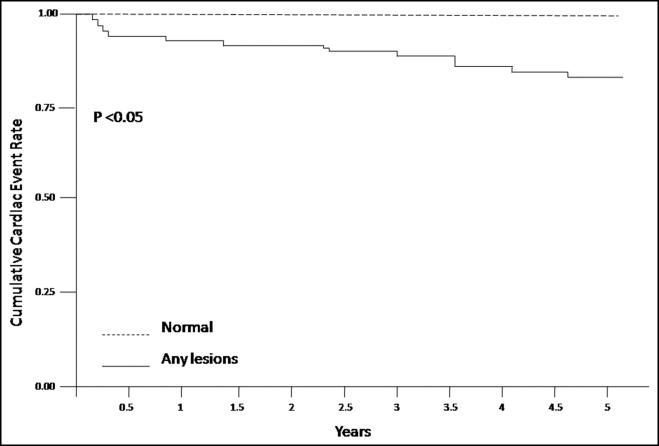
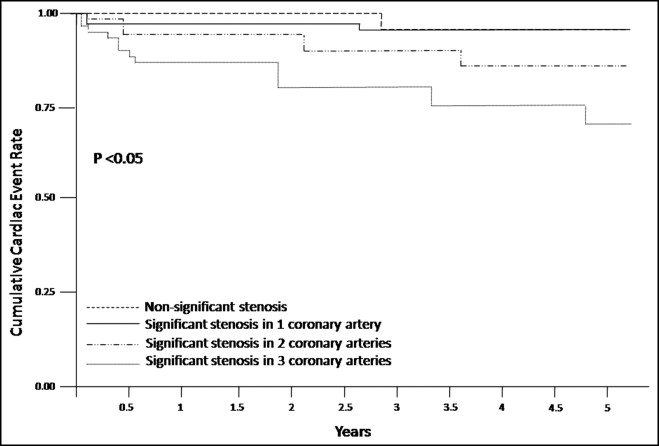
A paucity of data on outcome of coronary multislice computed tomography (CT) is available. The aim of this study was to assess the long-term follow-up of 64-slice CT in a homogenous patient group. In total 222 patients (136 men, 61%, 59 ± 11 years of age) with chest pain at intermediate risk of coronary artery disease (CAD) and no previous CAD underwent 64-slice CT. Coronary lesions were considered significant or not based on a threshold of 50% luminal narrowing. Plaques were classified as calcified, noncalcified, and mixed based on type. End point during follow-up was major adverse cardiac events (nonfatal myocardial infarction, unstable angina requiring hospitalization, myocardial revascularization). Coronary plaques were detected in 162 patients (73%). Coronary artery stenosis was significant in 62 patients. Normal arteries were found in 59 patients (27%). During a mean follow-up of 5 ± 0.5 years, 30 cardiac events occurred. Annualized event rates were 0% in patients with normal coronary arteries, 1.2% in patients with nonsignificant stenosis, and 4.2% in patients with significant stenosis (p <0.01). Predictors of cardiac events were presence of significant stenosis, proximal stenosis, and multivessel disease. Noncalcified and mixed plaques had the worse prognosis (p <0.05). In conclusion, 64-CT provides long-term incremental value in patients at intermediate risk of CAD.
Coronary multislice computed tomography (CT) is increasingly being used as a tool for noninvasive visualization of coronary arteries. The technique provides information on atherosclerotic plaque burden and to some extent on plaque composition. Accuracy of coronary CT needs to be assessed in management outcome studies in which diagnostic and therapeutic strategies would be decided based on CT alone, without reference to any coronary angiographic results. Therefore, the purpose of the present study was to explore extent, degree, and structure/function of coronary atherosclerosis by 64-CT in a homogenous patient population with chest pain, intermediate probability of coronary artery disease (CAD), and no previous cardiac events and to analyze the impact of these variables on long-term follow-up.
