Chapter 10
Lower Limb Ulceration
Huw O.B. Davies and J. Mark Scriven
Heart of England NHS FT, Birmingham, UK
Introduction
One percent of the general population suffers from lower limb ulceration and this prevalence increases with age (3% of over 65-year-olds are affected). The management of leg ulcers often involves frequent visits to care providers (community nurses, tissue viability specialists, podiatrists, secondary care nurses, general practitioners, diabetologists, dermatologists, plastic surgeons and vascular surgeons) and non-healing ulceration increases the risk of lower limb amputation. Thus, chronic persistence and frequent ulcer recurrence places a large financial burden upon the NHS (estimated at £400–600 million annually). There is also a significant effect on patients’ quality of life: ulcers can be painful, malodorous and may necessitate prolonged bandage treatment. As a result, patients can feel stigmatised and become socially isolated.
Table 10.1 details the causes of leg ulceration, the most common of which is vascular insufficiency. Venous ulceration accounts for over 75% of cases, the remaining aetiologies comprising arterial disease (2%), arteriovenous disease (12%) and the remaining due to other pathologies as described later. As the aetiology of lower limb ulceration spans a range of pathologies and thus will present in varying guises to primary care, such a structured, evidence-based approach to management is imperative. However, once an initial assessment and diagnosis has been made, most leg ulcers can subsequently be managed in a primary care setting.
Table 10.1 Causes of lower limb ulceration.
“Vascular”
|
Neuropathy
|
| Trauma/factitious |
| Malignancy |
|
| Underlying osteomyelitis |
| Immobility/obesity |
| Lymphoedema |
| Steroid medication |
Blood dyscrasias
|
Skin conditions
|
Infection
|
Nutritional deficiency
|
Lower limb ulceration clinical assessment
Assessment of the underlying cause of ulceration is the key to ongoing management; this will direct treatment of both the primary ulcer and the underlying pathology. Box 10.1 outlines a pragmatic management pathway for patients presenting with lower limb ulceration. This combined with clinical assessment allows appropriate investigation and referral to specialist care.
Clinical history
Assessment of a patient’s ulcer begins with a thorough history. Location, size, duration, pain and recurrence will guide the clinician towards a diagnosis. Co-morbid conditions should also be enquired about—diabetes, peripheral vascular disease, autoimmune disease, inflammatory bowel disease and connective tissue disorders as well as medication should be recorded. Previous arterial or venous interventions may give a clue to aetiology. Although eliciting a history of varicose veins is important, it is worth remembering that a proportion of patients with significant venous reflux have no varicosities apparent on clinical examination.
Social factors may also contribute to lower limb ulceration. Smoking is a known cause of peripheral vascular disease. Occupation may also contribute—particularly those who stand for long periods of the working day. Elderly people with decreased mobility possibly to the extent of spending most of the day sitting in a chair with oedematous dependent legs will have reduced calf muscle pump function and be at risk of ulceration. Muscle pump stasis also occurs as a result of morbid obesity that has a bearing when treatment options are considered.
Poorly controlled diabetes not only causes neuropathy but also an increased prevalence of lower limb infection and poor wound healing.
Physical examination
Evaluation of the venous and arterial systems will commonly yield a cause for ulceration. It is therefore important to examine both of these systems thoroughly followed by a detailed assessment of the skin and ulcer. Absence of arterial or venous signs may indicate a rarer cause for ulceration and careful consideration regarding biopsy should be made.
Venous assessment
Evaluate both limbs for signs of chronic venous insufficiency (CVI). These include prominent varicose or reticular veins, brawny skin and venous eczema. Haemosiderin deposition and lipodermatosclerosis should also be noted.
Arterial assessment
Again both limbs should be assessed for the presence or absence of palpable lower limb pulses. Trophic changes associated with chronic arterial insufficiency may be present (pale, shiny skin that is often hairless).
The ankle-brachial pressure index (ABPI) should be measured to assess the degree of any underlying arterial pathology. Care should be taken in interpretation of results in diabetics who may have falsely elevated readings due to vessel calcification. An ABPI > 0.8 excludes a significant ischaemic component and would permit the safe use of compression bandages or hosiery if required to treat venous hypertension. If arterial disease is significant, then further imaging with a view to revascularisation would be indicated.
