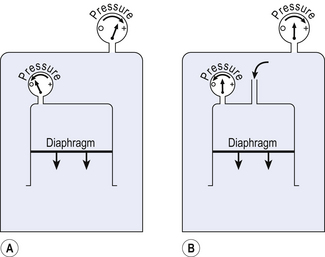
11 A simple spirometer (Fig. 5.2, p. 63) will provide much useful information about a patient’s lungs. Large people have larger lungs than small people and age exerts its malign effect. Extensive study of these relationships has provided us with tables which, for example, relate vital capacity to height (see Appendix). Measurements made on a spirometer may be classified as: • static, where the only consideration is the volume exhaled, or • dynamic, where the time taken to exhale a certain volume is what is being measured. Although such measurements as inspiratory reserve volume (IRV) and expiratory reserve volume (ERV) can be informative, the most usual and useful static spirometric test is the forced vital capacity (FVC). This is ‘forced’ because the subject is enthusiastically urged to breathe in as far as he can and out as far as he can (Fig. 11.1). This test, which can be classed as static because it does not involve an element of time, is often combined with a dynamic test, the FEV1: • Forced expired volume in one second (FEV1). The subject is urged to breathe in as far as he can and breathe out as fast and far as he can. The volume he breathes out in 1 second is the FEV1. Characteristic traces in normals and patients with chronic obstructive (emphyzematous/bronchitic) or restrictive (fibrotic) lung disease are shown in Figure 11.1. • Functional residual capacity (FRC) and residual volume (RV). Because a subject cannot breathe out all the air in his lungs plethysmographic (see below) and dilution methods have to be used to measure these two lung volumes. RV and FRC are frequently increased in diseases such as asthma, bronchitis and emphysema, when airways resistance is increased, and RV is particularly increased in air-trapping emphysema. In the helium dilution method the principle is simple. The patient breathes out to FRC or RV, whichever is being measured, and is connected to a spirometer of known volume containing helium (He) at known concentration. The patient breathes normally for an appropriate length of time and the dilution of the He by the RV or FRC in his lungs is measured. The level of the trace of his breathing is carefully watched and oxygen added at the same rate as it is used up to keep the overall volume in lungs + spirometer constant (Fig. 11.2). Flow-volume loops. With the subject breathing through a pneumotachograph (Fig. 4.6, p. 45) which measures flow, and by integrating that flow to provide volume, loops of inspiratory and expiratory flowvolume relationships can be recorded. (Fig. 11.3). These loops are constructed by having the patient breathe from total lung capacity down to residual volume several times. They are particularly useful in assessing chronic obstructive pulmonary disease (COPD) where the inspiratory part of the loop has a normal shape, although being of reduced volume, while the expiratory part of the loop has a characteristic ‘scooped out’ shape as flow is restricted by airway collapse. This instrument is described in Chapter 4 and consists of an airtight box in which the subject sits. To understand the principles on which this instrument works, consider the subject’s chest as a syringe with the diaphragm represented by the plunger. The subject first pants against a closed shutter – the neck of the syringe is blocked. In terms of gas law the situation is as in Figure 11.4A, where a large enclosed volume of gas (the contents of the box) surrounds a small enclosed volume of gas (the air in the lungs) which increases and decreases in volume as it is compressed or decompressed. This change in volume of the syringe compresses and decompresses the air in the box, and so the pressure in the box changes proportionately and in the opposite sense to the pressure in the lungs. Measuring the pressure changes in the box while the subject pants against a closed shutter enables us to calculate pressure within the lungs (Fig. 11.4) and therefore from the gas laws calculate lung volume, and is usually used to measure functional residual capacity (FRC) and residual volume (RV). Plethysmography is also used to measure lung volumes (TLC) in patients with severe airflow obstruction in preference to the usual helium (He) dilution technique. This is because in these patients air trapping is so bad that the He cannot get to closed off volumes in the lungs, which are therefore not registered. In plethysmography, however, these closed off volumes are still subject to the gas laws (see the Appendix) on which this technique is based. The principle of the relationship between box pressure and lung airway pressure does not depend on the ‘syringe’, which represents the lungs, being closed. In Figure 11.4B
LUNG FUNCTION TESTS
MEASURING DISABILITY
Spirometry
Flow measurements
Plethysmography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine

 inequalities.
inequalities.