Assessing the efficacy of implantable cardioverter-defibrillators (ICD) in patients with Chagas’ heart disease (ChHD) and identifying the clinical predictors of mortality and ICD shock during long-term follow-up. ChHD is associated with ventricular tachyarrhythmias and an increased risk of sudden cardiac death. Although ChHD is a common form of cardiomyopathy in Latin American ICD users, little is known about its efficacy in the treatment of this population. The study cohort included 116 consecutive patients with ChHD and an ICD implanted for secondary prevention. Of the 116 patients, 83 (72%) were men; the mean age was 54 ± 10.7 years. Several clinical variables were tested in a multivariate Cox model for predicting long-term mortality. The average follow-up was 45 ± 32 months. New York Heart Association class I-II developed in 83% of patients. The mean left ventricular ejection fraction was 42 ± 16% at implantation. Of the 116 patients, 58 (50%) had appropriate shocks and 13 (11%) had inappropriate therapy. A total of 31 patients died (7.1% annual mortality rate). New York Heart Association class III (hazard ratio [HR] 3.09, 95% confidence interval 1.37 to 6.96, p = 0.0064) was a predictor of a worse prognosis. The left ventricular ejection fraction (HR 0.972, 95% confidence interval 0.94 to 0.99, p = 0.0442) and low cumulative right ventricular pacing (HR 0.23, 95% confidence interval 0.11 to 0.49, p = 0.0001) were predictors of better survival. The left ventricular diastolic diameter was an independent predictor of appropriate shock (HR 1.032, 95% confidence interval 1.004 to 1.060, p = 0.025). In conclusion, in a long-term follow-up, ICD efficacy for secondary sudden cardiac death prevention in patients with ChHD was marked by a favorable annual rate of all-cause mortality (7.1%); 50% of the cohort received appropriate shock therapy. New York Heart Association class III and left ventricular ejection fraction were independent predictors of worse prognosis, and low cumulative right ventricular pacing defined better survival.
Data are conflicting regarding the efficacy of implantable cardioverter-defibrillator (ICD) in patients with Chagas’ heart disease (ChHD). The evidence is based on the results of 2 manufacturer-sponsored registries and 1 retrospective cohort study. The reported annual mortality rates in these 3 studies varied from 5.5% to 16.6%, with the upper value greater than the mortality rates reported in studies restricted to patients with sustained ventricular tachycardia (VT) who were treated with antiarrhythmic drugs. Thus, the aim of the present study was to assess, during long-term follow-up, the ICD efficacy of a ChHD cohort from a tertiary center, considering all-cause mortality and appropriate ICD shock therapy rates and analyzing the predictive value of the clinical variables.
Methods
The inclusion criteria were ChHD, diagnosed by positive serologic tests, and an ICD implanted for secondary prevention of sudden cardiac death, according to the Brazilian guidelines. The exclusion criteria were age <18 years old, advanced atrioventricular block, or previous pacemaker or cardiac resynchronization device at ICD implantation (n = 76 patients). The study flow chart is shown in Figure 1 .
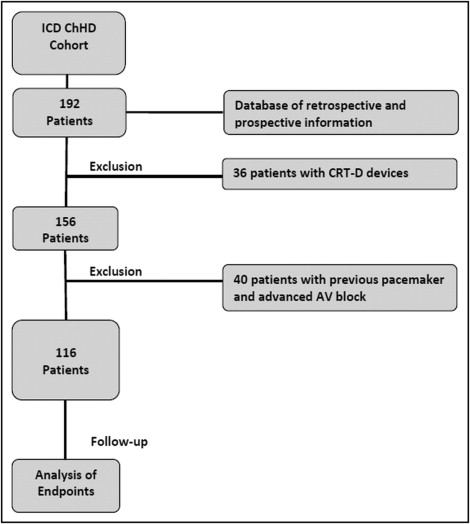
The present study was a retrospective cohort study of patients with ChHD and an ICD from the Heart Institute of the University of São Paulo Medical School (InCor) in Brazil. The ethics committee of our institution approved the study in January 2000 and the study was implemented in June 2000. The last inclusion occurred in June 2008, and follow-up was closed in March 2009. A database system was designed to include patient characteristics, medical history, ICD indication, and functional outcomes at implantation and during follow-up. The data were collected on several potential risk factors, including age, gender, New York Heart Association functional class, syncope, left ventricular ejection fraction (LVEF), the use of drugs (amiodarone, β blockers, angiotensin-converting enzyme inhibitors), echocardiographic parameters (LVEF, left ventricular diastolic diameter, left atrial diameter, and mitral regurgitation), the percentage of cumulative right ventricular pacing, and the occurrence of appropriate and inappropriate shock therapy. Radiofrequency catheter ablation was undertaken on a case-by-case basis.
Before ICD implantation, all patients received optimal medical therapy. The ICD implants included 114 transvenous systems, manufactured by Medtronic (Minneapolis, Minnesota) (33%), Biotronik (Berlin, Germany) (25%), Guidant/CPI (St. Paul, Minnesota) (10%), and St. Jude Medical (Sylmar, California) (32%). The ICD programming included therapy for standard VT with antitachycardia pacing combined with low-energy shock therapy and for ventricular fibrillation (VF)—shock therapy with a 300-ms cutoff cycle interval. It was considered standard VT in the presence of sustained tachycardia with a cycle interval ranging from 300 to 400 ms, not discriminated as supra-VT by specific algorithms. It was considered VF when the cycle interval was inferior to 300 ms. ICD therapy was classified as appropriate for VT/VF if the recorded intracardiac electrogram for the intervention was compatible with the clinical manifestation, on medical discretion. The shock therapy was considered inappropriate when the ICD therapy was applied to supra-VT, noise, myopotential oversensing, or R-wave double counting. Customized programs were performed according to individual needs. The decision regarding activation of pacing therapy for bradycardia was left to the discretion of each physician at the outpatient pacemaker clinic.