Methods
The study group was composed of 222 consecutive patients (136 men, 61%, mean age 59 ± 11 years) who underwent 64-CT at the Cardiothoracic Centre of Monaco, Monte Carlo from January to October 2005. All patients included in the study presented with chest pain suspicious for angina. A subgroup of patients had previous equivocal stress test results. Eligibility criteria for this study were suspected but no previously known CAD and intermediate pretest likelihood of CAD (score 9 to 15 points) according to a modification of a method by Diamond and Forrester as published by Morise et al. Exclusion criteria for recruitment were previous documented CAD, history of percutaneous transluminal coronary angioplasty or coronary artery bypass grafting, nonchest pain indication for CT, and low and high pretest likelihoods of CAD. A structured interview and clinical history were obtained, and the following cardiac risk factors were assessed before CT: (1) hypertension (defined as blood pressure ≥140/90 mm Hg or use of antihypertensive agents), (2) hyperlipidemia as defined by low-density lipoprotein cholesterol >140 mg/dl, (3) diabetes mellitus (defined as fasting glucose level >120 mg/dl or need for insulin or oral antidiabetic medicines), (4) smoking (current or previous habit), (5) body mass index, (6) family history of CAD in first-degree relatives, and (7) medication use. All patients gave written informed consent to the study protocol, which was approved by the local ethics committee. All scans were performed with a 64-slice computed tomographic scanner that features a temporal resolution time of 165 ms and a spatial resolution of 0.4 mm 3 (Siemens Somatom Sensation 64 Cardiac, Siemens, Forchheim, Germany). If heart rate was ≥65 beats/min, additional β blockers (metoprolol 5 mg intravenously to a maximum dose of 10 mg) were provided. Nitroglycerin (0.4 mg sublingually) was used in all studies unless contraindicated. Patients with known allergy to iodine, significant arrhythmia (atrial fibrillation and frequent premature beats) or rapid heart rate (90 beats/min), impaired renal function (serum creatinine ≥1.3 mg/dl), and contraindications to β blockade were not imaged. The following parameters were applied for CT: collimation of 64 × 0.6 mm, tube rotation time of 330 ms, and tube current of 450 mA at 120 kV. Nonionic contrast material was administered in the antecubital vein at 80 to 105 ml, depending on total scan time, and a flow rate of 5 ml/s (Iodixanol 320, GE Healthcare SA, Velizy-Villacoublay, France and Iomeron 400, Bracco Imaging, Courcouronnes, Evry cedex, France) followed by a saline flush of 50 ml at a flow rate of 5 ml/s. The bolus-tracking technique was used to synchronize the arrival of contrast in coronary arteries and initiation of the scan. Automated detection of peak increase in the aortic root was used for timing of the scan. All images were acquired during an inspiratory breath-hold of approximately 10 seconds, with simultaneous registration of a patient’s electrocardiogram. To evaluate presence of coronary artery plaques, reconstructions in diastole (typically 75% of cardiac cycle) were generated with a slice thickness of 0.75 mm at an increment of 0.6 mm. If motion artifacts were present, additional reconstructions were made at different time points of the RR interval. Axial datasets were transferred to a remote workstation (Syngo, Siemens, Berlin, Germany) for postprocessing and subsequent evaluation. Radiation dose-decreasing techniques, i.e., dose modulation along the z-axis and pulsing algorithm along the RR interval, were employed for all scans. All studies were analyzed by 2 experienced readers blinded to all clinical variables, history, and patient demographics. Coronary arteries were divided into 17 segments according to the modified American Heart Association classification. Only segments with a diameter ≥1.5 mm were included. Each segment was classified as interpretable or not. Patients were excluded from analysis for (1) an uninterpretable proximal or midsegment or (2) >3 uninterpretable segments in general. Then, interpretable segments were evaluated for presence of any atherosclerotic plaque using axial images and multiplanar reconstructions. After visual inspection of volume-rendered images, which depicted the gross coronary artery luminal configuration, coronary artery plaques were carefully inspected on axial images, curved multiplanar reformatted images, and cross-sectional multiplanar reformatted images. Coronary plaques were defined as structures >1 mm 2 within and/or adjacent to the coronary artery lumen, which could be clearly distinguished from the vessel lumen and the surrounding pericardial tissue, epicardial fat, or the vessel lumen itself. One coronary plaque was assigned per coronary segment. An assessment of plaque composition was also allowed. Differentiation was made among noncalcified plaques (composed exclusively of material having density <130 HU), calcified plaques (composed exclusively of high-density material >130 HU), and mixed plaques (having components of noncalcified and calcified material). Atherosclerotic lesion was deemed significant if diameter stenosis was ≥50%. Lesions below this threshold were considered nonsignificant or mild. For each patient, number of diseased coronary segments, number of segments with significant stenosis, and number of each type of plaque was calculated. Computed tomograms without coronary lesions were considered normal; computed tomograms showing coronary wall irregularities or ≥1 coronary plaque (significant or not) were defined as abnormal. Significant coronary stenosis were further classified as localized in 1 epicardial artery or 2 or 3 epicardial arteries (left anterior descending, left circumflex, right coronary arteries) and significant plaques in the left main and/or proximal left anterior descending coronary artery. Follow-up information was obtained by clinical visits, telephone contact, or questionnaires sent by mail. All reported events were verified by hospital records or direct contacts with the attending physician. The following clinical events were recorded: (1) cardiac death (including death without definitive cause), (2) nonfatal acute myocardial infarction (AMI), (3) unstable angina pectoris requiring hospitalization, and (4) coronary revascularization (by coronary angioplasty or bypass). Coronary revascularization occurring soon after CT was performed as a consequence of its result. Therefore, patients undergoing coronary revascularization procedures sooner than 90 days after CT were excluded from further analysis. The end point of this study was major adverse cardiac events including nonfatal AMI, unstable angina pectoris requiring hospitalization, and revascularization. Definitions of AMI and unstable angina were previously described. For multiple events in a given patient, the first was the event included in the analysis. All patients were followed for a mean period of 5.0 ± 0.5 years (maximum follow-up period 5.5 years).