Ulcer assessment
Location is particularly helpful to determining the underlying cause but bear in mind that an atypical presentation of common ulcers does occur. Size should also be noted (it may be helpful to use serial measurement to assess response to treatment) and the ulcer’s shape and sides should be noted along with the appearance of the base. The clinician should assess for superimposed infection (possibly requiring treatment with antibiotics or debridement) by examining surrounding skin also, compression of surrounding tissues may produce pus and any sinus tracks should be explored by probing with bacteriology swabs. Table 10.2 details some common features of ulcer types.
Table 10.2 Ulcer characteristics.
| Ulcer type | Location | Appearance | Associated features |
| Venous | Gaiter area (above malleoli) | Sloping edge Granulating base Exudate/slough | Haemosiderin skin changes Lipodermatosclerosis |
| Arterial | Anterior leg (shin) Over malleoli Under heel Over toe joints | Punched-out edge Grey/pale base with little granulation Typically painful | History of severe ischaemia |
| Neuropathic | Over malleoli Under heel Over toe joints Under metatarsal heads Medial aspect of first metatarsal head (bunion area) | Punched out Surrounding callus | Diabetes Sinus formation Underlying osteomyelitis Charcot deformity Impaired sensation |
Investigations
Duplex ultrasonography is a cheap non-invasive method of assessing arterial and venous disease that is available in most vascular surgical clinics. It is the gold standard modality for deep and superficial venous assessment. Ultrasonographers are also able to assess arterial disease and identify flow-limiting stenoses and occlusions.
Computed tomography (CT) angiography is a widely available method of visualising peripheral arterial disease. Modern scanners are able to use low doses of contrast to image the entire vascular tree. It is limited in assessment of venous disease as it is unable to measure reflux but CT can be useful for determining causes of proximal venous obstruction (such as pelvic masses and central vein occlusion).
Magnetic resonance imaging (MRI) is an excellent method of arterial imaging and does not require the administration of contrast; however, it is of limited use in venous disease. It is more time consuming and requires greater technical expertise to produce high-quality images and is thus more expensive. MRI is especially useful to examine for evidence of osteomyelitis/deep sepsis in diabetic foot ulcer disease.
Digital subtraction angiography can be used to accurately image arterial pathology and simultaneously treat arterial stenoses and occlusions. However, it is invasive and associated with radiation exposure, risks of arterial injury/thrombosis and contrast nephropathy.
In addition to vascular investigations, haematology and standard biochemical investigations are useful as well as testing for auto-antibodies and acute and chronic markers of inflammation if an autoimmune or vasculitic aetiology is suspected.
The importance of histological examination by way of an ulcer edge biopsy cannot be ignored for ‘atypical’ ulcers, recalcitrant lesions and where the diagnosis remains unclear after excluding venous/arterial/diabetic aetiologies. This is a simple procedure requiring simple equipment and a local anaesthetic. Either a punch biopsy can be taken or a larger ellipse of tissue including normal skin, ulcer edge and ulcer base.
Arterial ulceration
Arterial ulcers may occur in any position on the leg (Figure 10.1). They are more common over bony prominences often related to local pressure effects. Arterial ulcers have a ‘punched-out’ appearance with straight sides to the ulcer edge. The base of the ulcer often appears sloughy, pale and devitalised having little or poor granulation tissue present. They often have little wound exudate and can be dry and necrotic. Infection is a common associated feature. They are often deeper than venous ulcers and involve underlying structures such as tendon or bone. The ulcer itself is usually painful. This pain is particularly noted at night or on elevation of the affected limb and is improved by placing the limb in a dependant position.
