The aim of this study was to examine long-term compliance with nonpharmacologic treatment of patients with heart failure (HF) and its associated variables. Data from 648 hospitalized patients with HF (mean age 69 ± 12 years, 38% women, mean left ventricular ejection fraction 33 ± 14%) were analyzed. Compliance was assessed by means of self-report at baseline and 1, 6, 12, and 18 months after discharge. Patients completed questionnaires on depressive symptoms, HF knowledge, and physical functioning at baseline. Logistic regression analyses were performed to examine independent associations with low long-term compliance. From baseline to 18-month follow-up, long-term compliance with diet and fluid restriction ranged from 77% to 91% and from 72% to 89%, respectively. In contrast, compliance with daily weighing (34% to 85%) and exercise (48% to 64%) was lower. Patients who were in New York Heart Association functional class II were more often noncompliant with fluid restriction (odds ratio [OR] 1.97, 95% confidence interval [CI] 1.25 to 3.08). A lower level of knowledge on HF was independently associated with low compliance with fluid restriction (OR 0.78, 95% CI 0.71 to 0.86) and daily weighing (OR 0.86, 95% CI 0.79 to 0.94). Educational support improved compliance with these recommendations. Female gender (OR 1.91, 95% CI 1.26 to 2.90), left ventricular ejection fraction ≥40% (OR 1.55, 95% CI 1.03 to 2.34), a history of stroke (OR 3.55, 95% CI 1.54 to 8.16), and less physical functioning (OR 0.99, 95% CI 0.98 to 0.99) were associated with low compliance with exercise. In conclusion, long-term compliance with exercise and daily weighing was lower than long-term compliance with advice on diet and fluid restriction. Although knowledge on HF and being offered educational support positively affected compliance with weighing and fluid restriction, these variables were not related to compliance with exercise. Therefore, new approaches to help patients with HF stay physically active are needed.
Although it has been well established, most studies on determinants of compliance in patients with heart failure (HF) have been cross-sectional or have focused solely on compliance with 1 specific nonpharmacologic recommendation. Data on temporal trends in compliance with cardiovascular medication have been reported previously, but little is known about long-term compliance with nonpharmacologic treatment (i.e., sodium-restricted diet, fluid restriction, daily weighing, and exercise) and its determinants. Noncompliance with nonpharmacologic treatment is related to adverse outcomes and lower quality of life. It is therefore vital to identify those patients who are at risk for noncompliance over a longer period, especially considering that studies have shown that noncompliance is a problem in the HF population. It has been suggested that compliance with a specific recommendation might be a marker for compliance with other recommendations or lifestyle changes. Unfortunately, direct comparisons of compliance with different recommendations in the same study population are not available. In the present study, we aimed to address this gap by examining long-term compliance with nonpharmacologic recommendations and by assessing variables associated with long-term compliance.
Methods
We used a descriptive, prospective design with data from the Coordinating Study Evaluating Outcomes of Advising and Counseling in Heart Failure (COACH) study. COACH was a randomized, multicenter, controlled study in which 1,023 patients with HF were included from November 2002 to February 2005. Inclusion criteria were an admission for HF, evidence of a structural underlying heart disease, and age ≥18 years. Exclusion criteria were participation in another study, a planned or recent invasive cardiac intervention, or inability to complete questionnaires. COACH was designed to evaluate the effect of education and counseling by an HF nurse on clinical outcomes in patients with HF. Patients were randomized to either a control group (care as usual, with routine management by a cardiologist) or to 1 of the intervention groups (basic support or intensive support). Along with routine management by a cardiologist, patients in the 2 intervention groups received additional care from an HF nurse. This additional care was provided during hospitalization and after discharge according to protocol and consisted of comprehensive education and counseling about HF and the HF regimen. Patients in the intensive group had more contact moments with the HF nurse, including ≥1 home visit. Multidisciplinary advice was also part of the intensive intervention.
The study complied with the Declaration of Helsinki, and the medical ethics committee granted approval for the protocol. All patients provided written informed consent and were enrolled and examined during a fixed period of 18 months after discharge from the hospital. Assessments, conducted by an independent data collector, took place at index hospitalization (baseline) and 1, 6, 12, and 18 months after discharge (follow-up) at patients’ homes. Patients completed questionnaires on compliance, HF knowledge, and quality of life. The presence of depressive symptoms was assessed at baseline and 12 and 18 months after discharge. When patients were not able to complete the questionnaires themselves, the data collector guided the patients through the questionnaires by reading them the questions. At baseline, clinical variables were retrieved from the patients’ medical records and by means of structured interviews. Data on left ventricular function were obtained using standard transthoracic echocardiography. Patients were included in this study on long-term compliance when they completed the compliance questionnaire during ≥4 of 5 assessment moments. Only 1 missing value on each separate recommendation was permitted. When patients had 1 missing value on a specific recommendation during the total follow-up period, this missing value was substituted by the lowest compliance score for that specific recommendation on all other assessments.