The follow-up protocol included regular clinical and device evaluation performed 3 times annually.
The primary outcome was death from all causes. The circumstances of the deaths were reviewed and categorized as from a cardiac or noncardiac cause, and the classification of Hinkle and Thaler was used to evaluate the suspected mechanism of death.
The primary data analysis examined the effect of the potential risk factors on appropriate shocks and long-term mortality. Cumulative survival was assessed using the Cox regression method adjusted for independent covariates, and the differences were compared using Cox proportional hazard models. Analyses, adjusted for potential confounders, were also performed using multivariate Cox proportional hazard models. The covariates were applied in a forward selection according to the unadjusted association of p <0.05 in the univariate models. The Cox model assumption of proportional hazards was found to be valid from the log-minus-log curves and the Schoenfeld test. The software used was SPSS, version 16.0.1, for Windows (SPSS, Chicago, Illinois).
Results
The study cohort consisted of 116 patients. Of the 116 patients, 73 were men. The patient age range was 18 to 79 years (mean 54 ± 10.7 years). New York Heart Association functional class I-II was present in 82.7%, and the mean LVEF was 42.4 ± 15.7%. Of the 116 patients, 90 (77.6%) were taking a median daily dose of 400 mg (range 100 to 600) amiodarone, and 38 (32.8%) were using a β blocker. The ICD indication was resuscitated VF or VT in 21 patients (18.1%) and symptomatic sustained VT in 95 (81.9%). Of these, 64 patients (55.2%) underwent an electrophysiologic study and had hemodynamic unstable VT or VF induced by <3 extra stimuli. ICD implantation was performed from June 1990 to June 2008. The baseline clinical characteristics of the cohort are listed in Table 1 .
| Characteristics at implantation | Value |
|---|---|
| Men | 73 (62%) |
| Mean age (years) | 54.0 ± 10.7 |
| New York Heart Association functional class | |
| I | 36 (31%) |
| II | 60 (52%) |
| III | 20 (17%) |
| Syncope | 73 (63%) |
| Mean left ventricular ejection fraction (%) | 42.4 ± 15.7 |
| Left atrium (mm) | 41.2 ± 6.7 |
| Left ventricular end-diastolic diameter (mm) | 63.3 ± 9.2 |
| Amiodarone | 90 (78%) |
| Median daily dose (mg) | 400 |
| β Blocker | 38 (33%) |
| Angiotensin-converting enzyme inhibitors | 95 (82%) |
| Electrophysiologic study | 79 (68.1%) |
| Not induced | 3 (4%) |
| Monomorphic ventricular tachycardia | 1 (1%) |
| Monomorphic sustained ventricular tachycardia | 61 (77%) |
| Polymorphic sustained ventricular tachycardia | 11 (14%) |
| Ventricular fibrillation | 3 (4%) |
| Mean QRS width (ms) | 125.6 |
| Nonsustained ventricular tachycardia | 59 (66%) |
| Sustained ventricular tachycardia | 3 (3%) |
| Implantable cardioverter-defibrillator indication | |
| Aborted sudden cardiac death | 21 (18%) |
| Symptomatic sustained ventricular tachycardia | 95 (82%) |
| Type of implantable cardioverter-defibrillator | |
| Atrioventricular | 67 (58%) |
| Ventricular | 49 (42%) |
| Median percentage of cumulative right ventricular pacing | 17% |
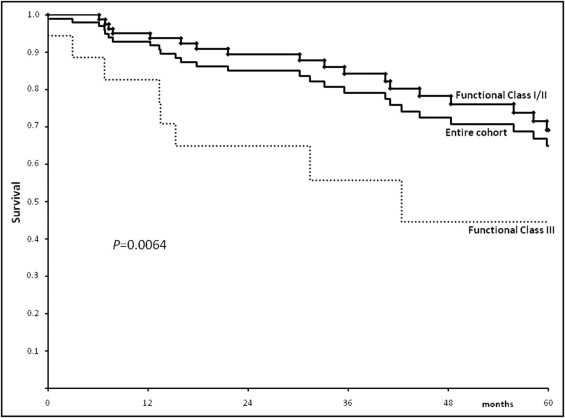
During a mean follow-up of 45 ± 32 months, 31 deaths (26.7%) occurred ( Table 2 ), corresponding to an annual mortality rate of 7.1%. The potential confounder variables applicable to the multivariate Cox proportional hazards models (those associated with death on univariate analysis, p <0.05) were New York Heart Association functional class, the use of amiodarone, LVEF, left ventricular end-diastolic diameter, left atrial diameter, nonsustained VT, rate of cumulative right ventricular pacing, and number of appropriate shocks. New York Heart Association functional class III (hazard ratio [HR] 3.09, 95% confidence interval [CI] 1.37 to 6.96, p = 0.0064) was a predictor of a worse prognosis. The LVEF (HR 0.972, 95% CI 0.94 to 0.99, p = 0.0442) and a low rate of cumulative right ventricular pacing (HR 0.23, 95% CI 0.11 to 0.49, p = 0.0001) were predictors of better survival.
| Cause | Patients (n) |
|---|---|
| Unknown | 3 (8%) |
| Cardiac | |
| Heart failure | 14 (45%) |
| Sudden death | 0 |
| Non cardiac | 14 (45%) |
| Total | 31 |
The survival curves of the entire cohort, stratified according to New York Heart Association functional class and cumulative right ventricular pacing, are presented in Figures 2 and 3 . Survival curves free of appropriate shock therapy, including the survival curve for the entire cohort, are presented in Figure 4 .