Analyses were performed with SAS 9.1.3 (SAS Institute, Cary, North Carolina). All continuous data are presented as mean ± SD, and all categorical data are reported as percentage or absolute number. A p value <0.05 was considered statistically significant. In univariate analysis, unpaired Student’s t tests or chi-square tests were used to assess differences between groups. Kaplan-Meier survival curves were constructed for computed tomographically diagnosed CAD and were compared with log-rank test. Effect of CAD on hard cardiac events at CT was determined using Cox proportional hazard model. After adjustment for all baseline clinical characteristics, a forward stepwise model was used to determine independent predictors of coronary atherosclerotic variables on computed tomogram (p <0.05). Hazard ratios and confidence intervals were calculated.
Results
Of the 246 patients included in the study, 13 were excluded from analysis because of poor image quality related to cardiac motion artifact and respiratory motion artifact; 11 patients declined to participate in the follow-up study and 30 patients were lost during 5-year follow-up. Replies were obtained from 192 patients (follow-up rate 87%). All patients presented with chest pain suspicious for angina. A smaller subset of patients (83, 37%) initially underwent stress testing with equivocal findings and continued symptoms that warranted further evaluation. A complete overview of baseline characteristics of the entire study population is presented in Table 1 . Based on coronary computed tomographic results, the study population was divided into 3 subgroups: patients with normal arteries (59, 27%), patients with nonsignificant stenosis (101, 45%), and patients with significant stenosis (62, 28%). A correlation between clinical risk factors and occurrence and grade of stenosis is presented in Table 1 . As presented, significant stenosis occurred more frequently in patients who were older, had hypertension, and a smoking habit (p <0.05). Computed tomographic characteristics are listed in Table 2 . After exclusion of 45 inaccessible segments (1.2%) because of motion artifacts, plaque burden was evaluated in 3,729 segments. According to plaque texture, 28 (45%) were from patients with obstructive calcified plaques, 16 (26%) were from those with obstructive mixed plaques, and 14 (23%) were from those with obstructive noncalcified plaques. A combination of different significant plaques (calcified and/or noncalcified and/or mixed plaques) was found in 4 patients (6%). Patients with significant calcified plaques were on average significantly older then patients with significant noncalcified and mixed plaques (63 ± 8.2 vs 61 ± 7.1, p <0.01) and more frequently affected by hypertension (18 vs 10, p <0.05).
| Variable | Total | Normal Arteries | Nonsignificant Stenosis | Significant Stenosis | p Value |
|---|---|---|---|---|---|
| (n = 59) | (n = 101) | (n = 62) | |||
| Age (years) | 59.2 ± 10.8 | 53.1 ± 11.2 | 60.6 ± 9.8 | 62.7 ± 9.7 | <0.001 |
| Men | 136 (61%) | 33 (55%) | 62 (61%) | 41 (67%) | 0.39 |
| Hypertension | 91 (41%) | 16 (27%) | 42 (42%) | 33 (53%) | 0.016 |
| Diabetes mellitus | 38 (17%) | 6 (10%) | 19 (19%) | 13 (21%) | 0.27 |
| Hyperlipidemia ⁎ | 78 (35%) | 18 (30%) | 36 (36%) | 24 (39%) | 0.58 |
| Smoker | 49 (22%) | 6 (10%) | 27 (27%) | 16 (26%) | 0.056 |
| Body mass index >30 kg/m 2 | 51 (23%) | 9 (15%) | 25 (25%) | 17 (27%) | 0.32 |
| Normal coronary circulation | 59 (27%) |
| Coronary stenosis <50% | 101 (45%) |
| Coronary stenosis ≥50% | 62 (28%) |
| Plaques in left main/proximal left anterior descending coronary artery | 67 (9%) |
| Plaques in all left anterior descending coronary artery | 280 (39%) |
| Plaques in left circumflex coronary artery | 172 (24%) |
| Plaques in right coronary artery | 199 (28%) |
| Number of coronary arteries narrowed ≥50% | |
| 1 | 43 (19.4%) |
| 2 | 21 (9.5%) |
| 3 | 21 (9.5%) |
| Total number of segments with plaques | 718 (19.2%) |
| Total plaque score | 3.2 |
| Calcified plaque (significant or not) | 374 (52%) |
| Mixed plaque (significant or not) | 273 (33%) |
| Noncalcified plaque (significant or not) | 109 (15%) |
Prognostic analysis was performed in 192 patients. In these patients, 30 major cardiac events occurred (total event rate 15.6%). Nonfatal AMI affected 2 patients (1%) and unstable angina 14 patients (7.3%); coronary revascularization was performed in 14 patients (7.3%, 11 with angioplasty and 3 with bypass). No cases of cardiac deaths were recorded. Annual cardiac event rates were 4.2% in patients with significant stenosis, 1.2% in patients with nonsignificant stenosis, and 0% in patients with normal arteries on 64-slice computed tomogram ( Figures 1 and 2 ). Patients with cardiac events were significantly older. Univariate analysis is presented in Table 3 . Predictors of all cardiac events are presented in Table 4 . Any obstructive plaque, multivessel distribution, proximal stenosis, and noncalcified and mixed plaques had the worse prognosis ( Figures 1 to 3 ) .

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