The Center for Epidemiologic Studies Depression Scale was used to measure the presence of depressive symptoms. This scale consists of 20 items and measures the presence of depressive feelings and behaviors. A score of ≥16 indicates the presence of depressive symptoms. To differentiate between patients with moderate or severe depressive symptoms, the following cut-off scores were used: 0 to 15 (no depressive symptoms), 16 to 23 (moderate depressive symptoms), and ≥24 (severe depressive symptoms).
Compliance with recommendations on a sodium-restricted diet, fluid restriction, exercise, and daily weighing was measured using the Revised Heart Failure Compliance Scale. Compliance was measured on a 5-point scale (0 = never, 1 = seldom, 2 = half of the time, 3 = mostly, 4 = always). Two HF nurses, experienced in the field of compliance, assessed face validity of the Dutch version of the scale. Patients were defined as compliant with diet, fluid restriction, or exercise when they followed the recommendations always or mostly during the previous week. They were compliant with weighing when they weighed daily or ≥3 times a week during the previous month. When a patient reported compliance with a specific recommendation, a score of 1 point was assigned. Because compliance was measured at 5 different assessment moments (baseline and at 1, 6, 12, and 18 months during follow-up), the compliance score for each recommendation could range from 0 to 5 points. This long-term compliance score was categorized as either low or high, with a score ≤3 defined as low long-term compliance. High long-term compliance indicated compliance at 4 or all 5 assessment moments.
HF knowledge was measured with the Dutch Heart Failure Knowledge Scale, which consists of 15 multiple-choice items (range 0 to 15), with higher scores indicating higher levels of HF knowledge. This scale is a reliable and valid instrument for measuring knowledge of HF in general, symptom recognition, and the HF regimen.
Perceived health and physical functioning were assessed using the RAND-36, a self-report questionnaire of general health status similar to the Medical Outcomes Study 36-item General Health Survey. Patients were asked to score their general health on a 5-point scale (1 = excellent, 5 = bad). Next, patients were divided into 2 groups: those who perceived their general health as good to excellent and those who perceived it as fair to bad. The subscale “physical functioning” consists of 10 items on limitations experienced when performing daily physical activities due to health problems. The total score of the subscale ranges from 0 to 100, with higher scores indicating better functioning.
Descriptive statistics were used to characterize the study population and to examine long-term compliance with the recommendations. For this study, data from the COACH study were used. Compliance with each recommendation was therefore also described separately for patients in the control group and for patients who were assigned to 1 of the intervention groups. Because examining differences in compliance between the 2 intervention groups was not the main focus of the present study, data were pooled for the 2 intervention groups and compared with the control group. To assess which baseline variables were independently associated with low long-term compliance, logistic regression analyses were performed. Low long-term compliance was used as the dependent variable; an odds ratio >1 indicates a higher probability of being low long-term compliant, whereas an odds ratio <1 indicates a lower probability of being low long-term compliant. First, univariate regression analyses were performed to explore which baseline variables were individually associated with low long-term compliance. All theoretically relevant variables for which the Wald test of no association with low long-term compliance had p values <0.10 were subsequently inserted in a multivariate regression model to determine whether these variables were also independently associated with low long-term compliance. This procedure was conducted for all 4 recommendations. SPSS version 16.0 (SPSS, Inc., Chicago, Illinois) was used to perform the statistical analyses.
Results
Of the 1,023 patients participating in COACH, 648 were included in this substudy. A total of 375 (1,023–648) patients were excluded: 272 patients died during the follow-up period of 18 months, and 103 patients did not complete the compliance questionnaires on ≥4 assessment moments or had >1 missing value on a specific recommendation. Compared to included patients, excluded patients were significantly older (74 vs 69 years, p <0.001), more often lived alone (44% vs 36%, p = 0.015), were more often in New York Heart Association (NYHA) functional class III or IV at discharge (58% vs 44%, p <0.001), and more often had an ischemic origin of HF (48% vs 39%, p = 0.008).
