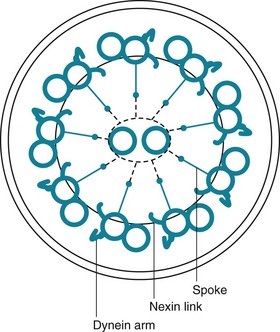
22 Before the discussion of infectious disorders of the respiratory system in Chapters 23 through 26, it is appropriate to first consider how the lung protects itself against the infectious agents to which it is exposed. Although this chapter focuses on protective mechanisms against infection, defenses against noninfectious substances, especially inhaled particulate material, also are addressed. The major categories of defense mechanisms to be discussed include (1) physical or anatomic factors relating to deposition and clearance of inhaled material, (2) antimicrobial peptides, (3) phagocytic and inflammatory cells that interact with the inhaled material, and (4) adaptive immune responses, which depend on prior exposure to and recognition of the foreign material. The chapter concentrates on the aspects of the host defense system specific to the lung and then proceeds with a discussion of several ways the system breaks down, resulting in an inability to handle microorganisms and an increased risk for certain types of respiratory tract infection. The chapter concludes by briefly considering how we can activate or augment specific immune responses through immunization, thus enhancing defenses against selected respiratory pathogens. The term mucociliary transport or mucociliary clearance refers to a process of waves of beating cilia moving a blanket of mucus (and any material trapped within the mucus) progressively upward along the tracheobronchial tree. From the trachea down to the respiratory bronchioles, the most superficial layer of epithelial cells lining the airway has cilia projecting into the airway lumen. These cilia have a structure identical to that of cilia found elsewhere in the body, consisting of longitudinal microtubules with a characteristic architecture. Specifically, a cross-sectional view of cilia shows two central microtubules surrounded by nine pairs of microtubules arranged around the periphery (Fig. 22-1). Small projecting side arms from each doublet, called dynein arms, are crucial to the contractile function of the microtubules and hence to the beating of the cilia. The sol layer contains a number of substances that are important in innate immunity. The innate immune system can be thought of as a fast-acting system that is ready to quickly protect the lungs without prior sensitization and ideally avoid activation of the adaptive immune system (discussed in the Adaptive Immune Responses section). In addition to mucociliary clearance, the innate immune system is composed of small molecules, proteins, and cells that are able to respond to inhaled particles in a way that does not require any previous exposure to the particle. These molecules are generally highly conserved in evolution and are present in many invertebrate species as well as in humans. They are able to immediately interact with microorganisms through recognition of conserved structures on the microbes, and they can act directly to kill the invader and stimulate a further host immune response. They provide a fast, energy-efficient, effective frontline defense, with broad overlap in actions. There are many components of innate immunity in the lung, and a full description is beyond the scope of this chapter. The interested reader is referred to the in-depth reviews listed in the references. For the reader to get a sense of the system, this chapter focuses on a few of the best described of these molecules: lysozyme, lactoferrin, defensins, collectins (surfactant protein A [SP-A] and surfactant protein D [SP-D]), and immunoglobulin (Ig)A. Respiratory IgA can be considered part of the innate immune system because it is also constitutively produced by the respiratory epithelium and does not require prior exposure. IgA is further discussed in the section on humoral immune mechanisms.
Lung Defense Mechanisms
Physical or Anatomic Factors
Antimicrobial Peptides
Lung Defense Mechanisms