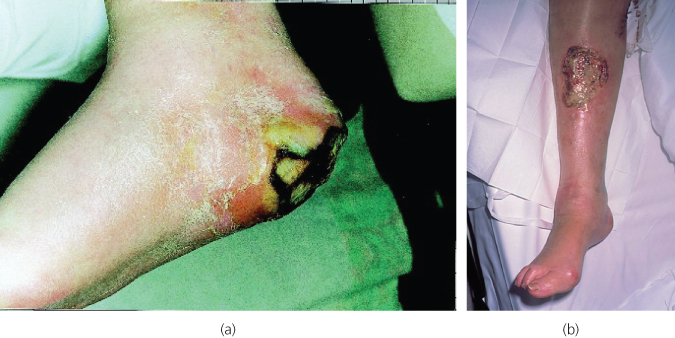
Figure 10.1 Arterial ulcers involving heel (a) and shin (b). Note associated necrosis and absence of venous skin changes.
Arterial revascularisation is the treatment for arterial ulcers. This may involve an angioplasty-based procedure. Bypass grafting in the presence of tissue loss runs a higher than average risk of serious surgical site or graft infection.
Dressings are important. Typically, these are occlusive—to allow a suitable, moist microenvironment for the growth of new tissue. They also allow the control of exudate and encourage epithelial cell migration generating an environment rich in leucocytes helping to control infection. There is also evidence that pain and pruritis are decreased by this dressing type. There is extensive current research into ‘smart’ active dressings that utilise nanotechonology to deliver substances such as growth factors to increase rates of healing or interact with tissue proteases to encourage epithelia activity.
Those wounds that are actively infected or carry a heavy slough load will benefit from one of the various debridement treatments available (larvae, hydrocolloid dressings, mechanical ward-based treatments or surgery). Antibacterial dressings (silver and iodine) also have a role in some instances.
Neuropathic ulceration
Neuropathy causes the loss of protective sensation and coordination of muscle groups in the foot and leg. This predisposes patients to unnoticed injuries and structural foot deformities all of which worsen repetitive stress at pressure points leading to tissue breakdown.
Diabetes is the most common cause for neuropathic ulceration, which commonly occurs on the soles of the feet particularly under the metatarsal heads (Figure 10.2). They are typically painless and are usually surrounded by callosities. The presence of sinus tracks should increase suspicion that underlying tissue and bone may be infected. Imaging with X-ray or MRI can identify underling osteomyelitis.

Figure 10.2 Typical neuropathic ulceration over metatarsal head on the sole of a diabetic patient’s foot.
Often diabetic neuropathic ulcers have a degree of arterial insufficiency that also needs addressing. Only then should callus and necrotic tissue be debrided either with dressings or surgically (it is often possible to carry out extensive debridement under only local anaesthetic because of the degree of sensory neuropathy). Any active infection should be treated to minimise the extent of possible tissue loss. The ulcerated area should then be protected with off-loading footwear or a windowed plaster cast while healing takes place.
Patients with neuropathic ulcers or feet at risk of developing diabetic ulcers should be managed along the lines of the National Service Framework for Diabetes in specialist facilities with multidisciplinary team input.
Venous ulceration
Venous hypertension is the commonest cause of leg ulceration in the Western world. This condition alone places a significant burden on NHS resources, especially considering the plethora of community-based dressings and bandages used as well as nursing time required. While community-based management based on effective compression therapy has been the traditional method of treatment, clinical trials are currently assessing the efficacy of more interventional approaches. It is important to recognise that because venous disease is so common (up to 50% of the population), it is not unusual for venous ulcers to develop in association with other contributory factors such as arterial disease and diabetes.
Venous ulcers classically develop in the medial gaiter region above the ankle usually in association with the clinical features of underlying CVI (Figure 10.3) and sometimes visible varicose veins. However, they can also be found laterally located or atypically on the foot (Figure 10.4). Patients often describe having had ulceration for protracted periods of time, sometimes decades, and a pattern of intermittent healing and recurrence is common. The clinical appearance is characterised by a superficial defect with sloping edges and florid, friable granulation tissue in the base. Venous ulcers are often associated with variable levels of slough formation and can exude large volumes of fluid. This fluid loss is often difficult to control and may cause secondary damage to surrounding skin due to the maceration that can occur. Traditionally, ulceration has been considered a consequence of previous deep vein thrombosis but assessment with duplex ultrasound scanning demonstrates that over 60% of the patients with venous ulcers have isolated superficial reflux in isolation with normal deep veins and only 1 in 10 limbs demonstrate evidence of post-thrombotic deep vein changes.