The baseline characteristics of the study population are listed in Table 1 . The mean age of the study population (n = 648) was 69 ± 12 years, 38% were women, and 44% were in NYHA class III or IV at discharge, with a mean left ventricular ejection fraction (LVEF) of 33 ± 14% ( Table 1 ). The mean length of HF symptoms was 26 ± 48 months. Of all patients, 18% had moderate and 20% had severe depressive symptoms. In total, 31% of the patients were in the “care as usual” group, and 69% were in 1 of the 2 intervention groups.
| Variable | Value |
|---|---|
| Age (years) | 69 ± 12 |
| Women | 244 (38%) |
| Living alone | 233 (36%) |
| Educational level (high) | 74 (11%) |
| Left ventricular ejection fraction (%) | 33 ± 14% |
| Left ventricular ejection fraction ≥40% | 187 (32%) |
| NYHA class III or IV at discharge | 281 (44%) |
| Ischemic origin of HF | 255 (39%) |
| Length of HF (months) | 26.3 ± 48.3 |
| Previous HF admission | 183 (28%) |
| Depressive symptoms | |
| Moderate | 112 (18%) |
| Severe | 120 (20%) |
| Diabetes mellitus | 153 (24%) |
| Chronic obstructive pulmonary disease | 160 (25%) |
| Stroke | 49 (8%) |
| RAND-36 score | |
| Perceived health, fair to bad | 400 (64%) |
| Physical functioning | 39 ± 27 |
| Dutch Heart Failure Knowledge Scale total score | 11.3 ± 2.3 |
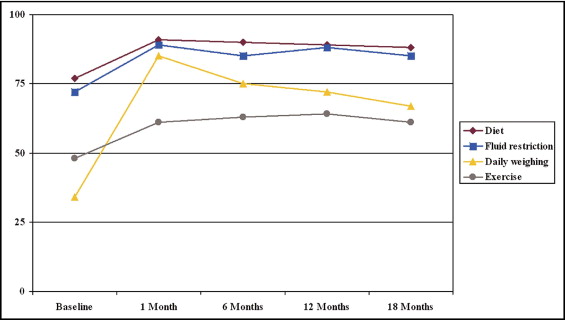
Compliance with daily weighing (ranging from 34% to 85% at the 5 assessment moments) and compliance with exercise (range 48% to 64%) was lower compared to compliance with a sodium-restricted diet (range 77% to 91%) and fluid restriction (range 72% to 89%) ( Figure 1 ) . Compliance with diet at 1 month after discharge from the index hospitalization increased from 77% to 91% and remained stable afterward. A similar trend was found for compliance with fluid restriction. Compliance with daily weighing increased from 34% to 85% at 1 month but decreased over time to 67% at 18 months. Although compliance with exercise increased at 1 month, it remained at about 60% during follow-up ( Figure 1 ). Compliance was also examined separately for patients in the control group and for patients in the intervention groups. In the 2 groups, percentages of compliance were also lower for daily weighing and exercise compared to diet and fluid restriction. Compliance with fluid restriction, particularly daily weighing, was higher in the intervention groups ( Figures 2 and 3 ) .
Subsequently, low long-term compliance (defined as being compliant at ≤3 of 5 assessment points during baseline and follow-up) with each separate recommendation was examined. Of all patients, 16% demonstrated low compliance in the long term with a sodium-restricted diet and 21% with fluid restriction. In contrast, 41% and 54%, respectively, showed low compliance with daily weighing and exercise. Of all patients who showed low compliance with diet (n = 104), 54% showed low compliance with fluid restriction, 61% with daily weighing, and 82% with exercise. These percentages indicate that low compliance with 1 recommendation does not automatically indicate low compliance with other recommendations in the long term. Similar results were found for low long-term compliance with fluid restriction, weighing, and exercise ( Table 2 ).
| Diet | Fluid Restriction | Daily Weighing | Exercise | |
|---|---|---|---|---|
| Diet (n = 104) | 54% (n = 56) | 61% (n = 63) | 82% (n = 85) | |
| Fluid restriction (n = 138) | 41% (n = 56) | 65% (n = 89) | 79% (n = 109) | |
| Daily weighing (n = 267) | 24% (n = 63) | 33% (n = 89) | 69% (n = 184) | |
| Exercise (n = 352) | 24% (n = 85) | 31% (n = 109) | 52% (n = 184) |
In a multivariate analysis, being in NYHA class II was independently associated with low compliance with fluid restriction. Having more knowledge about HF and being assigned to basic or intensive support were inversely associated with low compliance with fluid restriction and also with low compliance with daily weighing. This indicates that patients with more knowledge or patients who received additional support were more often compliant over a longer period. Women and patients with LVEFs ≥40% were more likely to have low compliance with exercise. In addition, a history of stroke and poor physical functioning due to health problems were associated with low long-term compliance with exercise. No significant associations in univariate or in multivariate analyses were found between compliance with a sodium-restricted diet and possible relevant variables ( Table 3 ).
| Variable | Unadjusted OR (95% CI) | p Value | Unadjusted OR (95% CI) | p Value | Nagelkerke r 2 | C-Statistic |
|---|---|---|---|---|---|---|
| Low compliance, sodium restriction | 0.019 | 0.582 | ||||
| Chronic obstructive pulmonary disease | 0.59 (0.34–1.02) | 0.06 | 0.60 (0.35–1.03) | 0.06 | ||
| Basic/intensive support | 0.66 (0.43–1.02) | 0.06 | 0.66 (0.42–1.03) | 0.07 | ||
| Low compliance, fluid restriction | 0.137 | 0.685 | ||||
| Left ventricular ejection fraction ≥40% | 1.54 (1.02–2.32) | 0.038 | 1.19 (0.76–1.86) | 0.44 | ||
| NYHA class II | 1.68 (1.13–2.50) | 0.010 | 1.97 (1.25–3.08) | 0.003 | ||
| Stroke | 2.10 (1.13–3.91) | 0.019 | 1.57 (0.77–3.21) | 0.22 | ||
| HF knowledge | 0.77 (0.71–0.84) | <0.001 | 0.78 (0.71–0.86) | <0.001 | ||
| Basic/intervention support | 0.47 (0.32–0.69) | <0.001 | 0.50 (0.32–0.77) | 0.002 | ||
| Low compliance, daily weighing | 0.150 | 0.688 | ||||
| Age | 1.03 (1.01–1.04) | <0.001 | 1.01 (0.99–1.03) | 0.19 | ||
| Living alone | 1.49 (1.07–2.06) | 0.017 | 1.26 (0.86–1.83) | 0.24 | ||
| Educational level (high) | 0.61 (0.36–1.03) | 0.06 | 0.81 (0.45–1.44) | 0.47 | ||
| Left ventricular ejection fraction ≥40% | 1.77 (1.25–2.52) | 0.001 | 1.44 (0.98–2.11) | 0.06 | ||
| HF knowledge | 0.85 (0.79–0.91) | <0.001 | 0.86 (0.79–0.94) | 0.001 | ||
| Basic/intervention support | 0.32 (0.23–0.45) | <0.001 | 0.32 (0.21–0.46) | <0.001 | ||
| Low compliance, exercise | 0.180 | 0.716 | ||||
| Age | 1.03 (1.01–1.04) | <0.001 | 1.02 (0.99–1.04) | 0.06 | ||
| Female gender | 1.83 (1.32–2.53) | <0.001 | 1.91 (1.26–2.90) | 0.002 | ||
| Living alone | 1.36 (0.98–1.88) | 0.07 | 0.82 (0.54–1.24) | 0.34 | ||
| Left ventricular ejection fraction ≥40% | 1.57 (1.10–2.23) | 0.013 | 1.55 (1.03–2.34) | 0.036 | ||
| NYHA class II | 0.63 (0.46–0.86) | 0.004 | 0.90 (0.60–1.35) | 0.61 | ||
| Previous HF admission | 1.35 (0.95–1.90) | 0.09 | 1.30 (0.83–2.03) | 0.25 | ||
| Diabetes mellitus | 1.41 (0.98–2.04) | 0.07 | 1.09 (0.69–1.73) | 0.72 | ||
| Stroke | 3.56 (1.75–7.27) | <0.001 | 3.55 (1.54–8.16) | 0.003 | ||
| Depressive symptoms | ||||||
| None | 1.00 (reference) | 1.00 (reference) | ||||
| Moderate | 1.80 (1.16–2.77) | 0.008 | 1.47 (0.88–2.46) | 0.14 | ||
| Severe | 1.73 (1.14–2.63) | 0.011 | 1.04 (0.61–1.75) | 0.89 | ||
| Total HF symptoms | 1.10 (1.02–1.17) | 0.010 | 1.01 (0.92–1.11) | 0.78 | ||
| Perceived health fair to bad | 1.93 (1.39–2.68) | <0.001 | 1.28 (0.84–1.94) | 0.25 | ||
| Physical functioning | 0.98 (0.98–0.99) | <0.001 | 0.99 (0.98–0.99) | 0.006 | ||
| HF knowledge | 0.86 (0.80–0.93) | <0.001 | 0.93 (0.85–1.02) | 0.14 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