Figure 10.3 Typical skin changes of chronic venous insufficiency demonstrating haemosiderin pigmentation, ‘inverted champagne bottle legs’ and bilateral ulceration over the medial gaiter region.

Figure 10.4 Atypical location of a venous ulcer; illustrating the requirement for full clinical assessment of lower limb ulceration to direct appropriate treatment.
Community-based compression therapy is the cornerstone treatment modality in the United Kingdom. A systematic review and meta-analysis in 2009 demonstrated that four-layer bandaging increased the chances of ulcer healing by 30% compared with short-stretch bandaging. Previous studies have demonstrated the efficacy of superficial venous surgery in achieving ulcer healing. Prevention of recurrence of venous ulceration can be significantly enhanced by correction of superficial venous reflux in combination with compression (ESCHAR study). Currently, newer modalities of superficial venous treatment (ultrasound-guided foam sclerotherapy and thermal endovenous ablation) are being evaluated to test the efficacy of compression alone versus compression plus endovenous ablation of superficial reflux. To this end, the results of the EVRA (early venous reflux ablation) ulcer trial are awaited.
For the majority of patients with venous ulceration, appropriate investigation and treatment can result in a healed limb; however, ulcer recurrence remains a problem and the prevention of recurrence remains an important aspect of ulcer management. Below knee class II compression hosiery (which delivers 18–24 mmHg pressure at the ankle) is effective in preventing re-ulceration in compliant patients. Many patients with venous ulcers are elderly, arthritic and find donning and doffing hosiery difficult. In these circumstances, class I (14–17 mmHg) may be a pragmatic compromise or alternative stockings with zip fasteners/wrap around designs may be more appropriate.
Timely vascular surgical referral for formal assessment of ulcers is recommended. The Venous Forum of the Royal Society of Medicine recommends that all breaks in the skin below the knee of more than 2-week duration be referred urgently to a vascular surgical department. However, despite timely and appropriate treatment, there remains a small proportion of patients (approximately 10%) with venous leg ulcers that remain unhealed after several years of treatment.
Arteriovenous ulceration
Up to 20% of leg ulcers develop as a result of combined arterial (ABPI < 0.8) and venous insufficiency (duplex evidence of venous reflux). This group of patients can be challenging as standard compression bandages are not suitable in the presence of arterial disease. Modified or reduced compression can be used with ABPI > 0.7 but in most cases correction of the arterial disease is required. This will allow the safe application of effective compression or treatment of superficial venous reflux.
Other conditions to consider
While most patients presenting with lower limb ulceration will have either venous, arterial, mixed or neuropathic ulcers occasionally, less common causes of ulceration occur (Table 10.1). These alternative diagnoses are important to make so that appropriate management can be instituted. The clinical history and examination will often alert the clinician to less typical forms of ulceration, especially if further assessment excludes arterial or venous disease. Basal cell (Figure 10.5) and squamous carcinoma are commonly confirmed on biopsy of the ulcer edge. Figure 10.6 demonstrates a thigh ulcer in an Asian patient with cutaneous TB. Patients whose ulcers develop without any obvious aetiology need careful assessment for underlying vasculitis, blood dyscrasias, rheumatoid disease, etc. before being labelled as factitious.
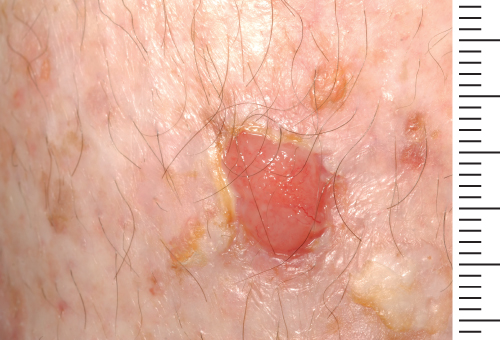
Figure 10.5 Pretibial basal cell carcinoma. Consideration of malignant lesions requires a high degree of suspicion. This lesion had shown some signs of reduction in size with community-based compression bandaging but does not demonstrate the expected features of underlying CVI.

Figure 10.6 Atypical tuberculous thigh ulcer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


